Cytoskeletal Defects in Neurodegeneration: Mechanisms, Therapeutic Targeting, and Future Directions
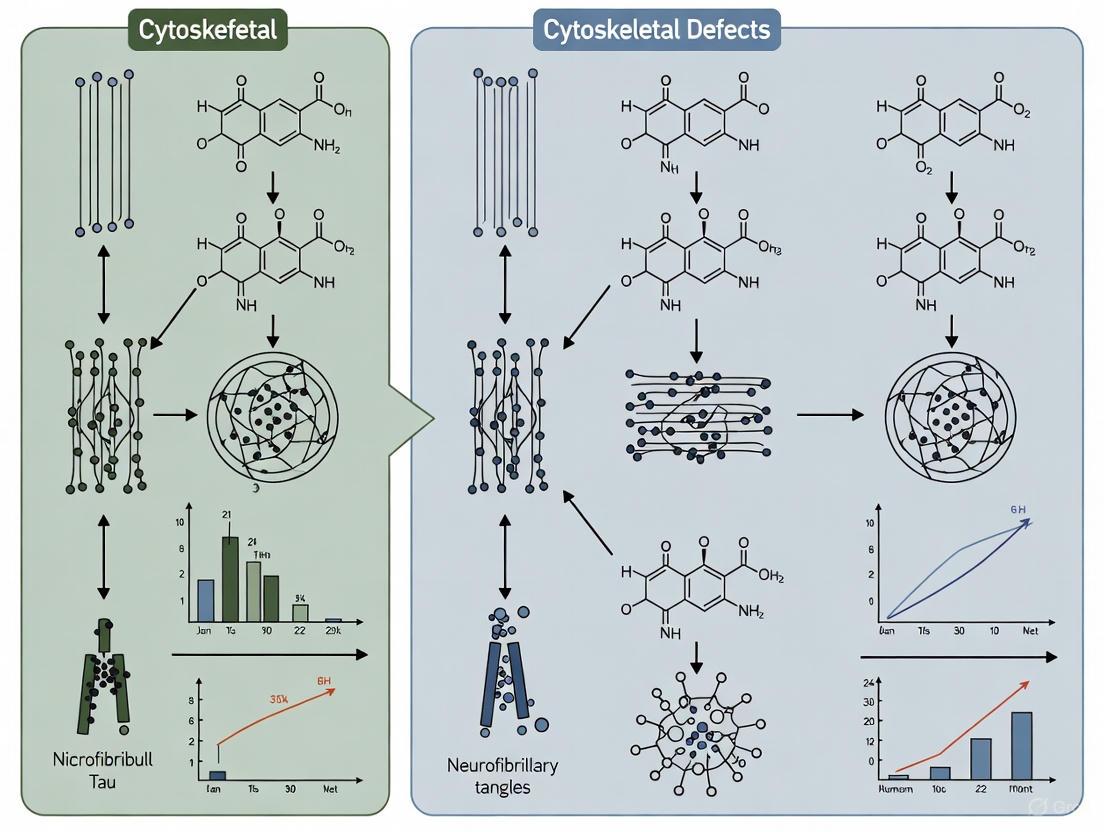
This article synthesizes current knowledge on cytoskeletal dysfunction as a central mechanism in neurodegenerative diseases, including Alzheimer's disease, Parkinson's disease, Amyotrophic Lateral Sclerosis, and Huntington's disease.
Cytoskeletal Defects in Neurodegeneration: Mechanisms, Therapeutic Targeting, and Future Directions
Abstract
This article synthesizes current knowledge on cytoskeletal dysfunction as a central mechanism in neurodegenerative diseases, including Alzheimer's disease, Parkinson's disease, Amyotrophic Lateral Sclerosis, and Huntington's disease. We explore how defects in microtubules, neurofilaments, and actin filaments disrupt axonal transport, mitochondrial function, and neuronal integrity. For researchers and drug development professionals, this review examines emerging therapeutic strategies targeting cytoskeletal pathways, discusses methodological approaches and associated challenges, and evaluates cytoskeletal biomarkers for disease monitoring and therapeutic validation. The integration of foundational science with translational applications provides a comprehensive framework for developing novel interventions against these devastating disorders.
The Neuronal Cytoskeleton: Architecture and Core Pathologies in Neurodegeneration
The neuronal cytoskeleton, a complex and dynamic network, is fundamental to maintaining cellular structure, facilitating intracellular transport, and enabling neuronal plasticity. Comprised primarily of microtubules, neurofilaments, and actin filaments, this integrated system ensures proper neuronal function and viability. Increasing evidence indicates that defects in these cytoskeletal components and their regulatory mechanisms constitute a primary pathological feature in numerous neurodegenerative diseases. This whitepaper provides an in-depth technical analysis of the structure, function, and dynamics of these core filaments, frames their integrity within the context of neurodegeneration research, and presents current methodologies for investigating cytoskeletal defects. Understanding these mechanisms is crucial for developing novel biomarkers and therapeutic strategies aimed at preserving neuronal health in conditions such as Alzheimer's disease, Parkinson's disease, and amyotrophic lateral sclerosis.
The cytoskeleton is an essential, dynamic network of filamentous proteins that extends throughout the cell cytoplasm, providing mechanical support, organizing intracellular contents, and facilitating crucial processes like cell division, motility, and intracellular transport [1] [2]. In neurons, the cytoskeleton takes on additional, specialized responsibilities due to the cells' extreme polarity and unique architectural demands. The elongated axons and complex dendrites of neurons, which can span remarkable distances, require a robust and adaptable internal scaffold to maintain their shape, resist mechanical stress, and enable the efficient transport of cargo between the cell body and distant synaptic terminals [3].
This neuronal scaffold is composed of three primary polymeric structures, classified by their diameter and biochemical composition: microtubules (~25 nm), neurofilaments (~10 nm), and actin filaments (~7 nm) [1] [2] [3]. Unlike static girders, these filaments form a dynamic system that is constantly being remodeled through assembly and disassembly, and their functions are finely tuned by a vast array of associated proteins, molecular motors, and post-translational modifications [4]. The coordinated interplay between these three systems allows the neuron to construct, maintain, and adapt its complex morphology over a lifetime.
The critical importance of the cytoskeleton for neuronal health is underscored by the fact that its collapse is a common hallmark of neurodegenerative diseases [3]. Defects in axonal transport, alterations in filament dynamics, and the accumulation of filamentous aggregates are observed in conditions including Alzheimer's disease (AD), Parkinson's disease (PD), amyotrophic lateral sclerosis (ALS), and spinal muscular atrophy (SMA) [5] [3]. The resulting failure to transmit information and essential cargoes between the cell body and synapses triggers a "dying-back" degeneration of the neuron [3]. Consequently, the cytoskeleton is not merely a structural element but a central player in neurodegeneration, making its components prime targets for diagnostic and therapeutic intervention.
Core Components: Structure, Function, and Dynamics
Microtubules
Structure and Composition: Microtubules are the largest of the cytoskeletal filaments, with a diameter of approximately 25 nm [1] [6]. They are hollow cylinders composed of 13 linear protofilaments, each of which is a polymer of alternating α-tubulin and β-tubulin heterodimers [6]. This structure exhibits an inherent polarity, with a fast-growing plus end (exposed β-tubulin) and a slow-growing minus end (exposed α-tubulin) [6]. The minus end is typically anchored at the microtubule-organizing center (MTOC), while the plus end extends into the cellular periphery, a configuration critical for directional transport [6].
Dynamic Instability and Regulation: A defining characteristic of microtubules is dynamic instability, the stochastic switching between phases of growth and shrinkage [6]. This process is governed by GTP hydrolysis; the addition of GTP-bound tubulin stabilizes the growing end, while hydrolysis to GDP destabilizes the lattice, leading to rapid depolymerization (a "catastrophe") [6]. In neurons, microtubules are exceptionally stable, a property conferred by extensive post-translational modifications (e.g., acetylation, detyrosination) and stabilization by microtubule-associated proteins (MAPs) like tau and MAP2 [6] [3]. Neuronal microtubules are also highly organized; in axons, they exhibit a uniform plus-end-out orientation, whereas dendrites contain microtubules of mixed polarity [6].
Key Functions in Neurons:
- Intracellular Transport: Microtubules serve as tracks for the ATP-dependent movement of motor proteins. Kinesins typically transport cargo (e.g., vesicles, organelles) anterogradely toward the axon terminal, while dynein mediates retrograde transport back to the cell body [6] [3].
- Structural Support: They provide structural integrity to long axons and dendrites, resisting compressive forces [1].
- Neuronal Development: Microtubules are essential for neurite outgrowth, axon pathfinding, and the establishment of neuronal polarity during development [6].
Neurofilaments
Structure and Composition: Neurofilaments are the core type IV intermediate filaments of mature neurons, with a diameter of about 10 nm [1] [7]. They are composed of three principal subunits: neurofilament light (NF-L), medium (NF-M), and heavy (NF-H) chains, which co-assemble as obligate heteropolymers, often with α-internexin in the CNS or peripherin in the PNS [7]. Like all intermediate filament proteins, each subunit features a central α-helical rod domain flanked by variable head (N-terminal) and tail (C-terminal) domains [1] [7].
Assembly and Dynamics: Assembly begins with two monomers forming a parallel coiled-coil dimer. Two dimers then associate in an anti-parallel, staggered fashion to form a tetramer. Eight tetramers pack together to form a unit-length filament, which then anneals end-to-end to create the mature, ropelike polymer [1] [7]. This structure confers tremendous tensile strength. Neurofilaments are less dynamic than microtubules and actin and do not exhibit classic dynamic instability [1]. However, their organization and transport are highly dynamic and regulated by phosphorylation events on their head and tail domains [7].
Key Functions in Neurons:
- Radial Axonal Growth: Neurofilaments are the primary determinants of axonal caliber. A denser neurofilament network expands the axon's diameter, which in turn increases the conduction velocity of action potentials [7].
- Mechanical Strength: They provide mechanical strength, enabling neurons to withstand physical stress [1] [2].
- Synaptic Regulation: Specific subunits interact with synaptic components; for example, NF-L binds to the NMDA receptor and myosin Va, thereby influencing synaptic vesicle dynamics and receptor anchoring [7].
Actin Filaments
Structure and Composition: Actin filaments (or microfilaments) are the thinnest cytoskeletal filaments, with a diameter of roughly 7 nm [1] [2]. They are helical polymers of the protein actin, which exists as a globular monomer (G-actin) that polymerizes into filamentous F-actin [4]. The filament is polarized, featuring a fast-growing barbed end (plus end) and a slow-growing pointed end (minus end) [4].
Dynamics and Regulation: Actin filaments undergo rapid assembly and disassembly, a process controlled by a host of actin-binding proteins. Profilin promotes actin polymerization, while cofilin severs and depolymerizes existing filaments [4] [5]. The Rho family of GTPases (e.g., Rho, Rac, Cdc42) acts as master regulators, integrating extracellular signals to orchestrate large-scale actin remodeling [4]. This allows the actin cytoskeleton to be rapidly rebuilt in response to cellular needs.
Key Functions in Neurons:
- Cell Motility and Morphogenesis: Actin is the primary driver of cell crawling and, in neurons, the motility of the growth cone at the tip of a developing axon [4].
- Structural Cortex: A meshwork of actin filaments underneath the plasma membrane, known as the cell cortex, provides structural stability and defines cell shape [4] [1].
- Synaptic Plasticity: Actin is highly enriched in dendritic spines and presynaptic terminals, where its dynamic remodeling is essential for the formation, maintenance, and structural changes underlying synaptic plasticity and learning [3].
- Cargo Transport: While microtubules are the highways for long-range transport, actin facilitates short-range movements and the final positioning of cargo near the membrane [4].
Table 1: Quantitative Comparison of Core Cytoskeletal Components
| Feature | Microtubules | Neurofilaments | Actin Filaments |
|---|---|---|---|
| Diameter | ~25 nm [1] [6] | ~10 nm [1] [7] | ~7 nm [1] [2] |
| Protein Subunit | α/β-Tubulin heterodimer [6] | NF-L, NF-M, NF-H [7] | Actin [4] |
| Polymer Polarity | Yes (Plus/Minus end) [6] | No (Apolar) [1] | Yes (Barbed/Pointed end) [4] |
| Nucleotide Hydrolysis | GTP [6] | Not applicable | ATP [4] |
| Dynamic Instability | Yes [6] | No [1] | Yes (Treadmilling) [4] |
| Primary Motor Proteins | Kinesin, Dynein [6] | Myosin Va [7] | Myosin [4] |
| Key Neuronal Function | Long-range transport, Structural support [6] | Axonal caliber determination, Mechanical strength [7] | Growth cone motility, Synaptic plasticity [4] |
Cytoskeletal Defects in Neurodegeneration Mechanisms
The proper function of the cytoskeletal network is paramount for neuronal survival, and its disruption is a convergent mechanism in many neurodegenerative diseases. These defects often manifest as impaired axonal transport, aberrant filament aggregation, and a breakdown of structural integrity, ultimately leading to the characteristic "dying-back" neuropathy where the synapse degenerates first [3].
Microtubule Dysregulation
Microtubule instability is one of the earliest pathological events in several neurodegenerative disorders [6]. In Alzheimer's disease (AD), the microtubule-associated protein tau becomes hyperphosphorylated, causing it to detach from microtubules. This leads to microtubule destabilization and the self-aggregation of tau into neurofibrillary tangles (NFTs), a key pathological hallmark of the disease [6] [3]. The loss of functional tau from microtubules compromises axonal transport, depriving synapses of essential components. Furthermore, mutations in the MAPT gene encoding tau are directly linked to frontotemporal dementia, providing genetic evidence for the central role of microtubule dysfunction in neurodegeneration [3].
In Parkinson's disease (PD) and ALS, microtubule dysregulation also contributes to impaired intracellular trafficking and loss of neuronal integrity [6]. Mutations in genes encoding proteins involved in the axonal transport machinery, such as kinesin family member 5A (KIF5A) and dynactin (DCTN1), are associated with ALS and other neuropathies, directly linking transport defects to disease pathogenesis [3].
Neurofilament Aggregation and Pathophysiology
The accumulation of neurofilaments is a long-observed feature in ALS, PD, and AD [7]. While historically considered a secondary phenomenon, the discovery of rare neurological disorders caused by mutations in NF genes has solidified their primary pathogenic role. For example, mutations in the NEFL gene cause Charcot-Marie-Tooth disease type 2E, a peripheral neuropathy, by interfering with normal neurofilament assembly and transport [3] [7].
The mechanism of NF aggregation often involves hyperphosphorylation, particularly of the side-arm domains of NF-M and NF-H [7]. This aberrant phosphorylation can alter ionic interactions between subunits, disrupt their binding to molecular motors, and protect NFs from proteolysis, ultimately leading to their accumulation and aggregation in axonal swellings [7]. These aggregates physically obstruct axonal transport and are thought to contribute to the degeneration of motor neurons in ALS. Notably, neurofilament proteins themselves, especially the light chain (NF-L), have emerged as highly sensitive biomarkers in patient biofluids (blood and CSF) for monitoring neurodegeneration across a spectrum of diseases, including ALS and SMA [5] [3].
Actin Dynamics and Synaptic Failure
Defects in the actin cytoskeleton are increasingly recognized as a key factor in synaptic failure and neurodegeneration. Mutations in profilin 1 (PFN1), an actin-binding protein that regulates polymerization, are a cause of familial ALS [3]. These mutations lead to cytoskeletal defects, including impaired axonal outgrowth. In Spinal Muscular Atrophy (SMA), caused by a deficiency in the survival of motor neuron (SMN) protein, there is a profound disruption of actin dynamics in growth cones and synapses, contributing to the selective vulnerability of motor neurons [5]. Furthermore, in Huntington's disease and Fragile X syndrome, aberrant actin regulation in dendritic spines underlies the observed deficits in synaptic plasticity and cognitive function [3].
Table 2: Cytoskeletal Defects in Select Neurodegenerative Diseases
| Disease | Key Cytoskeletal Defects | Associated Genes/Proteins |
|---|---|---|
| Alzheimer's Disease (AD) | Tau hyperphosphorylation & NFT formation; Microtubule destabilization; NF accumulation [6] [3] [7] | MAPT (Tau) [3] |
| Parkinson's Disease (PD) | Microtubule dysfunction; Impaired axonal transport; Presence of NFs in Lewy bodies [6] [7] | |
| Amyotrophic Lateral Sclerosis (ALS) | NF aggregates in axons; Mutated actin-regulating proteins; Impaired axonal transport [3] [7] | SOD1, TDP-43, PFN1, KIF5A [3] |
| Charcot-Marie-Tooth Disease (CMT2E) | Disorganized NF network; Disrupted NF assembly and transport [3] [7] | NEFL [3] |
| Spinal Muscular Atrophy (SMA) | Impaired actin dynamics in growth cones; Destabilization of microtubules; Altered profiling and plastin levels [5] | SMN1 [5] |
| Frontotemporal Dementia (FTD) | Tau pathology leading to microtubule instability [3] | MAPT [3] |
Experimental Protocols for Cytoskeletal Research
Analyzing Neurofilament-Motor Protein Interactions
Objective: To characterize the direct interaction between neurofilament subunits and the cytoplasmic dynein motor complex.
Method Details:
- Protein Purification: Isolate native neurofilaments from central nervous system tissue (e.g., bovine spinal cord) via differential centrifugation. Purity is assessed by SDS-PAGE, confirming the presence of the NF triplet proteins (NF-L, NF-M, NF-H) constituting >95% of total protein [8]. Purify the dynein/dynactin complex from brain tissue using microtubule affinity and ATP-dependent release, followed by sucrose gradient sedimentation [8].
- Atomic Force Microscopy (AFM): Deposit diluted protein samples (NFs, dynein/dynactin, or mixtures) onto freshly cleaved mica. Image in fluid tapping mode to visualize single molecules and complexes in an unfixed, unstained state. To quantify binding frequency, scan along the contour of multiple neurofilaments and measure height profiles. A localized height increase >15 nm (sum of NF height ~8 nm and dynein height ~6 nm) is scored as a binding event [8].
- Yeast Two-Hybrid Screening: Use a human brain library to screen for proteins that interact with the dynein intermediate chain (DIC). Identify positive clones encoding interacting proteins, such as fragments of NF-M, via DNA sequencing and database searching. This confirms a direct protein-protein interaction [8].
- Inhibition Assays: Pre-incubate neurofilaments or dynein with function-blocking monoclonal antibodies. Subsequent AFM imaging or in vitro motility assays is used to assess the disruption of the NF-dynein interaction, validating the specificity of the binding [8].
Diagram 1: Experimental workflow for characterizing NF-motor protein interaction.
Profiling Cytoskeletal Gene Expression in Age-Related Diseases
Objective: To identify transcriptionally dysregulated cytoskeletal genes as potential biomarkers for age-related neurodegenerative and other diseases.
Method Details:
- Data Acquisition: Retrieve transcriptome data (e.g., RNA-Seq) from public repositories for disease cohorts (e.g., Alzheimer's, Cardiomyopathy) and matched controls. Obtain a curated list of cytoskeletal genes from the Gene Ontology term GO:0005856 [9].
- Machine Learning Feature Selection: Employ Recursive Feature Elimination (RFE) coupled with a Support Vector Machine (SVM) classifier. The RFE-SVM model is trained on the expression data of cytoskeletal genes and recursively prunes the least important features, identifying a minimal subset of genes that best discriminates patients from controls. Validate model performance using 5-fold cross-validation [9].
- Differential Expression Analysis: Independently analyze the transcriptome data using tools like
DESeq2orLimmato identify cytoskeletal genes with statistically significant (e.g., adjusted p-value < 0.05) expression changes between disease and control groups [9]. - Data Integration and Validation: Identify the overlapping genes from the RFE-selected features and the differential expression analysis. Validate the diagnostic power of these candidate biomarker genes using Receiver Operating Characteristic (ROC) analysis on external, independent datasets [9].
Diagram 2: Computational pipeline for cytoskeletal biomarker discovery.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Tools for Cytoskeletal Research
| Reagent / Tool | Function / Application | Example Use-Case |
|---|---|---|
| Paclitaxel (Taxol) | Microtubule-stabilizing drug. Binds to and stabilizes polymerized microtubules, suppressing dynamic instability [8] [6]. | Used in protein purification to stabilize microtubules for motor protein assays; employed in cellular models to study the effects of hyper-stable microtubules [8]. |
| Profilin & Cofilin | Actin-binding proteins. Profilin promotes G-actin polymerization; Cofilin severs and depolymerizes F-actin [4] [5]. | Used in in vitro actin polymerization assays to manipulate dynamics; studied in cellular models of ALS (mutant PFN1) and SMA to understand pathogenesis [5] [3]. |
| Function-Blocking Antibodies | Monoclonal antibodies that inhibit the activity of specific target proteins. | Antibodies against dynein IC or NF-M used in AFM/in vitro assays to block and study specific protein interactions [8]. |
| SOMAmer Technology | Slow Off-rate Modified Aptamers; a high-throughput proteomic platform for measuring thousands of proteins in biofluids [10]. | Used in large consortia (e.g., GNPC) to discover and validate protein biomarkers, including cytoskeletal proteins like neurofilaments, in plasma and CSF [10]. |
| [11C]MPC‑6827 | A positron emission tomography (PET) radiotracer that selectively binds to destabilized microtubules [6]. | Enables non-invasive, in vivo imaging of microtubule instability in the brains of living patients with AD or PD, serving as a translational diagnostic tool [6]. |
| Tubulin & Actin Polymerization Assay Kits | Commercial kits containing purified proteins and buffers to monitor in vitro polymerization in real-time (e.g., via fluorescence). | Used for high-throughput screening of compounds that modulate microtubule or actin dynamics for drug discovery [6]. |
The essential cytoskeletal components—microtubules, neurofilaments, and actin filaments—form an integrated, dynamic network that is fundamental to neuronal architecture, function, and survival. The precise regulation of their assembly, disassembly, and transport is critical for maintaining axonal integrity, synaptic connectivity, and cellular homeostasis. As detailed in this whitepaper, the breakdown of this delicate balance is a central mechanism in the pathogenesis of a wide spectrum of neurodegenerative diseases. The convergence of genetic, biochemical, and histopathological evidence firmly establishes cytoskeletal defects not as a mere secondary consequence but as a primary driver of neurodegeneration.
Current research, leveraging advanced techniques from atomic force microscopy and machine learning to in vivo PET imaging, is rapidly translating this knowledge into clinical applications. The emergence of neurofilament proteins as fluid biomarkers and the development of tracers for microtubule stability herald a new era for early diagnosis and disease monitoring. Future therapeutic efforts aimed at directly stabilizing the cytoskeleton, modulating the activity of associated proteins, or correcting aberrant post-translational modifications hold significant promise. For researchers and drug development professionals, targeting the cytoskeleton offers a powerful, mechanistic approach to developing the next generation of treatments for neurodegenerative disorders.
Cytoskeletal Defects as a Unifying Hallmark Across Neurodegenerative Disorders
The neuronal cytoskeleton is an intricate, dynamic network essential for maintaining neuronal structure, facilitating intracellular transport, and supporting synaptic function. Comprising three primary polymeric structures—microtubules (composed of tubulin), intermediate filaments (neurofilaments), and actin-based microfilaments—this complex system enables neurons to construct, maintain, and modify their elaborate architecture [3]. In neurodegenerative diseases, this carefully orchestrated system undergoes progressive disintegration, leading to a cascade of cellular failures. Cytoskeletal defects represent a fundamental pathological hallmark shared across diverse neurodegenerative disorders, including Alzheimer's disease (AD), Parkinson's disease (PD), amyotrophic lateral sclerosis (ALS), frontotemporal dementia (FTD), and Huntington's disease (HD) [3] [11]. These defects disrupt critical cellular processes, ultimately resulting in the characteristic clinical manifestations of these devastating conditions.
The significance of cytoskeletal pathology in neurodegeneration is underscored by its recent identification as one of the eight core hallmarks of neurodegenerative diseases, alongside pathological protein aggregation, synaptic dysfunction, aberrant proteostasis, altered energy homeostasis, DNA/RNA defects, inflammation, and neuronal cell death [11] [12]. This review comprehensively examines the molecular mechanisms linking cytoskeletal abnormalities to neurodegenerative processes, presents current experimental methodologies for their investigation, and explores emerging therapeutic strategies targeting cytoskeletal integrity.
Molecular Composition and Functions of the Neuronal Cytoskeleton
Core Cytoskeletal Components
The neuronal cytoskeleton consists of three structurally and functionally distinct filament systems that collectively determine cell morphology, mechanical properties, and intracellular organization. Microtubules, the stiffest of the three polymers, are hollow tubes composed of αβ-tubulin heterodimers with a persistence length of approximately 5 mm, enabling them to form nearly linear tracks that span the considerable length of mature neurons [13]. These structures serve as primary highways for intracellular transport, guiding the movement of vesicles, organelles, and cargo via molecular motor proteins including kinesins and dyneins [13]. Actin filaments (microfilaments) are more flexible polymers that organize into complex networks and bundles beneath the plasma membrane and at synaptic terminals. They are crucial for maintaining cell shape, facilitating motility, and mediating structural plasticity at dendritic spines and other specialized neuronal compartments [13] [3]. Intermediate filaments, particularly neurofilaments in mature neurons, provide crucial mechanical strength and regulate axon diameter, thereby influencing conductivity velocity and structural integrity [3].
Regulatory Proteins and Molecular Interactions
The organization and dynamics of these cytoskeletal networks are controlled by numerous regulatory proteins that govern assembly, disassembly, and higher-order organization. Key regulators include nucleation-promoting factors that initiate filament formation, capping proteins that terminate filament growth, polymerases that promote sustained elongation, depolymerizing factors that disassemble filaments, and crosslinkers that organize higher-order network structures [13]. Particularly important in neuronal contexts are microtubule-associated proteins (MAPs) such as tau, which stabilize microtubules and regulate motor protein access [3]. The actin cytoskeleton is similarly regulated by proteins like cofilin (which severs and depolymerizes actin filaments), profilin (which promotes actin polymerization), and formins (which nucleate linear actin filaments) [13] [14]. Cross-linking proteins including bullous pemphigoid antigen 1 (BPAG1) and microtubule actin cross-linking factor 1 (MACF1) stabilize connections between different cytoskeletal elements, creating an integrated network [3].
Table 1: Major Cytoskeletal Components in Neurons and Their Primary Functions
| Cytoskeletal Element | Protein Composition | Key Functions | Regulatory Proteins |
|---|---|---|---|
| Microtubules | αβ-tubulin heterodimers | Intracellular transport, structural support, mitotic spindle organization | Tau, MAP2, kinesin, dynein |
| Actin Filaments | Actin | Cell shape determination, structural plasticity, endocytosis, cytokinesis | Cofilin, profilin, formins, WAVE complex |
| Intermediate Filaments | Neurofilament proteins (NFL, NFM, NFH) | Mechanical strength, axon caliber regulation, organelle positioning | Kinases, phosphatases |
Cytoskeletal Defects in Major Neurodegenerative Diseases
Alzheimer's Disease
Alzheimer's disease presents profound cytoskeletal pathology characterized by neurofibrillary tangles composed of hyperphosphorylated tau protein. In healthy neurons, tau normally stabilizes microtubules and promotes their assembly. In AD, abnormal phosphorylation of tau reduces its affinity for microtubules, leading to microtubule destabilization and collapse of the transport system [3]. The dissociated tau subsequently aggregates into paired helical filaments and eventually neurofibrillary tangles, which represent a defining neuropathological feature of the disease [15] [3]. Beyond tau pathology, actin cytoskeleton abnormalities also contribute to AD pathogenesis. Recent research has identified that mutations to the actin-ATP interface (K18A, D154A, G158L, K213A) promote the formation of disease-associated actin-rich structures including cofilin-actin rods and Hirano bodies, which disrupt synaptic function and contribute to spine loss [14].
Parkinson's Disease
While Parkinson's disease is traditionally characterized by Lewy bodies containing aggregated α-synuclein, emerging evidence indicates significant cytoskeletal involvement in its pathogenesis. Mutations in genes encoding the microtubule-associated protein tau have been identified as risk factors for PD, suggesting shared pathogenic mechanisms with primary tauopathies [3]. Additionally, defects in axonal transport machinery have been documented in PD models, with impaired mitochondrial trafficking contributing to the selective vulnerability of dopaminergic neurons in the substantia nigra [3]. The actin cytoskeleton also undergoes alterations in PD, with disruptions in actin-binding proteins contributing to synaptic dysfunction and neuronal death [16].
Amyotrophic Lateral Sclerosis
ALS demonstrates prominent cytoskeletal pathology manifested through abnormalities in all three cytoskeletal systems. Mutations in the gene encoding neurofilament light chain (NEFL) cause Charcot-Marie-Tooth disease type 2E, with mutant NEFL interfering with proper neurofilament assembly and transport [3]. Additionally, mutations in profilin 1 (PFN1), an actin-binding protein, lead to ALS pathogenesis through disrupted actin polymerization and the formation of ubiquitinated protein aggregates [3]. TAR DNA-binding protein 43 (TDP-43) inclusions, a pathological hallmark of most ALS cases, are associated with impaired axonal transport and cytoskeletal disorganization, ultimately leading to the degeneration of motor neurons [3].
Frontotemporal Dementia and Huntington's Disease
Frontotemporal dementia frequently involves direct tau pathology, with mutations in the MAPT gene encoding tau leading to familial forms of the disorder [3]. These mutations result in microtubule destabilization and breakdown of the neuronal cytoskeleton, accompanied by the formation of toxic tau aggregates [3]. In Huntington's disease, mutant huntingtin protein disrupts vesicular transport along microtubules by interfering with molecular motor proteins, particularly kinesin-1 and dynein [3]. This transport deficit contributes to the selective vulnerability of striatal neurons, even though huntingtin itself is widely expressed throughout the brain.
Table 2: Cytoskeletal Defects in Major Neurodegenerative Diseases
| Disease | Primary Cytoskeletal Defects | Associated Gene Mutations | Resulting Pathological Inclusions |
|---|---|---|---|
| Alzheimer's Disease | Tau hyperphosphorylation, microtubule destabilization, actin rod formation | MAPT (tau) | Neurofibrillary tangles, cofilin-actin rods, Hirano bodies |
| Parkinson's Disease | Impaired axonal transport, tau pathology, actin dynamics disruption | MAPT | Lewy bodies, neurofibrillary tangles |
| Amyotrophic Lateral Sclerosis | Neurofilament aggregation, disrupted actin polymerization, impaired transport | NEFL, PFN1, TDP-43 | Neurofilament aggregates, ubiquitinated inclusions |
| Frontotemporal Dementia | Tau dysfunction, microtubule instability | MAPT | Tau inclusions, neurofibrillary tangles |
| Huntington's Disease | Disrupted vesicular transport, impaired motor protein function | HTT (huntingtin) | Huntingtin aggregates |
Molecular Mechanisms Linking Cytoskeletal Defects to Neurodegeneration
Disrupted Axonal Transport
The extreme polarity and considerable length of neurons make them uniquely dependent on efficient axonal transport for their survival and function. The cytoskeleton provides the structural framework for this transport, with microtubules serving as tracks for motor proteins that carry essential cargo between the cell body and synaptic terminals [13] [3]. Cytoskeletal disruptions directly impair this critical process, leading to a "dying-back" pattern of degeneration where distal synapses and axons degenerate before the cell body [3]. Mutations in genes encoding components of the axonal transport machinery, including kinesin family member 5A (KIF5A) and dynactin 1 (DCTN1), have been directly linked to ALS and Charcot-Marie-Tooth disease, highlighting the fundamental importance of intact transport systems for neuronal health [3]. The collapse of efficient transport results in improper distribution of vesicles, organelles (including mitochondria), and essential components between the cell body and synaptic endings, ultimately compromising synaptic function and neuronal viability [3].
Actin Dynamics and Synaptic Dysfunction
The actin cytoskeleton plays particularly important roles at synapses, where it forms the structural core of dendritic spines and participates in the trafficking of neurotransmitter receptors. Defects in actin regulatory proteins have been implicated in multiple neurodegenerative conditions. For example, mutations in profilin 1 (PFN1), which promotes actin polymerization, cause ALS by disrupting actin dynamics and leading to the formation of pathological inclusions [3]. Similarly, abnormalities in LIM domain kinase 1 (LIMK1), which phosphorylates and inactivates the actin depolymerizing factor cofilin, have been associated with spine morphology defects in Williams syndrome [3]. Recent research has demonstrated that specific mutations at the actin-ATP interface (K18A, D154A, G158L, K213A) promote the formation of cofilin-actin rods and Hirano bodies under conditions of cellular stress, providing a direct mechanistic link between actin pathology and neurodegenerative processes [14]. These actin-rich aggregates sequester essential actin-binding proteins, disrupt synaptic function, and contribute to the elimination of excitatory synapses [14].
Cytoskeletal Cross-Talk and Integration
The different components of the cytoskeleton do not function in isolation but rather engage in extensive cross-talk that integrates their activities. Plakins such as BPAG1 and MACF1 physically cross-link different cytoskeletal elements, allowing coordinated responses to mechanical and biochemical signals [3]. The Rho GTPase family members, including RhoA, Rac1, and Cdc42, serve as key regulators of cytoskeletal dynamics, controlling actin organization and microtubule stability through complex signaling networks [3]. During neurodegeneration, disruptions to this integrated cytoskeletal network become progressively amplified through positive feedback loops. For example, activation of the RhoA signaling pathway leads to cytoskeletal remodeling, which in turn activates myocardin-related transcription factor (MRTF), promoting the expression of fibrosis-related genes and further strengthening RhoA signaling [17].
Experimental Models and Methodologies
Investigating Actin Pathology Using the CofActor System
Recent advances in optogenetic tools have enabled more precise investigation of cytoskeletal dynamics in living cells. The CofActor system represents an innovative approach for studying actin-cofilin interactions in a light- and stress-gated manner [14]. This system consists of two primary components: (1) a blue-light responsive cryptochrome 2 (Cry2)-Cofilin.S3E protein fusion, and (2) a betaActin-CIB protein fusion [14]. Upon blue light activation in the presence of cellular stress (e.g., ATP depletion), these components interact to form cytoplasmic clusters that can be quantitatively monitored using live-cell imaging techniques.
Experimental Protocol for CofActor Analysis:
- Cell Culture and Transfection: Plate HeLa cells or primary cortical neurons in appropriate culture conditions. Transfect with CofActor constructs (Cry2-mCherry-Cofilin.S3E and betaActin-CIB-GFP) using standard transfection methods.
- Stress Induction: Induce energetic stress using mitochondrial inhibitors (e.g., sodium azide) or oxidative stress using glutamate excitotoxicity models.
- Optogenetic Activation: Expose cells to 470 nm blue light to activate the Cry2-CIBN interaction system. Typically, light activation for 30-second intervals followed by imaging every 30 seconds provides optimal temporal resolution.
- Image Acquisition and Analysis: Capture time-lapse images using widefield or confocal microscopy. Quantify cluster formation using image analysis software (e.g., FIJI/ImageJ) with the Analyze Particles feature to determine particle counts, size distribution, and fluorescence intensity over time.
- Mutant Analysis: Introduce specific point mutations into the actin-ATP interface (e.g., K18A, D154A, G158L, K213A) to investigate their effects on cluster formation under stress conditions.
This methodology has revealed that mutations at the actin-ATP interface significantly alter the propensity to form anomalous actin structures, providing insight into how specific actin residues contribute to neurodegenerative disease progression [14].
Diagram 1: CofActor experimental workflow for analyzing actin-cofilin interactions.
Advanced Imaging and Visualization Techniques
The investigation of cytoskeletal defects in neurodegeneration relies heavily on advanced imaging methodologies that enable visualization of cytoskeletal dynamics in live cells and intact tissues. Recent advances in the visualization of the microtubule and actin cytoskeleton in multicellular organisms have provided unprecedented insights into cytoskeletal organization and dynamics [3]. Key approaches include:
- High-resolution live-cell microscopy using GFP-tagged cytoskeletal proteins to monitor dynamics in real-time
- Total internal reflection fluorescence (TIRF) microscopy for visualizing cytoskeletal structures near the plasma membrane
- Structured illumination microscopy (SIM) and stimulated emission depletion (STED) microscopy to overcome diffraction limits and resolve fine cytoskeletal details
- Electron microscopy techniques for ultrastructural analysis of cytoskeletal organization
- Combined approaches that correlate light and electron microscopy data to bridge resolution gaps
These techniques have revealed that both internal and external physical forces can act through the cytoskeleton to affect local mechanical properties and cellular behavior, with long-lived cytoskeletal structures potentially serving as epigenetic determinants of cell shape, function, and fate [13].
Therapeutic Approaches and Research Reagents
Targeting Cytoskeletal Pathways
Current therapeutic strategies for addressing cytoskeletal defects in neurodegenerative diseases focus on normalizing cytoskeletal dynamics, enhancing axonal transport, and reducing pathological protein aggregation. These approaches include:
Microtubule-Stabilizing Compounds:
- Epothilone D - crosses the blood-brain barrier and enhances microtubule stability, shown to improve axonal transport and reduce tau pathology in animal models of AD
- TPI-287 - a taxane-derived microtubule stabilizer evaluated in clinical trials for AD and PSP
- Naturally occurring compounds such as paclitaxel and its derivatives, which reduce microtubule dynamics but face challenges with blood-brain barrier penetration
Actin Dynamics Modulators:
- Rho kinase (ROCK) inhibitors - target the RhoA-ROCK pathway involved in stress fiber formation and neurite retraction
- Cofilin inhibitors - designed to prevent pathological cofilin-actin rod formation
- Blebbistatin - a selective inhibitor of non-muscle myosin II that reduces actin-myosin contractility
Signaling Pathway Modulators:
- LIMK inhibitors - target the kinase responsible for cofilin phosphorylation, potentially normalizing actin dynamics
- Rho GTPase modulators - influence multiple cytoskeletal regulatory pathways
Table 3: Research Reagent Solutions for Cytoskeletal Studies
| Reagent Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| Optogenetic Tools | CofActor system (Cry2-Cofilin.S3E, betaActin-CIB) [14] | Live-cell imaging of actin-cofilin dynamics | Light- and stress-gated monitoring of cytoskeletal protein interactions |
| Chemical Inhibitors/Activators | Rho kinase inhibitors (Y-27632), Microtubule stabilizers (Taxol), Cofilin inhibitors | Pathway modulation in cellular and animal models | Targeted manipulation of specific cytoskeletal regulatory pathways |
| Live-Cell Probes | GFP-tagged cytoskeletal proteins, SiR-actin/tubulin stains, Photoactivatable probes | Real-time visualization of cytoskeletal dynamics | Fluorescent labeling and tracking of cytoskeletal components |
| Genetic Tools | CRISPR/Cas9 gene editing, siRNA/shRNA knockdown, Mutant constructs (K18A, D154A actin) [14] | Genetic manipulation of cytoskeletal components | Selective alteration of specific cytoskeletal proteins and their regulators |
Multi-Targeted Therapeutic Strategies
Given the complexity of cytoskeletal defects in neurodegenerative diseases, effective therapeutic approaches will likely require multi-targeted strategies that address multiple pathological processes simultaneously [16] [11]. Promising approaches include:
- Combination therapies that simultaneously target cytoskeletal integrity and disease-specific protein aggregation
- Disease-modifying strategies focused on enhancing cellular resilience to cope with toxic protein species
- Interventions targeting shared pathways such as energy metabolism, oxidative stress, and neuroinflammation that indirectly influence cytoskeletal health
- Gene-based therapies designed to correct specific genetic defects affecting cytoskeletal proteins
These approaches recognize that cytoskeletal defects do not occur in isolation but rather interact with other hallmark pathological processes in neurodegeneration, including protein aggregation, synaptic dysfunction, and inflammatory responses [16] [11].
Diagram 2: Pathogenic cascade linking cytoskeletal defects to neurodegeneration.
Cytoskeletal defects represent a fundamental pathological hallmark shared across diverse neurodegenerative disorders, contributing directly to clinical symptomatology through disrupted axonal transport, synaptic failure, and loss of structural integrity. The integrated view of cytoskeletal pathology presented in this review highlights common mechanisms while acknowledging disease-specific variations. As research in this field advances, several promising directions emerge:
First, the development of increasingly sophisticated tools for visualizing and manipulating cytoskeletal dynamics in live cells and intact organisms will continue to provide deeper insights into pathological mechanisms. Second, the identification of cytoskeletal biomarkers - particularly neurofilament proteins in biofluids - offers potential for improved diagnosis and tracking of disease progression [3]. Third, therapeutic strategies that target cytoskeletal defects as part of a comprehensive, multi-target approach hold promise for effectively modifying disease progression across multiple neurodegenerative conditions.
Ultimately, recognizing cytoskeletal defects as a unifying hallmark of neurodegenerative diseases reframes our conceptual approach to these disorders, emphasizing shared pathogenic mechanisms while acknowledging disease-specific variations. This perspective provides a robust framework for developing novel diagnostic and therapeutic strategies aimed at preserving neuronal structure and function in the face of neurodegenerative assault.
The neuronal cytoskeleton, composed of microtubules, neurofilaments, and actin filaments, serves as the structural foundation for axonal transport—a critical process that maintains neuronal health and function. Neurons are highly polarized cells with markedly compartmentalized structures, making them reliant on intricate transport systems to shuttle newly synthesized macromolecules and organelles from the cell body to distant synaptic terminals (anterograde transport) and to return signaling endosomes and autophagosomes for degradation (retrograde transport). This continuous bidirectional trafficking occurs along microtubule highways powered by molecular motor proteins: kinesins primarily mediate anterograde transport toward the synapse, while cytoplasmic dynein drives retrograde transport back to the cell body [18].
The proper functioning of axonal transport is fundamental to neuronal survival, as it ensures the appropriate distribution of essential components throughout the extensive axonal architecture. Disruption of this finely balanced system represents an early and critical event in the pathogenesis of multiple neurodegenerative diseases, including Alzheimer's disease (AD), Parkinson's disease (PD), amyotrophic lateral sclerosis (ALS), and hereditary spastic paraplegia [18]. This whitepaper examines the molecular mechanisms underlying axonal transport failure, with particular emphasis on kinesin and dynein dysfunction within the broader context of cytoskeletal defects in neurodegeneration.
Molecular Mechanisms of Motor Protein Dysfunction
Regulation of Motor Protein Function and Cargo Binding
Motor proteins do not function in isolation; their activity is precisely regulated through interactions with binding partners, adaptor proteins, and post-translational modifications. Recent research has identified kinesin-binding protein as a key regulator of CHMP2B, a core component of the endosomal sorting complex required for transport (ESCRT) pathway. This regulation is crucial for the processive movement and presynaptic localization of CHMP2B, which facilitates endolysosomal protein degradation at synapses. The frontotemporal dementia-causative CHMP2Bintron5 mutation exhibits deficient binding to kinesin-binding protein, resulting in impaired axonal transport characterized by little processive movement and oscillatory behavior of transport vesicles—a phenotype reminiscent of a tug-of-war between kinesin and dynein motor proteins [19].
The annexin family of calcium-binding proteins provides another layer of motor protein regulation. Annexin A7 (ANXA7) enhances the axonal trafficking of TIA1, an RNA-binding protein that forms ribonucleoprotein (RNP) granules. This process is calcium-dependent, with calcium overload inducing phase separation of ANXA7-TIA1 complexes and consequently halting their transport. This mechanism is particularly relevant for ALS, where TIA1 mutations are associated with pathological protein aggregation. ANXA7 serves as a molecular bridge connecting TIA1-containing RNPs to dynein, facilitating their retrograde transport from axonal terminals to the cell body. Disruption of this system leads to TIA1 granule accumulation in axons and subsequent neurodegeneration [20].
Cytoskeletal Defects and Motor Protein Impairment
The integrity of microtubule networks is essential for efficient axonal transport, and modifications to tubulin or microtubule-associated proteins can severely disrupt motor protein function. In ALS, evidence suggests that tubulin nitration near the dynactin binding site may destabilize microtubule tracts and interfere with dynein motor function [21]. This nitration occurs through peroxynitrite formation, which modifies tyrosine residues on the aromatic ring. Since superoxide dismutase (SOD) normally prevents peroxynitrite formation, SOD1 mutations in familial ALS may promote tubulin nitration, creating a direct link between oxidative stress and transport defects along microtubules [21].
Tau, a microtubule-associated protein, plays a critical role in stabilizing microtubules and regulating motor protein function. In AD and other tauopathies, hyperphosphorylated tau exhibits reduced binding affinity to microtubules, potentially destabilizing them. However, hyperphosphorylated tau alone does not form fibrils unless sulphated aminoglycans such as heparin sulfate are present, suggesting that microtubule modifications may facilitate pathological fibril formation [21]. The specific tau isoforms also influence transport efficiency; mutations that increase the ratio of four-repeat to three-repeat tau isoforms enhance microtubule binding strength and aggregation propensity, further impairing axonal transport [21].
Table 1: Motor Protein Dysfunctions in Neurodegenerative Diseases
| Disease | Motor Protein Affected | Molecular Mechanism | Functional Consequence |
|---|---|---|---|
| Frontotemporal Dementia (linked to CHMP2Bintron5) | Kinesin | Deficient binding to kinesin-binding protein | Loss of processive movement, oscillatory transport vesicles, impaired presynaptic localization |
| Amyotrophic Lateral Sclerosis (ALS) | Dynein | Tubulin nitration near dynactin binding site | Impaired retrograde transport, organelle accumulation |
| Alzheimer's Disease | Kinesin and Dynein | Hyperphosphorylated tau destabilizing microtubules | Reduced microtubule stability, impaired bidirectional transport |
| ALS/FTD (linked to TIA1 mutations) | Dynein | Disrupted ANXA7-TIA1-dynein complex in calcium overload | Defective RNP granule transport, pathological aggregation in axons |
Axonal Transport Deficits in Neurodegenerative Diseases
Alzheimer's Disease and Tauopathies
In Alzheimer's disease, the relationship between cytoskeletal defects and axonal transport disruption represents a core pathological mechanism. While amyloid precursor protein (APP) and presenilin mutations influence the production and accumulation of amyloid-β peptides, neurofibrillary tangles consisting of hyperphosphorylated tau are more closely correlated with cognitive decline. Tau normally stabilizes microtubules, but when hyperphosphorylated, it dissociates from microtubules and aggregates into paired helical filaments. This loss of functional tau decreases microtubule stability, while the accumulated tau aggregates may physically impede motor protein progression along axons [21].
The significance of tau-mediated transport disruption extends beyond AD to a class of disorders collectively known as tauopathies, which include frontotemporal dementia with parkinsonism linked to chromosome 17 (FTDP-17), corticobasal degeneration, progressive supranuclear palsy, and Pick's disease. In FTDP-17, mutations in the tau gene directly cause disease, with some mutations altering the ratio of three-repeat to four-repeat tau isoforms and others affecting tau's binding affinity to microtubules [22]. These changes not only impair microtubule stability but also influence the motility of both kinesin and dynein motors, ultimately disrupting the balanced bidirectional transport essential for neuronal function.
Amyotrophic Lateral Sclerosis and Related Disorders
ALS exemplifies the devastating consequences of disrupted axonal transport on motor neuron survival. Multiple pathways converge to impair motor protein function in this disease. Mutations in SOD1, present in approximately 2% of familial ALS cases, were initially thought to cause disease through loss of antioxidant function. However, SOD1 null mice do not develop ALS-like pathology, suggesting a toxic gain-of-function mechanism instead [21]. Mutant SOD1 promotes protein aggregation that sequesters essential motor proteins and transport components, leading to measurable slowing of axonal transport in motor neurons—an early event in ALS pathophysiology [21].
The critical role of axonal transport in ALS is further highlighted by recent discoveries concerning RNA-binding proteins. In ALS and frontotemporal dementia, TIA1 protein mutations promote pathological phase separation and aggregation, disrupting the transport of mRNA granules in axons. The calcium-regulated mechanism of Annexin A7 in mediating TIA1-RNP transport via dynein provides a compelling link between calcium signaling defects and impaired axonal transport in neurodegeneration. When this transport fails, TIA1 granules accumulate in axons, forming pathological aggregates that trigger degenerative processes [20].
Table 2: Quantitative Measures of Axonal Transport Defects in Neurodegeneration
| Experimental Model | Transport Parameter Measured | Change in Disease State | Technical Method |
|---|---|---|---|
| CHMP2Bintron5 mutant neurons | Processive movement | Drastic reduction | Live-cell imaging of fluorescently tagged CHMP2B |
| CHMP2Bintron5 mutant neurons | Vesicle dynamics | Increased oscillatory behavior ("tug-of-war") | Kymograph analysis of vesicle movements |
| ANXA7-deficient neurons | Retrograde transport velocity | Decreased by >50% | Live imaging of TIA1-RNP granules in axons |
| SOD1 mutant models | Axonal transport rate | Significant slowing | Radiolabeled protein tracking in motor neurons |
| Hyperphosphorylated tau models | Mitochondrial transport | Reduced velocity and increased pausing | Live imaging of mito-GFP in axons |
Experimental Approaches and Methodologies
Live Imaging of Axonal Transport
The direct observation of cargo movement in living neurons has revolutionized our understanding of axonal transport dynamics. Current methodologies employ high-resolution live-cell imaging to track fluorescently labeled organelles, vesicles, or protein complexes in real-time. For investigating CHMP2B transport, researchers typically culture hippocampal or cortical neurons from rodent models, transfect them with fluorescent protein-tagged CHMP2B constructs (both wild-type and mutant forms), and conduct time-lapse imaging using spinning disk or TIRF microscopy. The resulting videos are analyzed with kymograph tools to quantify transport parameters including velocity, processivity, run length, and directionality. This approach revealed that while wild-type CHMP2B exhibits robust activity-dependent transport to presynaptic boutons, the CHMP2Bintron5 mutant displays minimal directed movement with increased oscillatory behavior [19].
For studying RNP granule transport, as in the ANXA7-TIA1 mechanism, researchers use microfluidic chambers to physically isolate axons from cell bodies, enabling clear observation of axonal transport without interference from somatic processes. Neurons are transfected with fluorescently tagged TIA1, and RNP movement is tracked before and after calcium influx induction. Fluorescence recovery after photobleaching (FRAP) can further assess granule dynamics and phase separation properties. Through these methods, researchers determined that ANXA7 knockdown reduces retrograde transport velocity of TIA1 granules by over 50%, while ANXA7 overexpression can rescue transport defects caused by disease-associated TIA1 mutations [20].
Biochemical and Molecular Analyses
Complementary biochemical approaches are essential for elucidating the molecular interactions underlying transport defects. Co-immunoprecipitation assays demonstrate physical interactions between motor proteins and their cargo adapters. For example, immunoprecipitation of ANXA7 from neuronal lysates followed by mass spectrometry identification of binding partners established its role as a molecular bridge between TIA1 and the dynein motor complex [20]. Similarly, comparative co-immunoprecipitation of wild-type versus mutant CHMP2B with kinesin-binding protein confirmed the deficient interaction in the disease-associated variant [19].
Proximity ligation assays (PLA) provide spatial information about protein interactions within cellular contexts, revealing disrupted molecular proximities in disease states. In vitro microtubule binding and motility assays using purified components allow researchers to dissect the direct effects of pathogenic proteins on motor function, isolating these mechanisms from broader cellular influences. These reductionist approaches have been instrumental in demonstrating how mutant SOD1 directly impairs kinesin motility on microtubules and how hyperphosphorylated tau creates physical barriers to motor protein movement.
Figure 1: Experimental Approaches for Studying Axonal Transport Mechanisms. This workflow integrates live imaging, biochemical assays, genetic manipulation, and animal models to comprehensively investigate motor protein dysfunction in neurodegeneration.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating Axonal Transport Defects
| Reagent/Tool | Specific Example | Research Application | Key Function |
|---|---|---|---|
| Fluorescent protein tags | GFP-, RFP-, mCherry-tagged CHMP2B | Live imaging of ESCRT component transport | Visualizing and quantifying processive movement and synaptic recruitment |
| Microfluidic chambers | Compartmentalized neuronal culture chips | Isolation of axons for transport studies | Analyzing directional transport without somatic interference |
| Kymograph analysis software | ImageJ KymoToolBox | Quantification of vesicle dynamics | Measuring velocity, processivity, and directionality of moving cargo |
| Site-directed mutagenesis kits | CHMP2Bintron5 mutation | Introducing disease-associated mutations | Modeling genetic forms of neurodegeneration |
| Calcium indicators | GCaMP, Fura-2 | Monitoring intracellular calcium dynamics | Linking calcium signaling to transport regulation |
| Motor protein inhibitors | Ciliobrevin D (dynein inhibitor) | Disrupting specific motor functions | Determining contribution of specific motors to transport defects |
| Proximity ligation assay | Duolink PLA | Detecting protein-protein interactions | Visualizing molecular complexes in situ |
| Gene manipulation vectors | shRNA for ANXA7 knockdown | Modulating expression of regulatory proteins | Establishing necessity of adaptor proteins for transport |
Therapeutic Approaches and Future Directions
Targeting Motor Protein Regulation
Emerging therapeutic strategies for neurodegenerative diseases focus on restoring axonal transport by targeting motor protein regulation and function. One promising approach involves enhancing the connectivity between motor proteins and their cargo. In the case of CHMP2Bintron5-related neurodegeneration, strategies that strengthen the interaction between mutant CHMP2B and kinesin-binding protein could potentially restore its axonal transport and presynaptic localization [19]. Similarly, modulating the ANXA7-TIA1-dynein interaction presents a therapeutic opportunity for ALS, particularly since ANXA7 overexpression has been shown to rescue TIA1 transport defects and reverse pathology in model systems [20].
Small molecule compounds that enhance kinesin or dynein processivity represent another innovative approach. These compounds could increase the run length of motor proteins, helping them overcome partial transport barriers formed by protein aggregates or cytoskeletal abnormalities. Additionally, compounds that regulate the phosphorylation state of motor proteins or their adaptors may optimize transport efficiency. For instance, glycogen synthase kinase-3β (GSK-3β) inhibitors can reduce pathological tau phosphorylation, thereby improving microtubule stability and motor protein function—a strategy being explored for Alzheimer's disease and other tauopathies.
Integrated Therapeutic Strategies
Given the complex, multifactorial nature of axonal transport breakdown, effective treatments will likely require integrated approaches that address multiple pathological mechanisms simultaneously. Gene therapy strategies that deliver neuroprotective factors like ANXA7 or functional versions of disease-associated genes offer promising avenues for inherited neurodegenerative conditions [20]. Meanwhile, approaches that enhance cellular protein clearance mechanisms, such as the ESCRT pathway whose components depend on proper axonal transport, may help reduce the burden of pathological protein aggregates [19].
The development of these targeted therapies depends on continued advances in understanding the basic biology of axonal transport and its regulation. Future research should focus on elucidating the precise molecular interactions between motor proteins, their adaptors, and cargoes; mapping the signaling pathways that regulate these interactions in response to neuronal activity and stress; and identifying how disease-associated mutations specifically disrupt these processes. Such insights will enable the rational design of therapeutics that can restore axonal transport in a precise and disease-specific manner.
Figure 2: Therapeutic Strategies Targeting Axonal Transport Breakdown. Multiple intervention points exist for restoring axonal transport, including direct enhancement of motor protein function, stabilization of the cytoskeleton, and correction of cargo mislocalization through genetic and pharmacological approaches.
The investigation of axonal transport breakdown represents a crucial frontier in understanding and treating neurodegenerative diseases. As research continues to unravel the intricate relationships between kinesin, dynein, cytoskeletal elements, and disease-associated proteins, new opportunities for therapeutic intervention will emerge. By targeting the fundamental mechanisms of motor protein dysfunction within the broader context of cytoskeletal defects, researchers and drug development professionals can work toward effective treatments that address the root causes of neurodegeneration rather than merely alleviating symptoms.
The neuronal cytoskeleton, a dynamic network of microtubules, neurofilaments, and actin microfilaments, serves as the fundamental architectural and functional backbone of the neuron. This tripartite system maintains structural integrity, enables morphological plasticity, and facilitates essential processes including axonal transport, synaptic function, and intracellular signaling [23] [24] [25]. Microtubules, composed of α/β-tubulin heterodimers, provide polarized tracks for the active transport of vesicles, organelles, and proteins [24] [25]. Neurofilaments, as intermediate filaments, confer mechanical strength and regulate axonal caliber [24]. Actin microfilaments govern synaptic remodeling and dendritic spine dynamics through continuous assembly and disassembly [24]. The precise regulation of this cytoskeletal network is critical for neuronal homeostasis, and its progressive collapse is a central event in neurodegenerative pathogenesis [23] [24].
This review examines the pathological interplay between key aggregating proteins—tau and α-synuclein—and the cytoskeletal framework, positioning cytoskeletal defects as a critical mechanistic nexus in neurodegeneration. We explore how the functional impairment of tau, a microtubule-associated protein, and α-synuclein, a presynaptic protein, triggers a "dying back" pattern of degeneration that begins at the vulnerable synaptic terminals and progresses along the axon [26]. The synergistic relationship between these proteinopathies, their co-aggregation, and their combined disruptive effects on cytoskeletal integrity represent a compelling paradigm for understanding disease progression in conditions like Alzheimer's disease (AD), Parkinson's disease (PD), and other related dementias [26] [27] [28].
Molecular Physiology of Cytoskeletal-Associated Proteins
Tau: Architect of Microtubule Stability
Tau is an intrinsically disordered microtubule-associated protein (MAP) predominantly expressed in neurons, where it plays a pivotal role in stabilizing microtubules and regulating axonal transport [26] [24]. The MAPT gene on chromosome 17 undergoes complex alternative splicing to generate six major isoforms in the human central nervous system [26] [24]. These isoforms differ by the inclusion of 0, 1, or 2 N-terminal inserts (0N, 1N, 2N) and either three or four microtubule-binding repeats (3R, 4R), resulting in proteins ranging from 352 to 441 amino acids [26] [24]. The 4R tau isoforms exhibit greater microtubule-binding affinity compared to 3R isoforms, and their balanced expression is crucial for neuronal health [26]. During development, a transition occurs where fetal brain expresses only the shortest 0N3R isoform, while adult brain maintains a nearly equal ratio of 3R and 4R isoforms, with regional variations in distribution [26] [24].
In the peripheral nervous system (PNS), tau transcript incorporates an additional exon, 4a, generating a high molecular weight isoform termed "Big tau" [26]. This isoform, with its elongated N-terminal domain, is believed to provide enhanced structural stability to long peripheral axons subject to significant mechanical stress and to facilitate the high rates of axonal transport characteristic of these neurons [26]. Its unique structure may also confer reduced propensity for pathological aggregation [26].
Table 1: Major Tau Isoforms in the Human Nervous System
| Isoform Name | N-Terminal Inserts | Microtubule-Binding Repeats | Primary Expression Context | Functional Notes |
|---|---|---|---|---|
| 0N3R | 0 | 3 | Fetal Brain, Adult CNS | Shortest isoform; developmental regulation |
| 1N3R | 1 | 3 | Adult CNS | --- |
| 2N3R | 2 | 3 | Adult CNS | --- |
| 0N4R | 0 | 4 | Adult CNS | Higher microtubule affinity |
| 1N4R | 1 | 4 | Adult CNS | Higher microtubule affinity |
| 2N4R | 2 | 4 | Adult CNS | Higher microtubule affinity; less abundant |
| Big Tau | Extended (Exon 4a) | 4 | Peripheral Nervous System (PNS) | Enhanced mechanical stability |
Beyond its canonical role in microtubule stabilization, tau participates in other cellular processes. It can regulate axonal transport by influencing the attachment and detachment of motor proteins like kinesin and dynein [26]. Tau also localizes to pre- and post-synaptic structures and the nucleus, suggesting additional non-microtubule-related functions [26]. Under physiological conditions, tau's intrinsically disordered nature allows it to adopt a "paperclip" conformation, where its N- and C-termini interact with the mid-domain, a state modulated by post-translational modifications [26].
α-Synuclein: A Multifunctional Synaptic Regulator
Alpha-synuclein (α-syn) is a 140-amino-acid, natively unfolded protein highly enriched at presynaptic terminals [29] [27]. Its primary physiological functions center on synaptic vesicle trafficking, neurotransmitter release, and the maintenance of synaptic vesicle pools [27]. α-Syn interacts with synaptic vesicles to promote their clustering and modulates the assembly of the SNARE (soluble N-ethylmaleimide-sensitive factor attachment protein receptor) complex, which is essential for synaptic vesicle exocytosis [27]. This role in facilitating efficient synaptic transmission underscores its importance in neuronal communication. Furthermore, α-syn's ability to bind lipids allows it to participate in regulating membrane curvature and lipid metabolism [27].
Neurofilaments: The Structural Scaffold
Neurofilaments are the intermediate filaments of neurons, forming a stable, flexible network that provides crucial structural support and determines axonal caliber [24]. Composed of polypeptide subunits (NF-L, NF-M, NF-H), they assemble into heteropolymers that exhibit high tensile strength and resistance to mechanical stress [23] [24]. Unlike the highly dynamic microtubules and actin filaments, neurofilaments are more stable, forming a robust scaffold that maintains the structural integrity of elongated axons and facilitates the efficient conduction of electrical impulses [23] [24].
Pathological Transitions: From Functional Protein to Cytoskeletal Toxin
Tau Misfolding, Hyperphosphorylation, and Microtubule Dissociation
The pathological transformation of tau from a stabilizing MAP to a toxic entity is a multi-step process. A critical initiating event is its abnormal post-translational modification, particularly hyperphosphorylation [24] [25]. In Alzheimer's disease (AD) and other tauopathies, tau undergoes site-specific hyperphosphorylation within its microtubule-binding domain, reducing its affinity for microtubules and leading to its dissociation [24] [25]. This liberation of tau from microtubules has two catastrophic consequences: the destabilization of microtubule networks, which disrupts axonal transport, and the accumulation of free, phosphorylated tau in the cytosol [24] [25].
Once dissociated, hyperphosphorylated tau undergoes a conformational change, misfolding and self-assembling into toxic oligomers, which subsequently aggregate into larger, insoluble structures known as paired helical filaments (PHFs) and straight filaments (SFs) [29] [24]. These filaments are the primary constituents of neurofibrillary tangles (NFTs), a defining histopathological hallmark of AD [24]. The accumulation of tau pathology, as described by Braak staging, closely parallels the trajectory of cognitive decline and brain atrophy in AD, positioning it as a central executor of neurodegeneration [24] [25]. The prion-like propagation of pathological tau between cells further accelerates the spread of pathology throughout connected brain networks [24].
α-Synuclein Aggregation and Strain Heterogeneity
Similar to tau, α-synuclein is prone to pathological transformation. Under stress conditions or due to genetic mutations, natively unfolded α-syn monomers undergo a conformational shift, forming β-sheet-rich oligomers and ultimately progressing into insoluble fibrils [29] [27]. These aggregates are the primary components of Lewy bodies (LBs) and Lewy neurites, the pathological hallmarks of PD and other synucleinopathies [27] [28]. A groundbreaking discovery in the field is the existence of distinct α-synuclein "strains"—structurally unique fibril polymorphs that are associated with different disease phenotypes and seeding properties [29].
Recent cryogenic electron microscopy (cryo-EM) studies have revealed a specific α-syn fibril polymorph, termed "strain B," which possesses a unique core structure that incorporates both the N- and C-termini of the protein (residues 14-22 and 105-115, respectively) [29]. This strain demonstrates a remarkable propensity to cross-seed and promote the aggregation of tau protein, both in neuronal cultures and in vitro, providing a structural basis for the co-occurrence of these pathologies [29]. The C-terminal domain of α-syn (residues 105-115) appears critical for this interaction, suggesting it presents a novel interface for direct interaction with tau [29].
Table 2: Characteristics of Pathological Alpha-Synuclein Strains
| Strain Feature | Strain A | Strain B |
|---|---|---|
| Primary Seeding Preference | α-Synuclein aggregation | Tau co-aggregation |
| Core Structure (Residues) | 38-97 | 14-22, 37-100, 105-115 |
| Fibril Core Size | Smaller, classic wild-type | Largest reported α-syn structure |
| Terminal Involvement | Not incorporated into core | N- and C-termini form part of ordered core |
| Biological Consequence | Traditional synucleinopathy | Mixed proteinopathy, promotes tau pathology |
Synergistic Toxicity: Cross-Seeding and Co-Aggregation
The interplay between tau and α-synuclein extends beyond mere coexistence; they engage in a synergistic relationship that exacerbates neurodegeneration. These proteins can directly interact and promote each other's aggregation through cross-seeding, where fibrils of one protein can act as a template to accelerate the misfolding and aggregation of the other [27] [28]. This cross-talk creates a deleterious feed-forward loop, significantly amplifying the burden of pathological aggregates beyond what either protein could achieve independently [28]. This synergy is a key feature of mixed dementias, such as Alzheimer's disease with Lewy bodies, and contributes to more rapid and aggressive disease progression [27] [28].
The molecular basis for this interaction is being unraveled. As mentioned, the unique structure of α-syn "strain B" facilitates tau aggregation [29]. Furthermore, the co-localization of tau and α-syn within the same cellular inclusions, such as Lewy bodies, has been consistently observed in post-mortem brain tissue, and mass spectrometry has identified tau as a component of LBs [27] [28]. This co-aggregation potentiates neurotoxicity by disrupting mutual physiological functions and overwhelming the cell's proteostatic clearance mechanisms, including the ubiquitin-proteasome system and the autophagy-lysosomal pathway [27].
Experimental Methodologies for Investigating Protein-Cytoskeleton Interactions
Structural Elucidation of Pathological Aggregates
Cryogenic Electron Microscopy (cryo-EM) for Atomic-Level Structural Determination
Cryo-EM has become an indispensable tool for determining the high-resolution structures of pathological protein aggregates, such as tau filaments and α-synuclein fibrils [29]. The following protocol outlines the key steps for structural determination of α-synuclein fibrils:
- Fibril Preparation and Purification: Recombinant α-synuclein is expressed and purified. Fibrillization is induced by incubating monomeric α-synuclein with constant agitation. Distinct strains (e.g., Strain A and B) can be generated through successive seeding generations [29].
- Grid Preparation and Vitrification: A purified fibril sample is applied to a cryo-EM grid (e.g., a holey carbon grid). Excess liquid is blotted away, and the grid is rapidly plunged into a cryogen (liquid ethane) to vitrify the sample, preserving its native state in a thin layer of amorphous ice [29].
- Data Collection: The vitrified grid is loaded into a high-end cryo-electron microscope (e.g., a 300 keV Titan Krios). Thousands of micrographs are collected automatically at a high magnification (e.g., 81,000x) under low-dose conditions to minimize radiation damage [29].
- Image Processing and Helical Reconstruction:
- Particle Picking: Fibril segments ("particles") are manually or automatically selected from the micrographs. For example, one study picked 46,626 fibril segments from 2,934 micrographs [29].
- 2D Classification: Particles are classified based on similar features to identify homogeneous groups and remove junk particles.
- Initial Model Generation and 3D Refinement: An initial 3D model is generated and used as a reference for iterative rounds of 3D classification and helical refinement using software suites like RELION. This yields a high-resolution 3D density map [29].
- Atomic Model Building and Refinement: An atomic model is built into the resolved density map using tools like Coot and refined against the map using programs like Phenix [29].
In Vitro Cross-Seeding Assays Using Thioflavin T (ThT) Fluorescence
Thioflavin T (ThT) fluorescence assays are a standard method to quantitatively monitor the kinetics of protein aggregation and cross-seeding in real-time [29].
- Reagent Preparation: Prepare purified monomeric proteins (e.g., tau 2N4R, α-synuclein). Pre-formed fibrils (PFFs) of the "seeding" protein are sonicated to generate short fragments.
- Assay Setup: In a quartz cuvette or multi-well plate, mix the monomeric "substrate" protein with ThT dye in a suitable buffer. For cross-seeding experiments, add PFFs of the "seeder" protein (e.g., α-syn Strain B) to the reaction. Include control groups with monomers alone and seeds alone.
- Fluorescence Measurement: Load the plate into a fluorescence plate reader. Set the excitation wavelength to ~440 nm and emission to ~480 nm. Incubate the reaction at 37°C with continuous shaking, taking fluorescence measurements at regular intervals.
- Data Analysis: Plot fluorescence intensity over time to generate aggregation kinetics curves. A characteristic sigmoidal curve is observed, with a lag phase (nucleation), growth phase (elongation), and plateau phase (saturation). Cross-seeding by an active strain (like α-syn Strain B) is indicated by a significant shortening of the lag phase and an increase in the final fluorescence intensity compared to controls [29].
The Scientist's Toolkit: Key Research Reagents and Models
Table 3: Essential Research Tools for Investigating Cytoskeletal Proteinopathies
| Tool / Reagent | Function/Application | Key Characteristics / Examples |
|---|---|---|
| Pre-Formed Fibrils (PFFs) | Seeding agents to induce aggregation in cell/animal models. | Sonicated α-syn or tau fibrils; distinct strains (e.g., α-syn Strain B for tau cross-seeding). |
| Thioflavin T (ThT) | Fluorescent dye for monitoring aggregation kinetics. | Binds to β-sheet-rich structures; increased fluorescence indicates fibril formation. |
| Primary Neuronal Cultures | Physiologically relevant in vitro system for studying toxicity. | Mouse or rat cortical/hippocampal neurons; can be seeded with PFFs. |
| Cryo-Electron Microscopy | High-resolution structural biology technique. | Determines atomic structures of fibrils (e.g., α-syn Strain B at 2.6 Å). |
| Transgenic Mouse Models | In vivo modeling of proteinopathy and cytoskeletal defects. | Express human mutant tau (e.g., P301L) or α-syn (e.g., A53T); model propagation. |
| Proteomics Platforms (SomaScan, Olink) | High-dimensional biomarker discovery in biofluids. | Measures ~7,000 proteins; identifies disease-specific signatures (GNPC consortium) [10]. |
Figure 1: Pathological Cascade of Tau and α-Synuclein Interaction. This diagram illustrates the synergistic relationship between tau and α-synuclein in driving neurodegeneration. Initial pathological triggers lead to the misfolding of both proteins. Critically, specific α-synuclein strains can directly cross-seed tau aggregation, creating a feed-forward loop that leads to co-aggregation, cytoskeletal collapse, and eventual neuronal death.
Therapeutic Implications and Future Directions
Targeting Cytoskeletal Integrity and Protein Aggregation
The understanding of tau and α-synuclein interactions with the cytoskeleton opens multiple avenues for therapeutic intervention. One strategic approach is to directly stabilize the microtubule network. Microtubule stabilizers, such as those used in cancer therapy (e.g., taxanes), or brain-penetrant derivatives like TPI-287, have been explored in clinical trials for AD and related tauopathies [23]. These compounds aim to compensate for the loss of stabilizing function caused by tau dissociation, thereby restoring axonal transport and neuronal health [23] [24].
A second, highly active area of research involves developing inhibitors that specifically target the pathogenic aggregation and cross-seeding processes. Based on the atomic structure of α-synuclein Strain B, researchers have designed peptide inhibitors that target the critical C-terminal domain (D105-E115), which is essential for its interaction with tau [29]. These inhibitors have shown promise in mitigating co-aggregation in experimental models [29]. Other strategies include small molecules like CT1812, which is designed to displace toxic protein oligomers (including both Aβ and α-syn) from synapses, and is currently in Phase 2 clinical trials for Alzheimer's disease and dementia with Lewy bodies (DLB) [30].
Furthermore, the shared genetic risk factors, such as the MAPT H1 haplotype which increases risk for both tauopathies and synucleinopathies, provide additional targets for disease-modifying therapies [28]. The growing recognition of mixed pathologies also underscores the need for therapeutic strategies that can simultaneously address multiple aggregating proteins [31] [30].
Consortium-Based Science and Biomarker Discovery
The complexity of these neurodegenerative diseases necessitates large-scale, collaborative efforts. The Global Neurodegeneration Proteomics Consortium (GNPC) represents a paradigm shift in this regard, having established one of the world's largest harmonized proteomic datasets [10]. This resource, which includes approximately 250 million unique protein measurements from over 35,000 biofluid samples, empowers the discovery of disease-specific and transdiagnostic proteomic signatures [10]. Such large-scale biomarker discovery is crucial for improving early detection, patient stratification, and the development of precision medicine approaches for clinical trials [10] [30].
Table 4: Selected Therapeutic Candidates Targeting Protein Aggregation and Cytoskeletal Defects
| Therapeutic Candidate / Approach | Proposed Mechanism of Action | Current Development Stage | Relevant Disease Context |
|---|---|---|---|
| Microtubule Stabilizers | Compensate for loss of tau function, restore axonal transport. | Preclinical / Early Clinical Trials | Alzheimer's disease, Tauopathies [23] |
| CT1812 | Displaces toxic Aβ and α-syn oligomers from synapses. | Phase 2 Clinical Trials | Alzheimer's disease, Dementia with Lewy Bodies [30] |
| α-Syn C-Terminal Peptide Inhibitors | Blocks α-syn (Strain B) interaction with tau. | Preclinical (Structure-Based Design) | Mixed Proteinopathies, PD/AD co-pathology [29] |
| Anti-tau Immunotherapies | Promote clearance of extracellular pathological tau. | Phase 2/3 Clinical Trials | Alzheimer's disease, Progressive Supranuclear Palsy |
| Levetiracetam (Repurposed) | Suppresses aberrant neuronal activity; may slow brain atrophy in an APOE ε4-stratified population. | Phase 2 Clinical Trials | Alzheimer's disease (MCI) [30] |
The intricate interplay between tau, α-synuclein, and the neuronal cytoskeleton represents a core mechanism driving neurodegeneration. The pathological synergy between these proteins, culminating in cytoskeletal collapse and a "dying back" pattern of degeneration, provides a unifying framework for understanding a spectrum of neurodegenerative diseases. Future research, leveraging structural biology, consortium-scale datasets, and therapeutic strategies targeting both protein aggregation and cytoskeletal resilience, holds the promise of effective precision interventions for these devastating disorders.
The neuronal cytoskeleton, a complex network of microtubules, neurofilaments, and actin filaments, is fundamental to maintaining structural integrity, enabling intracellular transport, and ensuring proper synaptic function. In neurodegenerative diseases, genetic mutations disrupting this delicate architecture provide compelling evidence for the central role of cytoskeletal defects in disease pathogenesis. This whitepaper synthesizes genetic evidence linking specific mutations in cytoskeletal genes to three prominent neurodegenerative disorders: Amyotrophic Lateral Sclerosis (ALS), Charcot-Marie-Tooth disease (CMT), and Frontotemporal Dementia with Parkinsonism linked to chromosome 17 (FTDP-17). By examining mutations in genes encoding neurofilament proteins (ALS), peripheral neurofilaments (CMT), and microtubule-associated proteins (FTDP-17), we aim to establish a unified understanding of how cytoskeletal disruptions drive neurodegeneration, offering insights for targeted therapeutic development.
Genetic Landscape of Cytoskeletal Mutations
Table 1: Summary of Key Cytoskeletal Gene Mutations in Neurodegenerative Diseases
| Disease | Gene/Protein | Mutation Types & Examples | Primary Cytoskeletal Component Affected | Functional Consequence |
|---|---|---|---|---|
| ALS | NEFL (Neurofilament Light Chain) [32] | Not Specified | Type IV Intermediate Filaments | Disrupted axonal transport, neurofilament aggregation, impaired structural stability |
| CMT2E | NEFL (Neurofilament Light Chain) [33] | Missense (e.g., p.N98S) | Type IV Intermediate Filaments | Gain-of-function, abnormal aggregation, impaired axonal transport |
| FTDP-17 | MAPT (Microtubule-Associated Protein Tau) [34] [35] [36] | >50 pathogenic mutations (e.g., P301L, intronic splice-site mutations) | Microtubules | Reduced microtubule binding, altered 3R:4R tau isoform ratio, hyperphosphorylation, tau aggregation |
Amyotrophic Lateral Sclerosis (ALS): Neurofilament Disruption and Axonal Transport Failure
Genetic Evidence and Pathogenic Mechanisms
In ALS, the neurofilament protein light chain (NEFL) gene is critically implicated. Neurofilaments, belonging to the type IV intermediate filament family, form the primary structural scaffold for axons and are essential for maintaining axonal caliber, which in turn facilitates efficient axonal transport [32]. Under pathological conditions, mutations in NEFL lead to a cascade of failures: the neurofilaments detach from axons, undergo abnormal aggregation, and cause a profound disruption in axonal transport [32]. The detection of elevated levels of neurofilament subunits, particularly the neurofilament light chain (NFL), in the cerebrospinal fluid (CSF) and blood of ALS patients underscores the ongoing axonal damage. The concentration of these subunits shows a significant positive correlation with disease progression, establishing NFs as a promising early diagnostic and prognostic biomarker [32].
Key Experimental Protocols for ALS Research
Protocol 1: Quantifying Neurofilament Light Chain (NFL) in Biofluids
- Sample Collection: Collect cerebrospinal fluid (CSF) and plasma samples from ALS patients and matched controls.
- Detection Assay: Utilize ultrasensitive immunoassay platforms, such as the Single Molecule Array (Simoa) technology, to quantify NFL levels [32].
- Data Analysis: Correlate NFL concentrations with clinical measures of disease progression (e.g., ALSFRS-R score) using statistical models (e.g., linear regression) to validate its utility as a biomarker.
Protocol 2: Modeling NEFL Aggregation in Cellular Systems
- Cell Culture: Maintain motor neuron-like cell lines (e.g., NSC-34) or use patient-derived induced pluripotent stem cells (iPSCs).
- Transfection: Introduce mutant NEFL genes (e.g., disease-associated variants) into the cells using lentiviral transduction.
- Phenotypic Analysis:
- Immunocytochemistry: Stain cells with antibodies against NFL and observe aggregation patterns via confocal microscopy.
- Protein Solubility Assay: Perform sequential protein extraction to separate soluble and insoluble protein fractions, followed by Western blotting to quantify aggregated NFL.
Charcot-Marie-Tooth Disease Type 2E (CMT2E): A Gain-of-Function Neurofilopathy
Genetic Evidence and Pathogenic Mechanisms
CMT2E, an axonal form of Charcot-Marie-Tooth disease, is caused by dominant mutations in the NEFL gene. A key mechanistic insight comes from the specific p.N98S (Asn98Ser) missense mutation, which acts through a heterozygous gain-of-function mechanism [33]. This mutation leads to the expression of a toxic protein that disrupts the normal assembly and function of the neurofilament network within peripheral nervous system axons. The resultant pathology includes abnormal aggregation of neurofilaments and impaired axonal transport, ultimately triggering axonal degeneration, which is the hallmark of CMT2E [33].
Key Experimental Protocols for CMT2E Research
Protocol: Testing Antisense Oligonucleotide (ASO) Therapy in a CMT2E Model
- Disease Modeling: Generate a patient-specific model using induced pluripotent stem cells (iPSCs) derived from CMT2E patients carrying the p.N98S mutation. Differentiate these iPSCs into motor neurons [33].
- Therapeutic Agent Design: Design and synthesize custom antisense oligonucleotides (ASOs) that specifically target the mutant NEFL mRNA for degradation, while sparing the wild-type allele [33].
- Treatment: Apply the ASO to the CMT2E iPSC-derived motor neurons.
- Efficacy Assessment:
- Molecular Readout: Use qPCR and Western blot to measure the reduction in mutant NEFL mRNA and protein levels.
- Phenotypic & Biomarker Readout: Quantify the reduction of axonal degeneration biomarkers (e.g., total NFL levels in culture supernatant) and assess improvements in neuronal morphology and survival [33].
FTDP-17: Microtubule Dysregulation and Tau Toxicity
Genetic Evidence and Pathogenic Mechanisms
FTDP-17 is an autosomal dominant disorder unequivocally caused by mutations in the MAPT gene encoding the microtubule-associated protein tau [35] [36]. Over 50 pathogenic mutations have been identified, which primarily fall into two mechanistic categories, as detailed in Table 2.
Table 2: Pathogenic Mechanisms of MAPT Mutations in FTDP-17
| Mutation Group | Genomic Location | Key Examples | Primary Molecular Effect | Downstream Pathogenic Consequence |
|---|---|---|---|---|
| Coding Region Mutations | Exons (esp. in microtubule-binding domain) | P301L, R406W | Disrupts tau binding to microtubules, reduces microtubule stability | Increased free tau, accelerated tau aggregation into filaments [36] |
| Splicing Mutations | Introns near exon 10; Exon 10 itself | +16, N279K, P301L | Alters splicing regulation of exon 10 | Imbalanced 3-repeat (3R) to 4-repeat (4R) tau isoform ratio (typically increased 4R tau) [36] |
A conserved in vivo mechanism across different FTDP-17 tau mutations involves enhanced phosphorylation of tau. This hyperphosphorylation leads to excessive stabilization of the actin cytoskeleton, which is a critical mediator of neurotoxicity. This cascade subsequently dysregulates key cellular pathways, including autophagy and the unfolded protein response, culminating in neuronal death [34].
Key Experimental Protocols for FTDP-17 Research
Protocol 1: Drosophila Model for Tau-Mediated Neurotoxicity
- Animal Model Generation: Use site-directed phiC31 integrase-mediated cassette exchange to generate Drosophila lines expressing equivalent levels of wild-type human tau or various FTDP-17 mutant tau (e.g., P301L) to ensure controlled comparison [34].
- Phenotypic Screening:
- Neurodegeneration Assay: Perform histological analysis of fly brains using markers like vacuolization.
- Behavioral Assay: Test locomotor function using climbing assays.
- Biochemical Analysis: Examine tau phosphorylation status via Western blot with phospho-specific tau antibodies. Assess actin cytoskeletal stabilization using biochemical methods [34].
Protocol 2: Investigating the Role of Microglial TREM2 in Tau Pathology
- Cell System: Use microglial cell lines or primary microglia.
- Intervention: Modulate TREM2 function using agonistic antibodies (e.g., AL002) or by knocking down TREM2 expression [37].
- Functional Assays:
- Phagocytosis Assay: Incubate microglia with fluorescently-labeled tau fibrils and measure uptake via flow cytometry or microscopy.
- Cytokine Profiling: Use ELISA to measure the production of inflammatory cytokines (e.g., TNF-α, IL-1β) upon TREM2 activation in the presence of tau [37].
Integrated Signaling Pathways in Cytoskeletal Neurodegeneration
The following diagram synthesizes the core signaling pathways and pathological interactions between key proteins discussed in this whitepaper, illustrating the convergent mechanisms of cytoskeletal failure.
The Scientist's Toolkit: Key Research Reagents and Models
Table 3: Essential Research Tools for Investigating Cytoskeletal Neurodegeneration
| Reagent/Model | Specific Example | Application & Function | Relevant Disease |
|---|---|---|---|
| Patient-derived iPSCs | iPSCs from CMT2E (p.N98S) patient [33] | Provides a human-specific in vitro model for pathomechanism studies and drug screening. | CMT, ALS |
| Site-directed Transgenic Models | Drosophila with phiC31-integrated human tau [34] | Ensures controlled, equivalent expression of transgenes for robust phenotype comparison. | FTDP-17 |
| Antisense Oligonucleotides (ASOs) | NEFL p.N98S-targeting ASO [33] | Targets mutant mRNA for degradation in allele-specific manner; a therapeutic and research tool. | CMT2E |
| Ultra-sensitive Detection Assays | Single Molecule Array (Simoa) [32] | Quantifies low-abundance biomarkers (e.g., NFL) in biofluids for diagnosis and monitoring. | ALS, CMT |
| Agonistic Antibodies | TREM2 agonist (e.g., AL002) [37] | Research tool to probe TREM2 pathway function and its impact on microglial phagocytosis. | FTDP-17, ALS |
The genetic evidence from ALS, CMT, and FTDP-17 paints a convergent picture: disruptions to the core components of the neuronal cytoskeleton—whether neurofilaments or microtubule-associated proteins—are a primary driver of neurodegeneration. A critical emerging concept is that of "co-proteinopathy," where multiple pathological protein aggregates (e.g., tau, TDP-43) can coexist, interact, and synergistically drive disease progression, challenging the traditional single-protein paradigm [38]. This underscores the complexity of the pathological landscape.
Therapeutic strategies are evolving to meet this challenge. For monogenic disorders like CMT2E caused by specific gain-of-function mutations, allele-specific silencing with ASOs represents a highly promising precision medicine approach [33]. For pathways involving non-cell autonomous mechanisms, targeting regulators of neuroinflammation, such as TREM2 signaling to enhance microglial protective functions, offers a complementary strategy [37]. Future research must leverage advanced in vitro models that better recapitulate human co-proteinopathy and continue to develop multi-target therapeutic strategies aimed at restoring cytoskeletal integrity and overall protein homeostasis in the nervous system.
Research Tools and Therapeutic Strategies Targeting Cytoskeletal Pathology
Neurofilament Light Chain (NfL) has emerged as a premier fluid biomarker for detecting and quantifying neuroaxonal injury across a wide spectrum of neurological conditions. As a key structural component of the neuronal cytoskeleton, NfL provides critical insights into neurodegenerative mechanisms central to cytoskeletal defect research. The quantification of NfL in cerebrospinal fluid (CSF) and blood represents a significant advancement in neurodiagnostics, offering a sensitive, dynamic, and accessible means to track disease progression, therapeutic response, and prognostic outcomes [39] [40].
Technological innovations in immunoassay platforms, particularly the development of single-molecule array (Simoa) technology, have enabled reliable quantification of NfL at low-pg/mL concentrations in blood, facilitating its transition from specialized research to broader clinical applications [39] [41]. This guide provides researchers and drug development professionals with a comprehensive technical overview of NfL as a cytoskeletal biomarker, encompassing its molecular biology, analytical methodologies, clinical validations, and implementation in therapeutic development.
Molecular Biology and Pathophysiological Significance
Structural Properties and Biological Function
Neurofilaments are class IV intermediate filaments that constitute the primary structural components of the neuronal cytoskeleton. They are heteropolymers composed of four subunits: neurofilament light chain (NfL, 68-70 kDa), medium chain (NfM, 145-160 kDa), heavy chain (NfH, 200-220 kDa), and either α-internexin (in the central nervous system) or peripherin (in the peripheral nervous system) [39] [40]. The NfL subunit is transcribed from the Neurofilament Light Polypeptide (NEFL) gene located on chromosome 8 (8p21.2) and serves as the backbone for neurofilament assembly [40].
Functionally, NfL supports the radial expansion of large myelinated axons, facilitating high-velocity nerve conduction. Recent evidence also suggests NfL presence in synaptic terminals in oligomeric form, potentially influencing synaptic plasticity and NMDAR-GluN1 expression [40]. Mutations in the NEFL gene are known to cause nerve damage disorders such as Charcot-Marie-Tooth disease, underscoring its critical role in maintaining axonal integrity [40].
Release Mechanisms and Pathological Significance
Under physiological conditions, neurofilaments exhibit high stability and slow turnover in mature neuronal cytoplasm [40]. However, during neuroaxonal damage, the neuronal membrane is disrupted, activating calpain-driven proteolysis that cleaves neurofilaments and releases NfL fragments into the extracellular space [42]. These fragments subsequently diffuse into CSF and blood, with CSF concentrations approximately 40-fold higher than blood levels [40].
Recent research indicates that released NfL is not merely a bystander biomarker but may actively participate in neuroinflammatory pathways. Secreted NfL can activate microglial cells, promoting cytokine release that contributes to disease pathology—a process that can be blocked with anti-NfL antibodies [42]. In SOD1 mouse models of amyotrophic lateral sclerosis (ALS), NfL knockout ameliorated microgliosis and delayed symptom onset, suggesting NfL may itself be a therapeutic target [42].
Table 1: Neurofilament Isoforms and Their Characteristics
| Isoform | Molecular Weight | Primary Location | Functional Role |
|---|---|---|---|
| NfL (Light Chain) | 68-70 kDa | CNS & PNS | Structural backbone for neurofilament assembly, radial axonal expansion |
| NfM (Medium Chain) | 145-160 kDa | CNS & PNS | Intermediate filament organization, axonal caliber maintenance |
| NfH (Heavy Chain) | 200-220 kDa | CNS & PNS | Cross-linking filaments, mechanical stability |
| α-internexin | 58-66 kDa | Central Nervous System (CNS) | Neuronal development, structural support |
| Peripherin | 57-59 kDa | Peripheral Nervous System (PNS) | Structural integrity of peripheral neurons |
Diagram Title: NfL Release Mechanism Following Neuronal Injury
Analytical Methodologies and Technical Considerations
Immunoassay Platforms for NfL Quantification
The evolution of immunoassay technologies has been instrumental in enabling precise NfL measurement in biological fluids. Current platforms offer varying levels of sensitivity, precision, and throughput suitable for different research and clinical applications.
Table 2: Analytical Platforms for NfL Quantification
| Platform/Manufacturer | Technology | Assay Range (pg/mL) | Limit of Detection (pg/mL) | Precision (%CV) | Matrices |
|---|---|---|---|---|---|
| Simoa HD-X Analyzer (Quanterix) | Digital ELISA | 0.5-500 | 0.085 | Intra-assay: <4.63%\nInter-assay: <8.46% | Serum, EDTA Plasma, CSF |
| Lumipulse G1200 (Fujirebio) | CLIA | 5.5-5000 | 3.0 | Intra-assay: <3.25%\nInter-assay: <5.50% | Serum, K₂EDTA Plasma, Li Hep Plasma, CSF |
| Cobas 8000 e 801 (Roche) | ECLIA | 0.168-1000 | 0.140 | Intra-assay: <5.2%\nInter-assay: <7.2% | Serum, Plasma, CSF |
| Atellica IM Analyzer (Siemens) | CLIA | 1-646 | 1.3 | Intra-assay: <6.4%\nInter-assay: <12.4% | Serum, EDTA Plasma |
The single-molecule array (Simoa) technology represents a significant advancement, utilizing miniaturized microwells and nanobeads that capture immunocomplexes to detect positivity signals even with minimal neurofilament molecules present [39]. This ultra-sensitivity enables reliable blood-based measurement, circumventing the need for invasive lumbar punctures in many applications.
Pre-analytical and Analytical Considerations
Blood NfL demonstrates good stability under various pre-analytical conditions, showing limited effects from multiple freeze-thaw cycles and prolonged exposure to room temperature [40]. Comparative studies indicate strong correlations between EDTA plasma and serum measurements, though plasma levels are approximately 20% lower [40]. Intra-individual variation of NfL measurements in stable conditions is minimal, with a mean coefficient of variation of approximately 7.4% between repeated measures [40].
Critical factors influencing NfL interpretation include:
- Age: Strong positive correlation with advancing age in both healthy and pathological states [43]
- Renal function: Impaired glomerular filtration rate affects NfL clearance [44]
- Body mass index (BMI): Inverse relationship with NfL levels [44]
- Matrix selection: Serum versus plasma considerations [40]
No significant biorhythmic fluctuations have been observed, allowing flexibility in sampling timing without affecting results [40].
Clinical Validations Across Neurological Disorders
Diagnostic and Prognostic Utility in Neurodegenerative Diseases
Multiple System Atrophy (MSA)
A prospective cohort study demonstrated that serum NfL levels effectively discriminate between MSA, Parkinson's disease (PD), and healthy controls. With cutoff values of 223.5 pg/mL for differentiating MSA from PD (AUC = 0.930) and 218.0 pg/mL for distinguishing MSA-parkinsonism subtypes from PD (AUC = 0.878), NfL exhibits robust diagnostic performance in early disease stages [45]. Furthermore, elevated baseline NfL levels independently predicted shorter time to poor prognosis and death, with orthostatic hypotension associated with higher mortality risk [45].
Parkinson's Disease (PD)
The ParkWest longitudinal study revealed that serum NfL is elevated in newly diagnosed PD patients compared to controls at all timepoints, with a faster annual increase over 5 years (0.09 pg/mL per year; p = 0.029) [43]. Higher baseline NfL predicted faster cognitive decline (β -0.77 transformed MMSE points per year; p = 0.010), while a 40% increase in NfL predicted future motor decline (β 0.28 UPDRS-III; p = 0.004) [43].
Alzheimer's Disease (AD) and Cognitive Decline
Plasma NfL demonstrates strong associations with global cognition (β = -1.28; P < 0.001) and specific cognitive domains including memory, language, praxis, and executive functions in neurodegenerative diseases [44]. As part of the AT(N) framework, NfL serves as the "N" indicator of neurodegeneration, complementing amyloid-β (A) and tau (T) biomarkers to enhance disease staging and prognostication [41]. Longitudinal studies show NfL elevations begin 10-20 years before symptom onset in autosomal-dominant AD, with CSF levels continuing to rise post-clinically while plasma levels stabilize [41].
Table 3: Clinically Validated NfL Cut-off Values Across Disorders
| Disorder | Clinical Context | Cut-off Value | AUC | Sensitivity/Specificity | Citation |
|---|---|---|---|---|---|
| Multiple System Atrophy | vs. Parkinson's Disease | 223.5 pg/mL | 0.930 | Not specified | [45] |
| MSA-Parkinsonism Subtype | vs. Parkinson's Disease | 218.0 pg/mL | 0.878 | Not specified | [45] |
| Hereditary Transthyretin Amyloidosis | Healthy carriers vs. Symptomatic patients | 7.9 pg/mL | 0.847 | Sensitivity: 90.0%\nSpecificity: 55.0% | [46] |
| Hereditary Transthyretin Amyloidosis | PND I vs. PND ≥ II | 18.4 pg/mL | 0.695 | Sensitivity: 67.0%\nSpecificity: 86.0% | [46] |
Applications in Non-Neurodegenerative Conditions
Beyond classical neurodegeneration, NfL exhibits utility across diverse neurological conditions including multiple sclerosis (MS), hereditary transthyretin amyloidosis (ATTRv), and psychiatric disorders.
In multiple sclerosis, serum NfL correlates with inflammatory activity and disease progression, detecting subclinical axonal damage that can inform therapeutic decision-making [47]. A consensus from the Spanish Society of Neurology recommends incorporating sNfL measurement into routine practice alongside clinical evaluation and MRI [47].
For hereditary transthyretin amyloidosis, serum NfL accurately distinguishes between healthy carriers and symptomatic patients, with a proposed cut-off of 7.9 pg/mL (AUC = 0.847) demonstrating 90% sensitivity [46]. Furthermore, increasing NfL levels correlate with functional disability progression measured by Polyneuropathy Disability Score [46].
Emerging evidence in psychiatry indicates blood NfL elevations in major depression, bipolar disorder, psychotic disorders, anorexia nervosa, and substance use disorders compared to physiological states [40]. Potential applications include excluding neurodegenerative disease, assessing pharmacological brain toxicity, and longitudinally monitoring treatment response.
NfL in Therapeutic Development and Clinical Trials
Regulatory Precedents and Clinical Trial Applications
The U.S. Food and Drug Administration (FDA) established a significant regulatory precedent by relying on plasma NfL as a surrogate endpoint reasonably likely to predict clinical benefit in the accelerated approval of tofersen for SOD1-amyotrophic lateral sclerosis (ALS) in 2023 [48]. This decision was supported by: (1) mechanistic evidence that tofersen reduced SOD1 protein; (2) scientific evidence demonstrating the prognostic value of plasma NfL in predicting ALS progression and survival; and (3) observed correlation between NfL reduction and diminished clinical decline [48].
Analysis of Investigational New Drug (IND) programs submitted to FDA between 2005-2024 reveals increasing integration of NfL in therapeutic development. Of 50 identified programs, predominantly from the last five years, 94% (n = 47) proposed NfL as a pharmacodynamic biomarker, 52% (n = 26) for patient stratification, 20% (n = 10) as a surrogate endpoint, and 8% (n = 4) for patient selection [48]. Among programs evaluating NfL as a pharmacodynamic biomarker with available data (n = 21), approximately 50% reported NfL changes correlating with drug exposure [48].
Experimental Protocols for Therapeutic Monitoring
Protocol 1: Longitudinal Serum NfL Monitoring in Neurodegenerative Trials
Sample Collection: Blood collected by standard venipuncture and processed within two hours. Centrifugation at 2000 rpm for 10 minutes at room temperature to obtain serum fraction. Aliquot into cryovials and store at -80°C [46].
NfL Measurement: Utilize SIMOA platform with Human Light Neurofilament (NF-L) Advantage Kit following manufacturer specifications. Perform measurements in duplicate with appropriate calibrators and controls. For multi-center trials, implement cross-platform calibration and standardized protocols to minimize inter-site variability [39] [41].
Timepoints: Baseline, 3 months, 6 months, 12 months, and annually thereafter. More frequent sampling (monthly) may be appropriate for acute interventions or rapidly progressive conditions.
Data Analysis: Adjust for age, renal function, and BMI. Express changes as both absolute concentrations and percent change from baseline. Employ linear mixed-effects models to analyze longitudinal trajectories with appropriate covariance structures.
Protocol 2: NfL-Based Patient Stratification in Early Phase Trials
Inclusion Criteria: Incorporate baseline NfL thresholds for enrollment, such as >90th percentile for age-matched controls for progressive forms of MS or >16.5 pg/mL for Parkinson's disease progression studies [43] [47].
Stratification Approach: Randomize patients according to baseline NfL quartiles to ensure balanced distribution across treatment arms. Pre-specified subgroup analyses based on baseline NfL levels.
Endpoint Integration: Correlate NfL changes with clinical outcomes (e.g., MMSE, UPDRS-III, EDSS) and imaging biomarkers (e.g., MRI volumetry, FDG-PET) [43] [44].
Diagram Title: NfL Biomarker Development Workflow
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Key Research Reagent Solutions for NfL Analysis
| Reagent/Platform | Manufacturer/Provider | Application Context | Technical Specifications | Evidence Level |
|---|---|---|---|---|
| NF-Light Serum ELISA Kit | Uman Diagnostics (Quanterix) | Quantitative NfL measurement in serum/plasma | LOD: 0.4 pg/mL\nInter-precision: <10%\nIntra-precision: <6.6% | Clinical validation in ATTRv, PD, MSA [46] |
| Simoa NF-Light Advantage Kit | Quanterix | Ultra-sensitive NfL measurement in serum/plasma/CSF | LOD: 0.085 pg/mL\nAnalytical range: 0.345-1140 pg/mL | Used in regulatory submissions; multi-center validation [48] [39] |
| Human Anti-NfL Monoclonal Antibodies (Clone 2.1 & 47.3) | Uman Diagnostics | Capture/detection antibodies for immunoassays | Epitope recognition of NfL cleavage products | Reference antibodies used across platforms [39] |
| Lumipulse G NfL Assay | Fujirebio Diagnostics | Automated NfL measurement on Lumipulse platform | LOD: 3.0 pg/mL\nRange: 2.0-5000 pg/mL | Clinical chemistry lab implementation [39] |
| Elecsys Neurofilament Light Chain Assay | Roche Diagnostics | NfL measurement on cobas e801 platform | LOD: 0.140 pg/mL\nRange: 0.168-1000 pg/mL | High-throughput clinical testing [39] |
Neurofilament Light Chain has firmly established itself as a robust biomarker for neuroaxonal injury across the spectrum of neurological diseases. Its integration into the AT(N) framework for Alzheimer's disease and emerging applications in therapeutic development underscore its utility as both a research and clinical tool. The recent regulatory acceptance of NfL as a surrogate endpoint in ALS trials marks a significant milestone in biomarker qualification.
Future developments will focus on standardizing pre-analytical and analytical protocols across platforms, establishing universally applicable reference intervals adjusted for age and comorbidities, and validating clinically actionable decision thresholds. Multi-analyte approaches combining NfL with other biomarkers (e.g., GFAP, tau species) show promise for enhanced diagnostic specificity. Furthermore, research illuminating the active role of secreted NfL in neuroinflammatory pathways may unveil novel therapeutic targets beyond its current biomarker applications.
For researchers and drug development professionals, NfL represents a versatile tool for quantifying neuroaxonal injury, stratifying patient populations, monitoring therapeutic efficacy, and accelerating regulatory approval pathways. As evidence continues to accumulate, NfL measurement is poised to become an integral component of precision neurology, bridging fundamental research on cytoskeletal defects with clinical applications across neurodegenerative disorders.
The neuronal cytoskeleton is a dynamic network essential for maintaining cellular structure, facilitating intracellular transport, and supporting synaptic function. Its integrity is crucial for neuronal health, and its collapse is a central event in numerous neurodegenerative diseases [49] [24]. Microtubules, key components of this cytoskeleton, are hollow filaments composed of α- and β-tubulin heterodimers. They provide structural support and serve as tracks for the intracellular transport of cargoes, such as proteins, organelles, and vesicles, powered by motor proteins like kinesins and dyneins [50] [51]. In the context of neurodegeneration, the microtubule-associated protein tau plays a critical role. Under physiological conditions, tau binds to and stabilizes microtubules, promoting their assembly and maintaining axonal transport [50] [24]. However, in Alzheimer's disease (AD) and related tauopathies, tau becomes hyperphosphorylated, leading to its detachment from microtubules. This loss of functional tau results in microtubule destabilization, impaired axonal transport, and ultimately, the formation of toxic tau aggregates known as neurofibrillary tangles (NFTs) [50] [31] [24]. This cascade directly links cytoskeletal failure to neuronal dysfunction and degeneration, establishing microtubule stabilization as a compelling therapeutic strategy.
The Rationale for Microtubule Stabilization as a Therapeutic Strategy
The hypothesis that exogenous microtubule-stabilizing agents could compensate for the loss of tau function offers a promising disease-modifying approach for neurodegenerative conditions. The foundational premise is that by directly stabilizing the microtubule network, these drugs can restore axonal transport and maintain neuronal health, even in the presence of pathological tau [50] [49].
Key evidence supporting this strategy comes from preclinical models. In vitro, microtubule-stabilizing agents have been demonstrated to protect cultured neurons against both tau- and Aβ-mediated neurotoxicity [50]. The first critical in vivo validation was reported in 2005, where treatment with paclitaxel was shown to restore fast axonal transport and increase microtubule density in the spinal motor neurons of a tau transgenic mouse model. This improvement in axonal physiology correlated with an amelioration of motor deficits [50]. A pivotal observation from these and subsequent studies is that the dose-response relationship for these agents is often U-shaped. Excessively high doses, typical in cancer chemotherapy, lead to toxic over-stabilization of microtubules, causing side effects like peripheral neuropathy. In contrast, very low doses can effectively restore microtubule dynamics and axonal transport to physiological levels, producing optimal therapeutic effects without significant toxicity [50]. This principle underscores the potential for using these agents at non-toxic, low doses for chronic treatment of neurodegenerative diseases.
Classes of Microtubule-Stabilizing Agents and Their Properties
Since the discovery of paclitaxel, a diverse range of natural and synthetic microtubule-stabilizing compounds has been identified. Table 1 summarizes the major classes, their brain penetrance, and their developmental status in the context of neurodegenerative diseases.
Table 1: Classes of Microtubule-Stabilizing Agents
| Compound Class | Representative Agents | Brain Penetrance | Stage of Development for Neurodegeneration |
|---|---|---|---|
| Taxanes | Paclitaxel, Docetaxel, TPI 287 | Generally poor; TPI 287 is brain-penetrant [50] [49] [52] | Paclitaxel showed efficacy in a spinal cord tau model but is unsuitable for brain tauopathies [50]. TPI 287 has been evaluated in clinical trials for tauopathies and glioblastoma [51] [52]. |
| Epothilones | Epothilone D (BMS-241027) | Brain-penetrant [50] | Evaluated in multiple tau transgenic mouse models; advanced to a Phase Ib clinical trial for Alzheimer's disease [50]. |
| Discodermolide | Discodermolide | Not reported | Not reported for neurodegeneration [50]. |
| Laulimalide | Laulimalide, Peloruside | Not reported | Peloruside has been evaluated in cell-based studies [50]. |
Key Compound Profiles
- Taxanes: This class includes the prototypical agent paclitaxel. While pivotal in validating the therapeutic concept, most first-generation taxanes are not brain-penetrant, limiting their utility for central nervous system (CNS) disorders [50] [49]. TPI 287 is a novel taxane derivative specifically designed to overcome this limitation; it is not a substrate for the P-glycoprotein efflux pump and readily accumulates in the brain following intravenous administration [52].
- Epothilones: Epothilone D is a brain-penetrant microtubule stabilizer that has shown significant promise in preclinical studies. Treatment with low, weekly doses in PS19 and rTg4510 tau transgenic mice normalized MT density, restored fast axonal transport, reduced axonal dystrophy, and decreased neuronal loss, leading to improved cognitive performance. These benefits were observed in both preventative and interventional regimens [50].
Preclinical Models and Experimental Outcomes
Preclinical studies using animal models of neurodegeneration have been instrumental in validating the efficacy of microtubule-stabilizing agents.
In Vivo Modeling Protocols
The most robust data come from studies using transgenic mouse models that overexpress human mutant tau, such as the PS19 and rTg4510 lines. These mice develop age-dependent NFT-like tau pathology, neuronal loss, and behavioral deficits, mimicking key aspects of human tauopathies [50].
A typical interventional study protocol involves:
- Animal Subjects: Age-matched transgenic mice and wild-type littermate controls.
- Treatment Administration: Mice are randomly assigned to treatment or vehicle control groups. The test compound (e.g., Epothilone D) is administered systemically (e.g., intraperitoneal injection) at low, weekly doses. Doses are typically set well below the maximum tolerated dose (MTD) used in oncology to avoid toxicity (e.g., 100-fold lower than the cumulative chemotherapeutic dose) [50].
- Duration: Studies can be "preventative" (treatment begins before the onset of overt pathology) or "interventional" (treatment begins after pathology is established) [50].
- Outcome Measures:
- Biochemical & Histopathological Analysis: Post-mortem brain tissue is analyzed for microtubule density (e.g., via immunoblotting or immunohistochemistry for tubulin), tau pathology (e.g., phospho-tau immunohistochemistry), and neuronal loss [50].
- Behavioral Analysis: Cognitive function is assessed using standardized tests like the Morris water maze or contextual fear conditioning to correlate pathological improvements with functional recovery [50].
Key Preclinical Findings
The outcomes from these models have been consistently supportive:
- Microtubule Stabilization: Treatment with brain-penetrant stabilizers like Epothilone D significantly increased the density of stable microtubules in the brains of tau transgenic mice [50].
- Restoration of Axonal Transport: These agents restored fast axonal transport, which is critical for neuronal viability and is impaired in tauopathies [50].
- Reduction of Pathology: Studies reported a reduction in axonal dystrophy and a decrease in the accumulation of pathological tau [50].
- Functional Improvement: The histological and biochemical improvements translated into better cognitive performance in behavioral tasks [50].
The following diagram illustrates the therapeutic mechanism and the experimental workflow used to validate it in preclinical models.
Clinical Trial Outcomes
The transition from preclinical models to human trials has begun, with several agents being evaluated for safety and efficacy in neurodegenerative diseases. Table 2 summarizes the key clinical findings for the most advanced compounds.
Table 2: Clinical Trial Outcomes of Microtubule-Stabilizing Agents in Neurodegeneration
| Agent | Trial Phase | Patient Population | Key Efficacy Outcomes | Key Safety Outcomes |
|---|---|---|---|---|
| Epothilone D (BMS-241027) | Phase Ib [50] | Alzheimer's Disease | Primary objective was safety; efficacy endpoints not publicly detailed in search results. | The trial was initiated based on strong preclinical safety and efficacy [50]. |
| TPI 287 | Phase 1 [52] | Recurrent Glioblastoma (rGBM) | Median PFS: 5.5 months; 6-month PFS: 40%; Median OS: 13.4 months [52]. | Generally well tolerated. Common AEs: fatigue, myelosuppression, peripheral neuropathy. No DLTs observed; MTD not reached [52]. |
| TPI 287 | Clinical Trials (Phase not specified) | Tauopathies (e.g., Alzheimer's, PSP) | Evidence of activity was noted in tauopathy trials [52]. | The drug was generally well tolerated, with dose limitations related to neuropathy [52]. |
Clinical Trial Design and Assessment Protocols
Clinical trials for these agents in neurodegenerative diseases follow rigorous designs. A typical Phase I trial, such as the one for TPI 287 in rGBM, employs a standard 3 + 3 dose-escalation scheme to determine the maximum tolerated dose (MTD) and safety profile [52].
- Patient Population: Adults with confirmed diagnosis (e.g., rGBM), adequate organ function, and a defined number of prior therapy lines. Key exclusion criteria often include prior exposure to similar drug classes (e.g., anti-angiogenics or other microtubule inhibitors) and pre-existing peripheral neuropathy [52].
- Dosing Regimen: The investigational drug (e.g., TPI 287) is administered intravenously on a set schedule (e.g., every 3 weeks). In combination trials, it is given alongside a standard therapy like bevacizumab [52].
- Primary Endpoint: Safety and the determination of the MTD. Dose-limiting toxicities (DLTs) are rigorously defined (e.g., grade 4 myelosuppression, grade ≥3 non-hematologic toxicity) and assessed during the first treatment cycle [52].
- Secondary Endpoints:
- Efficacy: Assessed via radiographic imaging (MRI) per standardized criteria (e.g., Response Assessment in Neuro-Oncology - RANO). Key metrics include Progression-Free Survival (PFS) and Overall Survival (OS) [52].
- Pharmacokinetics: Measurement of drug concentration in the blood over time.
The following diagram outlines the key stages and decision points in the clinical development of these agents.
The Scientist's Toolkit: Research Reagents and Methodologies
Advancing research on microtubule-stabilizing agents requires a specific set of reagents and tools. The table below details essential components for conducting experiments in this field.
Table 3: Essential Research Reagents and Tools
| Reagent / Tool | Function & Utility in Research | Examples / Notes |
|---|---|---|
| Stabilizing Compounds | Tool compounds for in vitro and in vivo proof-of-concept studies. | Paclitaxel (despite poor BBB penetration), Epothilone D, TPI 287 [50] [52]. |
| Tau Transgenic Mouse Models | In vivo models to study efficacy, dosing, and mechanisms of action in a pathologically relevant context. | PS19, rTg4510, 3X Tg models [50]. |
| Tubulin Polymerization Assays | In vitro biochemical assays to directly quantify a compound's ability to promote tubulin assembly into microtubules. | Measured by turbidity (increase in optical density) [50] [53]. |
| Cell-Based Phenotypic Assays | To assess compound effects on cellular microtubules and mitosis. | Evaluation of microtubule bundling in interphase cells and mitotic arrest [51] [53]. |
| Biomarkers of Target Engagement | To confirm the drug is hitting its intended target in the CNS and producing a biological effect. | Immunohistochemistry for stable microtubule density (e.g., acetylated tubulin) in animal brain tissue [50]. |
Microtubule-stabilizing agents represent a mechanistically rational and promising class of investigational therapeutics for neurodegenerative diseases characterized by cytoskeletal collapse, particularly tauopathies like Alzheimer's disease. Strong preclinical evidence demonstrates that brain-penetrant compounds such as Epothilone D and TPI 287 can counteract the downstream effects of pathological tau, including microtubule destabilization and deficits in axonal transport, leading to functional improvement in animal models [50] [52].
The critical challenge for the field is the successful clinical translation of these promising preclinical results. Initial clinical trials have established that these agents can be safely administered at low doses, avoiding the severe side effects seen in oncology [50] [52]. The ongoing and future clinical trials will be pivotal in determining whether the robust pathological and functional benefits observed in mice will translate into tangible cognitive and clinical benefits for patients. As research progresses, the integration of biomarker data to confirm target engagement and patient stratification based on tau pathology will be essential for validating this innovative therapeutic strategy and bringing it to the clinic.
Within the context of cytoskeletal defects in neurodegeneration, histone deacetylase 6 (HDAC6) has emerged as a critical enzyme interfacing between protein homeostasis, cytoskeletal integrity, and neuronal survival. Unlike other histone deacetylases that are primarily nuclear and regulate gene expression, HDAC6 is predominantly cytoplasmic and operates as a key regulator of non-histone substrates, most notably α-tubulin and components of the protein quality control machinery [54] [55]. In neurodegenerative diseases such as Alzheimer's disease (AD) and Amyotrophic Lateral Sclerosis (ALS), the pathogenic hallmarks—including accumulation of misfolded proteins, impaired axonal transport, and mitochondrial dysfunction—are intimately linked to HDAC6's catalytic functions [56] [57]. The enzyme's unique structure, featuring two catalytic domains and a ubiquitin-binding zinc finger motif, allows it to govern both microtubule stability via tubulin deacetylation and the clearance of toxic protein aggregates via the aggresome-autophagy pathway [58] [55]. Consequently, targeted inhibition of HDAC6 presents a compelling dual-pathway therapeutic strategy to counteract the cytoskeletal collapse and proteostatic failure that characterize neurodegenerative mechanisms.
Molecular Mechanisms of HDAC6 in Cytoskeletal and Proteostatic Dysfunction
Structural Determinants of HDAC6 Function and Inhibition
HDAC6 possesses a unique multi-domain architecture that underpins its diverse cellular roles. The structure includes two catalytic domains (CD1 and CD2), a dynein motor-binding domain, and a C-terminal zinc finger ubiquitin-binding domain (ZnF-UBP) [58] [55]. While both catalytic domains can deacetylate substrates, CD2 is the more catalytically active and is primarily responsible for the deacetylation of key substrates like α-tubulin [58] [59]. The ZnF-UBP domain allows HDAC6 to bind polyubiquitinated proteins, a critical function in protein aggregate clearance [56] [58]. Notably, HDAC6's active site is shallower and wider than other HDAC isoforms, a structural feature that has been strategically exploited to develop highly selective inhibitors with bulky cap groups that minimize off-target effects [59]. Key residues, such as the "gatekeeper" Ser531 and His614, facilitate specific hydrogen-bonding interactions with selective inhibitors, enabling enhanced isoform specificity [59].
Core Pathways in Neurodegeneration
The pathophysiological relevance of HDAC6 in neurodegeneration is driven by its regulation of two interconnected cellular processes: microtubule dynamics and aggresome formation.
Regulation of Tubulin Acetylation and Microtubule Stability: HDAC6 is the primary deacetylase of α-tubulin at Lys40. Deacetylation by HDAC6 reduces microtubule stability, compromising structural integrity and impairing intracellular transport [56] [55]. In neurons, this leads to defective axonal transport, disrupting the mitochondrial trafficking necessary for energy distribution and health in elongated axons. Inhibition of HDAC6 results in hyperacetylated, stabilized microtubules, which has been shown to protect against axonal degeneration in models like the mSOD1G93A mouse model of ALS [57].
Aggresome Formation and Protein Clearance: Under proteotoxic stress, HDAC6 acts as a scaffold that recognizes polyubiquitinated, misfolded proteins via its ZnF-UBP domain. It then links these protein cargos to the dynein motor complex, facilitating their transport along microtubules to the microtubule-organizing center (MTOC) to form aggresomes [58] [55]. Subsequently, aggresomes are encapsulated by autophagosomes and degraded by lysosomes in a process termed "aggrephagy." This HDAC6-dependent pathway serves as a critical compensatory mechanism when the ubiquitin-proteasome system is overwhelmed, as is common in neurodegenerative diseases with proteinopathy [56] [58].
The diagram below illustrates how HDAC6 inhibition concurrently stabilizes microtubules and clears toxic protein aggregates.
Diagram 1: HDAC6 Inhibition Promotes Neuroprotection. This figure illustrates the dual-pathway mechanism by which HDAC6 inhibition counteracts neurodegeneration. By inhibiting HDAC6, microtubules are stabilized through increased α-tubulin acetylation, improving axonal transport. Concurrently, HDAC6 inhibition enhances the clearance of toxic protein aggregates via the aggresome-autophagy pathway, addressing both cytoskeletal integrity and proteostatic dysfunction.
Quantitative Profiling of HDAC6 Inhibitors
The development of HDAC6 inhibitors has progressed from non-selective pan-inhibitors to highly selective compounds designed to minimize the adverse effects associated with broad-spectrum HDAC inhibition [59]. The quantitative profiling of these inhibitors, particularly their potency and selectivity, is fundamental for evaluating their therapeutic potential.
Table 1: Potency and Selectivity of Representative HDAC6 Inhibitors
| Inhibitor Name | HDAC6 IC₅₀ (nM) | Selectivity Index (vs. HDAC1) | Key Structural Features | Development Status |
|---|---|---|---|---|
| Cmpd. 5b [59] | 17.15 | 19-fold | Quinazolin-4-one cap; targets Ser531 and L1/L2 loops | Preclinical |
| Cmpd. 18 [60] | 5.41 | 117-fold | 2-(2-phenoxyethyl)pyridazin-3(2H)-one scaffold | Preclinical |
| Tubastatin A [60] | 15.11 | Not Specified | Hydroxamate-based; well-characterized tool compound | Preclinical / Research Use |
| Ricolinostat (ACY-1215) [61] | N/A | N/A | First-in-class selective inhibitor | Phase II (Diabetic Neuropathy) |
| KA2507 [61] | N/A | N/A | Potent and selective | Phase I (Solid Tumors) |
Table 2: Efficacy Data of HDAC6 Inhibitors in Preclinical Neurodegeneration Models
| Inhibitor Name | Disease Model | Key Efficacy Outcomes | Proposed Primary Mechanism |
|---|---|---|---|
| ACY-738 [57] | mSOD1G93A (ALS) mice | ↑ α-tubulin acetylation in spinal cord; ↓ motor neuron degeneration; ↑ peripheral nerve axon puncta size | Microtubule Stabilization |
| Panobinostat [56] | Alzheimer's models | ↑ Aβ clearance via upregulation of neprilysin | Protein Clearance Enhancement |
| Compound 5b [59] | Drug-resistant MCF-7/ADR cancer cells | Anti-proliferative activity (GI₅₀ = 2.4 μM); induced apoptosis | Multi-target (Oncology Model) |
| AVS100 [58] | Atherosclerosis model | ↓ Macrophage foam cell formation; ↓ plaque progression | Immunomodulation / Anti-inflammatory |
Experimental Framework for Evaluating HDAC6 Inhibitors
Protocol for In Vitro HDAC6 Inhibition and Selectivity Profiling
Objective: To determine the half-maximal inhibitory concentration (IC₅₀) of a candidate compound against HDAC6 and assess its selectivity over other HDAC isoforms (e.g., HDAC1).
Materials:
- Recombinant HDAC Enzymes: Human recombinant HDAC6, HDAC1, HDAC2, HDAC3, and HDAC8.
- Fluorogenic Substrate: Acetylated peptide substrate (e.g., (Ac)K-p-nitroanilide) for HDAC6.
- Developer Solution: Contains trypsin to terminate the deacetylation reaction and release the fluorescent product.
- Reference Inhibitors: Tubastatin A (selective HDAC6i) and Trichostatin A (pan-HDACi) as controls.
- Equipment: Fluorescence microplate reader.
Method:
- Enzyme Reaction: In a 96-well plate, serially dilute the test compound in assay buffer. Add recombinant HDAC enzyme and incubate for 10 minutes. Initiate the reaction by adding the fluorogenic substrate. Incubate the reaction mixture for 60-90 minutes at 37°C [59].
- Reaction Termination and Detection: Add the developer solution containing trypsin to each well and incubate for an additional 20 minutes. The fluorescence intensity (excitation ~360 nm, emission ~460 nm) is measured, which is proportional to the deacetylase activity.
- Data Analysis: Calculate the percentage of inhibition relative to a DMSO control (0% inhibition) and a no-enzyme blank (100% inhibition). Plot the dose-response curve and compute the IC₅₀ value using non-linear regression (e.g., log(inhibitor) vs. response -- Variable slope four-parameter fit). The selectivity index is calculated as (IC₅₀ for HDAC1) / (IC₅₀ for HDAC6) [59] [60].
Protocol for Assessing Tubulin Acetylation and Aggresome Clearance in Cellular Models
Objective: To validate the on-target activity of an HDAC6 inhibitor in cells and evaluate its functional impact on microtubule stability and protein aggregate clearance.
Materials:
- Cell Line: Neuroblastoma cell lines (e.g., SH-SY5Y) or primary neuronal cultures.
- Treatment: Candidate HDAC6 inhibitor (e.g., Tubastatin A, ACY-738), DMSO vehicle control, and proteasome inhibitor (e.g., MG-132) to induce aggresome formation.
- Antibodies: Anti-acetylated-α-tubulin (clone 6-11B-1), anti-α-tubulin (loading control), anti-HDAC6, and an antibody against a misfolded protein (e.g., anti-pTau for Alzheimer's models).
- Dyes: DAPI for nuclear counterstaining.
- Equipment: Western blot apparatus, confocal microscope.
Method:
- Cell Treatment and Lysate Preparation: Plate cells in appropriate culture dishes. The following day, pre-treat cells with the HDAC6 inhibitor or vehicle for 2 hours, then co-treat with MG-132 (10 µM) for an additional 4-6 hours to induce aggregation. Harvest cells and lyse in RIPA buffer supplemented with protease and deacetylase inhibitors [56] [57].
- Western Blot Analysis: Resolve equal amounts of protein lysates by SDS-PAGE and transfer to a PVDF membrane. Probe the membrane with anti-acetylated-α-tubulin and anti-α-tubulin antibodies. Use chemiluminescence for detection. Densitometric analysis of the acetylated-α-tubulin band, normalized to total α-tubulin, quantifies microtubule stabilization [57].
- Immunofluorescence and Aggresome Visualization: Seed cells on glass coverslips. After treatment, fix cells with 4% paraformaldehyde, permeabilize with 0.1% Triton X-100, and block with BSA. Incubate with anti-acetylated-α-tubulin and anti-ubiquitin (or anti-pTau) antibodies overnight at 4°C, followed by incubation with fluorescently-labeled secondary antibodies (e.g., Alexa Fluor 488, 555) and DAPI. Image cells using a confocal microscope. A successful HDAC6 inhibitor will increase diffuse acetylated-tubulin signal and reduce the number and size of perinuclear ubiquitin-positive aggregates [58] [55].
The following workflow summarizes the key steps in the discovery and validation of novel HDAC6 inhibitors.
Diagram 2: HDAC6 Inhibitor Discovery Workflow. This diagram outlines a multi-stage pipeline for developing and validating selective HDAC6 inhibitors, from initial design and synthesis to in vitro, cellular, and in vivo testing.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for HDAC6 and Neurodegeneration Research
| Reagent / Tool | Function / Application | Example Product / Identifier |
|---|---|---|
| Selective HDAC6 Inhibitors | Pharmacological tools to probe HDAC6 function and validate target engagement. | Tubastatin A, Ricolinostat (ACY-1215), ACY-738 |
| Anti-acetylated-α-tubulin Antibody | Readout for HDAC6 inhibition; measures microtubule stabilization via Western Blot (WB) and Immunofluorescence (IF). | Clone 6-11B-1 |
| Pan-HDAC Inhibitor (Control) | Positive control for inducing global protein hyperacetylation. | Trichostatin A (TSA) |
| Proteasome Inhibitor | Induces proteotoxic stress and aggresome formation for functional clearance assays. | MG-132 |
| Anti-Ubiquitin Antibody | Labels protein aggregates for quantification in aggresome clearance assays (IF). | P4D1 |
| HDAC6 Selectivity Panel | In vitro enzymatic assays to determine inhibitor IC₅₀ and selectivity profile. | Recombinant HDAC1, HDAC2, HDAC3, HDAC6, HDAC8 |
| Cell Line for Neurodegeneration Models | Human-derived neuronal cells for mechanistic studies. | SH-SY5Y neuroblastoma cells |
HDAC6 represents a mechanistically unique and therapeutically promising node at the intersection of cytoskeletal integrity and protein homeostasis in neurodegenerative diseases. The compelling preclinical data demonstrating that HDAC6 inhibition can simultaneously stabilize microtubules and enhance the clearance of toxic protein aggregates provides a strong rationale for its continued investigation [56] [57]. The field is advancing rapidly, moving beyond simple hydroxamate-based inhibitors to sophisticated molecules designed with artificial intelligence and rational structure-based design to achieve exquisite selectivity and improved pharmacokinetic properties [59] [60]. Future research should focus on optimizing the blood-brain barrier penetration of these compounds and validating their efficacy in complex, human-relevant disease models. As several selective HDAC6 inhibitors progress through clinical trials for oncology and peripheral neuropathies, their potential for repurposing in central neurodegenerative disorders presents a promising and timely frontier for drug development [61] [62].
The cytoskeleton, a dynamic network of filamentous proteins, is fundamental to neuronal health, governing processes critical to neurodegeneration such as synaptic plasticity, axonal transport, and structural integrity. Dysregulation of cytoskeletal signaling pathways is a central mechanism in the pathogenesis of numerous neurodegenerative diseases, including Alzheimer's disease (AD) and Parkinson's disease (PD) [63] [6]. Within this context, two key signaling molecules—Rho-associated coiled-coil containing protein kinase (ROCK) and Glycogen Synthase Kinase 3 Beta (GSK3β)—have emerged as critical regulators of cytoskeletal dynamics and promising therapeutic targets.
The RhoA/ROCK/GSK3β signaling axis represents a particularly crucial pathway, integrating multiple upstream signals to control downstream cytoskeletal effectors [63] [64]. ROCK, a serine/threonine kinase, acts as a primary downstream effector of the small GTPase RhoA, directly regulating actin cytoskeleton organization, cell adhesion, and motility [65]. GSK3β, another serine/threonine kinase, is a multifunctional enzyme with over 100 substrates, placing it at the intersection of numerous signaling cascades with profound effects on neuronal survival, tau phosphorylation, and microtubule stability [63] [66]. This technical review examines the mechanistic interplay between these kinases, their role in cytoskeletal pathology, and the experimental approaches for targeting them therapeutically.
Mechanistic Insights: The ROCK/GSK3β Signaling Axis
Molecular Architecture and Regulation
ROCK Isoforms and Activation Mechanisms: ROCK exists as two isoforms, ROCK-I and ROCK-II, which share 65% overall homology and 92% homology in their kinase domains [63]. While ROCK-I is expressed broadly in non-neuronal tissues including liver, testis, and kidney, ROCK-II is predominantly expressed in the brain and skeletal muscle, suggesting specialized neuronal functions [63]. Structurally, ROCK contains an N-terminal kinase domain, a central coiled-coil domain, and a C-terminal Pleckstrin Homology (PH) domain with an embedded cysteine-rich domain. The PH domain maintains ROCK in an auto-inhibited state under basal conditions by interacting with the N-terminal kinase domain [63].
ROCK activation occurs primarily through binding of GTP-bound RhoA to the Rho-binding domain, which relieves this auto-inhibition [65]. Alternative activation mechanisms include arachidonic acid binding to the PH domain or caspase-mediated cleavage of the C-terminal region, particularly during apoptosis [63]. Post-translational modifications, especially phosphorylation, further fine-tune ROCK activity and subcellular localization.
GSK3β Structure and Complex Regulation: GSK3β is constitutively active under basal conditions and is primarily regulated through inhibitory phosphorylation. The kinase is structurally organized with a conserved kinase domain and unique N- and C-terminal regions that mediate protein-protein interactions and subcellular targeting [63]. Phosphorylation of Ser9 in the N-terminal domain by upstream kinases such as AKT creates a pseudosubstrate that occupies the substrate-binding pocket, effectively inhibiting kinase activity [63]. The RhoA/ROCK pathway indirectly activates GSK3β by deactivating these GSK3β-inhibitory kinases, creating a direct signaling link between these two pathways [63].
Pathway Crosstalk and Downstream Effectors
The RhoA/ROCK/GSK3β signaling cascade represents a critical point of convergence in cytoskeletal regulation. Activated RhoA-GTP binds to and activates ROCK, which then phosphorylates multiple downstream substrates that directly control actin dynamics, including:
- LIM Kinase (LIMK): Phosphorylates and inactivates cofilin, an actin-depolymerizing factor, thereby stabilizing F-actin networks [63]
- Myosin Light Chain (MLC): Direct phosphorylation increases actomyosin contractility, while simultaneous phosphorylation of myosin phosphatase target subunit 1 (MYPT1) inhibits the myosin phosphatase complex, further enhancing MLC phosphorylation [65]
- Collapsing Response Mediator Protein-2 (CRMP-2): Phosphorylation inhibits microtubule assembly and contributes to growth cone collapse [63]
Table 1: Key Downstream Effectors of ROCK and GSK3β Signaling
| Effector | Phosphorylation Site | Functional Consequence | Cytoskeletal Impact |
|---|---|---|---|
| LIMK | Threonine 508 | Activation | Stabilizes F-actin; inhibits cofilin-mediated depolymerization |
| Cofilin | Serine 3 | Inactivation by LIMK | Reduces actin severing and depolymerization |
| MYPT1 | Threonine 696 | Inhibition of myosin phosphatase | Increases MLC phosphorylation; enhances contractility |
| CRMP-2 | Threonine 555 | Inactivation | Inhibits microtubule assembly; promotes growth cone collapse |
| Tau | Multiple Ser/Thr residues | Hyperphosphorylation | Reduces microtubule binding; promotes aggregation |
| β-catenin | Serine 33/37/Thr41 | Degradation | Downregulates Wnt signaling; affects cell adhesion |
ROCK further influences cytoskeletal dynamics through its indirect regulation of GSK3β. ROCK activation leads to inhibition of AKT, a key kinase responsible for inhibitory phosphorylation of GSK3β at Ser9. The consequent GSK3β activation drives tau hyperphosphorylation, impaired axonal transport, and transcriptional changes through substrates like β-catenin [63]. This pathway crosstalk creates an amplification loop wherein RhoA/ROCK signaling exacerbates GSK3β-mediated pathological processes.
Diagram 1: The ROCK/GSK3β Signaling Pathway in Neuronal Cytoskeletal Regulation. This diagram illustrates the molecular relationships and regulatory mechanisms within the ROCK/GSK3β signaling axis, highlighting key upstream regulators, downstream effectors, and functional outcomes relevant to neuronal health and disease.
Cytoskeletal Defects in Neurodegeneration
Alzheimer's Disease: Tau Pathology and Microtubule Instability
In Alzheimer's disease, the RhoA/ROCK/GSK3β pathway contributes significantly to the hallmark pathologies of amyloid-beta accumulation and tau hyperphosphorylation [63]. GSK3β hyperactivity drives the hyperphosphorylation of tau at multiple epitopes, reducing its affinity for microtubules and promoting aggregation into neurofibrillary tangles (NFTs) [63] [66]. This pathological tau phosphorylation occurs at specific sites including Thr231 and Ser262, which are particularly critical for microtubule binding affinity [66].
Microtubule destabilization represents one of the earliest pathological events in AD, preceding the formation of overt amyloid plaques and NFTs [6]. The loss of stable microtubules disrupts essential intracellular transport processes, leading to synaptic dysfunction and ultimately neuronal death. Recent advances in neuroimaging have enabled the visualization of microtubule instability in vivo using novel positron emission tomography (PET) radiotracers such as [¹¹C]MPC-6827, which selectively binds to destabilized microtubules and shows promising potential as an early diagnostic biomarker [6].
Parkinson's Disease and Synucleinopathies: Actin Dysregulation
In Parkinson's disease and related synucleinopathies like Multiple System Atrophy (MSA), cytoskeletal dysfunction manifests primarily through alpha-synuclein-mediated disruption of actin dynamics [67]. In MSA, oligodendroglial accumulation of alpha-synuclein impairs process outgrowth and myelin maintenance through direct interference with actin remodeling machinery [67]. This pathological mechanism was confirmed in post-mortem putaminal tissue from MSA patients, which showed significant actin imbalances compared to controls.
Notably, treatment with the ROCK inhibitor Y-27632 rescued oligodendroglial process formation and improved ensheathment capacity in human oligodendrocytes expressing alpha-synuclein, demonstrating the therapeutic potential of targeting this pathway [67]. This finding highlights how cytoskeletal defects in synucleinopathies extend beyond neurons to include glial pathology, with profound implications for neuronal function and survival.
Computational Evidence for Cytoskeletal Involvement
Recent computational approaches have further solidified the connection between cytoskeletal genes and age-related neurodegenerative diseases. A machine learning-based framework analyzing transcriptional changes in cytoskeletal genes identified 17 key genes associated with age-related diseases including Alzheimer's disease [9]. The study employed Support Vector Machines (SVM) classifiers, which achieved the highest accuracy in identifying disease-associated cytoskeletal genes, including ENC1, NEFM, ITPKB, PCP4, and CALB1 as specifically associated with AD [9].
Table 2: Quantitative Effects of Cytoskeletal-Targeted Interventions in Experimental Models
| Intervention | Experimental Model | Key Outcome Measures | Results | Source |
|---|---|---|---|---|
| ROCK Inhibitor (Y-27632) | Human oligodendrocytes with α-synuclein expression | Process outgrowth; Axon ensheathment | Rescued process formation; Improved ensheathment capacity | [67] |
| GSK-3β Inhibitor (AR-A014418) | MDA-MB-231 cancer cells (invasion assay) | Matrix invasion; Cell migration; Focal adhesion | Invasion reduced to 38.5±4.7%; Migration reduced to 45.5±5.5% of control | [68] |
| GSK-3β Inhibitor (AR-A014418) | RKO cancer cells (invasion assay) | Matrix invasion | Invasion reduced to 29.3±6.8% of control | [68] |
| ROCK/GSK3β pathway modulation | Alzheimer's disease models | Tau phosphorylation; Neurite outgrowth | Reduced tau hyperphosphorylation; Improved neurite outgrowth | [63] |
Experimental Approaches and Research Tools
Investigating ROCK/GSK3β Signaling: Methodological Framework
In Vitro Cytoskeletal Reorganization Assays: The study of ROCK and GSK3β inhibitors typically employs well-established cytoskeletal reorganization assays. For investigating cancer cell invasion (as a model for cytoskeletal dynamics), the Boyden chamber assay coated with extracellular matrix components is widely used [68]. In these experiments, cells are pre-treated with inhibitors for 24 hours before seeding in the chamber. Specific protocols utilize 20 μM AR-A014418 (a GSK-3β-specific inhibitor) or DMSO vehicle control, with invasion measured after 24-48 hours of incubation [68]. For morphological analysis of process outgrowth, differentiating human oligodendrocytes are treated with 2 μM Y-27632 (ROCK inhibitor) for 24 hours, followed by immunocytochemistry for cytoskeletal markers [67].
Molecular Analysis of Pathway Activity: Western blot analysis remains essential for evaluating phosphorylation status of pathway components. Key targets include:
- Phospho-MLC2 (Thr18/Ser19) for ROCK activity
- Phospho-cofilin (Ser3) for LIMK activity
- Phospho-GSK3β (Ser9) for inhibitory regulation
- Phospho-tau epitopes (Thr231, Ser396, etc.) for downstream pathological effects [63] [67]
Additional approaches include RhoA activation assays using Rhotekin-RBD pull-downs, microtubule stability assays measuring acetylated tubulin levels, and actin polymerization assays using phalloidin staining [65] [67].
Advanced Imaging Techniques: Recent advances in live-cell imaging and super-resolution microscopy enable direct visualization of cytoskeletal dynamics. For microtubule-specific imaging, plus-end tracking proteins such as EB3 fused to fluorescent tags allow quantification of microtubule dynamics in real-time [6]. For clinical translation, microtubule-targeted PET imaging with [¹¹C]MPC-6827 provides a non-invasive method for assessing microtubule stability in vivo, with demonstrated applications in neurodegenerative disease models [6].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating ROCK/GSK3β Signaling
| Reagent/Category | Specific Examples | Research Application | Mechanistic Function |
|---|---|---|---|
| ROCK Inhibitors | Y-27632, Fasudil (HA-1077) | Rescue of process outgrowth; Reduction of actomyosin contractility | ATP-competitive inhibition of ROCK kinase activity |
| GSK3β Inhibitors | AR-A014418, GSK-3β inhibitor XXVI, CHIR99021 | Reduction of tau phosphorylation; Inhibition of cancer cell invasion | ATP-competitive or allosteric inhibition of GSK3β |
| Cytoskeletal Stains | Phalloidin (F-actin), Anti-acetylated tubulin (microtubules) | Morphological analysis; Quantification of cytoskeletal organization | Direct binding to cytoskeletal polymers for visualization |
| Activation State Markers | Phospho-specific antibodies: p-MLC2, p-cofilin, p-GSK3β (Ser9) | Western blot; Immunofluorescence to assess pathway activity | Detection of phosphorylation events indicating pathway activation |
| Live-Cell Imaging Probes | EB3-GFP (microtubule plus-ends), LifeAct (F-actin) | Real-time visualization of cytoskeletal dynamics | Fluorescent tagging of dynamic cytoskeletal components |
Diagram 2: Experimental Workflow for Investigating ROCK/GSK3β Inhibition. This diagram outlines a comprehensive methodological approach for studying the effects of ROCK and GSK3β inhibitors on cytoskeletal signaling, incorporating model systems, functional assays, molecular analyses, and data integration strategies.
Therapeutic Translation and Challenges
Inhibitor Development and Clinical Prospects
The development of ROCK and GSK3β inhibitors has progressed significantly, though clinical translation for neurodegenerative applications faces substantial challenges. ROCK inhibitors including Fasudil (HA-1077) have advanced to clinical use for non-neurological indications, particularly cardiovascular applications, demonstrating generally favorable safety profiles [63]. In preclinical neurodegeneration models, ROCK inhibitors have shown promise in ameliorating cytoskeletal defects, improving axonal regeneration, and rescuing process outgrowth in oligodendrocytes expressing alpha-synuclein [67].
GSK3β inhibitor development has proven more challenging due to this kinase's involvement in numerous essential cellular processes, creating potential for off-target effects and toxicity [63]. The complexity of achieving specific neuronal inhibition without disrupting peripheral metabolism has limited clinical advancement, though next-generation inhibitors with improved CNS penetration and selectivity are under active investigation [63] [66].
Biomarker Development and Target Engagement
A critical hurdle in therapeutic development has been the quantification of target engagement and biological effect in the central nervous system. Recent advances in microtubule-targeted PET imaging with radiotracers such as [¹¹C]MPC-6827 offer promising approaches for directly assessing cytoskeletal stabilization as a pharmacodynamic marker in clinical trials [6]. These imaging tools enable non-invasive evaluation of microtubule integrity, potentially providing early readouts of therapeutic efficacy before structural neurodegeneration becomes irreversible.
Complementary biomarker approaches include measuring phospho-tau species in cerebrospinal fluid as indicators of GSK3β pathway modulation, and assessing inflammatory markers associated with ROCK pathway activity [63] [66]. The integration of these biomarker strategies with clinical outcomes will be essential for advancing cytoskeletal-targeted therapies through the drug development pipeline.
The RhoA/ROCK/GSK3β signaling axis represents a crucial point of convergence in cytoskeletal regulation with broad implications for neurodegenerative disease pathogenesis and treatment. The intricate crosstalk between these kinases creates both challenges and opportunities for therapeutic intervention, as combined approaches may yield synergistic benefits while mitigating individual limitations. Future research directions should prioritize the development of brain-penetrant inhibitors with improved selectivity, the validation of cytoskeletal biomarkers for clinical trial implementation, and the exploration of pathway modulation in early disease stages when cytoskeletal pathology may be most reversible.
The emerging recognition of microtubule instability as an early event in neurodegeneration, coupled with advanced imaging techniques for visualizing cytoskeletal dynamics in vivo, promises to transform our approach to diagnosing and treating these devastating disorders. As our understanding of cytoskeletal signaling networks continues to evolve, so too will opportunities for therapeutic intervention targeting the fundamental structural framework of the neuron.
Advanced Imaging and Biochemical Techniques for Cytoskeletal Analysis
The cytoskeleton, a dynamic network of protein filaments, is fundamental to cellular integrity, intracellular transport, and synaptic function. Within the context of neurodegenerative disease research, cytoskeletal defects are increasingly recognized as a critical pathological mechanism, rather than a mere consequence of cell death [21] [69]. The analysis of cytoskeletal organization and dynamics therefore provides a vital window into disease mechanisms. Traditional qualitative assessments have proven insufficient for capturing the subtle dysregulations characteristic of early neurodegeneration. This guide details advanced, quantitative methodologies that combine high-resolution imaging with sophisticated computational analysis and biochemical assays, enabling researchers to precisely decipher the role of cytoskeletal pathology in diseases such as Alzheimer's, Parkinson's, and Amyotrophic Lateral Sclerosis (ALS).
Advanced Imaging and Computational Analysis
Modern cytoskeleton research leverages live-cell imaging to capture dynamic processes, generating vast, high-dimensional datasets. The extraction of meaningful, quantitative information from these datasets necessitates robust computational approaches.
Deep Learning-Powered Image Segmentation
Conventional digital microscopy methods often struggle with accurate quantification of parameters like cytoskeleton density. A groundbreaking deep learning-based segmentation technique developed by Kumamoto University has significantly improved the precision of these measurements [70]. This AI-driven model, trained on hundreds of confocal microscopy images, excels at distinguishing cytoskeletal structures with high accuracy, enabling more reliable study of processes such as stomatal movement and zygote development in plant models, with direct applicability to neuronal systems [70].
Experimental Protocol: Deep Learning-Based Cytoskeleton Segmentation
- Sample Preparation: Culture and maintain cells (e.g., neuronal cell lines, primary neurons) on imaging-appropriate dishes. For fixed cells, stain F-actin with phalloidin conjugates; for live-cell imaging, transfert with fluorescently tagged actin-binding peptides (e.g., Lifeact) or G-actin (e.g., GFP-actin) [71].
- Image Acquisition: Acquire high-resolution z-stacks of the cells using a confocal microscope. Ensure consistent imaging parameters (laser power, gain, resolution) across all samples.
- Dataset Curation: Compile a dataset of hundreds of images. Manually annotate cytoskeletal structures in a subset of images to create a ground-truth training set.
- Model Training: Train a convolutional neural network (CNN), such as a U-Net architecture, using the annotated images. The model learns to map raw image pixels to segmentation masks of cytoskeletal filaments.
- Validation & Analysis: Validate the model's performance on a separate set of images not used in training. Apply the trained model to new images for automated, high-throughput segmentation and quantification of parameters like density, orientation, and filament length [70].
Quantification of Specific Actin Architectures
Different actin structures serve distinct functional roles, and their precise quantification is crucial. Table 1 summarizes specialized computational tools for analyzing specific actin architectures, along with the key metrics they provide.
Table 1: Computational Tools for Quantifying Actin Cytoskeleton Organization
| Tool Name | Actin Structure Analyzed | Key Quantitative Metrics | Application Example |
|---|---|---|---|
| Stress Fiber Extractor (SFEX) [71] | Stress fibers (ventral, dorsal, transverse arcs) | Fiber width, length, orientation, shape | Correlating stress fiber width with cellular contractility in mechanosensing studies. |
| FSegment [71] | Stress fibers (time-lapse analysis) | Length, width, orientation, intensity distribution over time | Measuring stress fiber thinning during cell relaxation. |
| SFALab [71] | Ventral stress fibers & focal adhesions | Number of ventral stress fibers, stress fibers per focal adhesion, focal adhesion density & aspect ratio | Linking focal adhesion density to cellular tension transmission. |
| FibrilTool [72] | Fibrillar structures (e.g., microtubule arrays) | Anisotropy and orientation of fibrillar structures | Analyzing cortical microtubule reorganization after plant cytokinesis. |
The following workflow diagram outlines the general process for the computational quantification of cytoskeletal images, from image acquisition to quantitative analysis.
Biochemical and Molecular Profiling Techniques
Beyond structural analysis, understanding the molecular underpinnings of cytoskeletal dysregulation in neurodegeneration requires techniques for profiling gene expression and protein interactions.
Identifying Cytoskeletal Gene Signatures in Disease
Transcriptional dysregulation of cytoskeletal genes is a hallmark of age-related diseases. An integrative computational framework combining machine learning with differential expression analysis can identify potential cytoskeletal biomarkers [9].
Experimental Protocol: Identifying Cytoskeletal Gene Biomarkers
- Gene Set Compilation: Retrieve a comprehensive list of cytoskeletal genes from the Gene Ontology browser (GO:0005856) [9].
- Data Retrieval & Preprocessing: Obtain transcriptome data (RNA-Seq or microarray) from relevant disease datasets (e.g., from GEO or TCGA) and matched normal controls. Perform batch effect correction and normalization using packages like Limma [9].
- Machine Learning Classification: Employ multiple algorithms (e.g., Support Vector Machines (SVM), Random Forest) to build classification models that distinguish disease from control samples based on cytoskeletal gene expression. SVM has been shown to achieve high accuracy in this context [9].
- Feature Selection: Use Recursive Feature Elimination (RFE) with the SVM classifier to identify the minimal set of most discriminative cytoskeletal genes [9].
- Differential Expression Analysis: Independently, perform differential expression analysis (e.g., using DESeq2 or Limma) to identify cytoskeletal genes with significantly altered expression in disease.
- Validation: Identify overlapping genes from the RFE-selected features and differential expression analysis. Validate the predictive power of these candidate genes using Receiver Operating Characteristic (ROC) analysis on external datasets [9].
This approach has successfully identified genes like ENC1, NEFM, and ITPKB for Alzheimer's disease, and ARPC3, CDC42EP4, and LRRC49 for Hypertrophic Cardiomyopathy, demonstrating its power in pinpointing cytoskeletal targets for therapeutic intervention [9].
Analyzing Pathological Protein Aggregates
In neurodegenerative diseases, the cytoskeleton is often compromised by the formation of pathological aggregates. A prime example is the cofilin-actin rod, which is increasingly linked to Alzheimer's disease and other conditions [69]. These rods, comprised of a 1:1 ratio of dephosphorylated cofilin and ADP-actin, form in response to stressors like ATP depletion, oxidative stress, and glutamate excitotoxicity [69]. They are thought to disrupt synaptic transport and may mature into larger inclusions like Hirano bodies [69]. Notably, standard F-actin probes like phalloidin and Lifeact are ineffective for staining cofilin-actin rods, creating a significant technical challenge that requires alternative staining strategies or the development of new probes [69].
The formation of cofilin-actin rods is a tightly regulated process initiated by specific cellular stressors and signaling pathways, as illustrated below.
Integrated Workflows and the Research Toolkit
Translating basic research on cytoskeletal defects into mechanistic insights for drug development requires integrated workflows that combine multiple techniques. The following diagram outlines a comprehensive pipeline from initial discovery to functional validation, specifically framed within neurodegeneration research.
The Scientist's Toolkit: Essential Reagents and Materials
Successful execution of these advanced protocols relies on a suite of specific reagents and tools. The following table details key resources for cytoskeletal analysis in neurodegeneration research.
Table 2: Research Reagent Solutions for Cytoskeletal Analysis
| Reagent/Material | Function/Application | Key Considerations |
|---|---|---|
| Phalloidin Conjugates [71] | High-affinity F-actin stain for fixed cells. Labels most actin structures. | Gold standard for fixed cells; does not stain cofilin-actin rods [69]. |
| Live-actin Probes (e.g., GFP-Lifeact, GFP-Utrophin) [71] | Live-cell imaging of F-actin dynamics. | Does not bind to cofilin-actin rods, limiting use for this pathology [69]. |
| Fluorescently Tagged G-actin (e.g., GFP-actin) [71] | Labels both monomeric and filamentous actin pools in live cells. | Can incorporate into dynamic structures but may perturb native actin dynamics. |
| StayGold Variants [72] | Extremely stable fluorescent proteins for long-term live imaging. | Useful for fusions to monitor cytoskeletal proteins over extended durations. |
| Cofilin Mutants & Antibodies (e.g., phospho-Ser3 specific) [69] | To monitor cofilin activation status (dephosphorylation = active) and rod formation. | Essential for studying rod pathology in neurodegeneration. |
| Machine Learning Platforms (e.g., Python with Scikit-learn, TensorFlow) [9] | For building custom classifiers and feature selection models based on cytoskeletal gene expression or image features. | Enables identification of novel disease-associated signatures. |
The field of cytoskeletal analysis has been transformed by the convergence of advanced imaging, biochemical profiling, and computational power. Moving beyond descriptive morphology, researchers can now obtain high-dimensional, quantitative data on cytoskeletal organization, dynamics, and molecular composition. The integration of these techniques—such as applying deep learning to images of cytoskeletal structures whose molecular components have been identified via transcriptomic analysis—provides a powerful, multi-angled approach to deciphering the complex role of the cytoskeleton in neurodegenerative diseases. These methodologies are paving the way for the identification of novel biomarkers and the development of targeted therapies aimed at preserving cytoskeletal integrity to halt or slow disease progression.
Challenges in Therapeutic Development and Optimization Strategies
Blood-Brain Barrier Penetration and Selective Targeting of Pathological Cytoskeleton
The blood-brain barrier (BBB) represents one of the most significant challenges in developing effective treatments for neurodegenerative diseases. This highly selective semi-permeable membrane prevents more than 98% of small-molecule drugs and nearly all large-molecule therapeutics from entering the central nervous system (CNS) [73] [74]. Meanwhile, cytoskeletal pathology has emerged as a fundamental component in neurodegenerative disease mechanisms, with abnormal aggregates of cytoskeletal proteins serving as neuropathological signatures across multiple conditions [22] [21]. The convergence of these two research domains—BBB penetration and cytoskeletal targeting—has created both a formidable challenge and a promising therapeutic opportunity for addressing neurodegenerative diseases.
Neurodegenerative diseases, including Alzheimer's disease (AD), Parkinson's disease (PD), amyotrophic lateral sclerosis (ALS), and frontotemporal dementia, are characterized by progressive neuronal loss and the accumulation of pathological protein aggregates [31]. Many of these diseases are classified as proteinopathies, with a significant subset specifically involving cytoskeletal proteins [22] [31]. The discovery of mutations in neuronal intermediate filament and tau genes has firmly established the importance of cytoskeletal abnormalities in disease pathogenesis [22]. These disorders, collectively termed neuronal intermediate filamentopathies and tauopathies, share common mechanisms of disease centered around progressive accumulation of abnormal filamentous proteins [22].
This technical guide provides a comprehensive analysis of current strategies for overcoming the BBB to target pathological cytoskeletal elements in neurodegenerative diseases. We examine the physiological structure of the BBB, explore the molecular mechanisms of cytoskeletal pathology, review advanced delivery platforms, detail experimental methodologies, and discuss emerging therapeutic approaches. The integration of targeted drug delivery with precision cytoskeleton modulation represents a promising frontier for developing effective treatments for these currently incurable conditions.
Blood-Brain Barrier: Structure and Function
Physiological Composition
The BBB is a multicellular, dynamic semi-permeable membrane that isolates the CNS from circulating blood [75]. Its selective barrier function depends on the collaborative efforts of several specialized cell types arranged in a complex neurovascular unit:
- Endothelial Cells: Cerebral capillary endothelial cells form the core anatomical structure of the BBB, lining cerebral blood vessels with continuous tight junctions and no fenestrations [75] [74]. These cells exhibit distinct luminal and abluminal membrane compartments, high mitochondrial content, net negative surface charge, low expression of leukocyte adhesion molecules, and specialized transporter systems [75].
- Tight Junctions: These protein complexes between endothelial cells form the primary physical barrier through proteins including claudins, occludins, and junctional adhesion molecules, which significantly restrict paracellular transport of molecules [75] [74].
- Pericytes: These mural cells embedded in the basement membrane cover approximately 100% of the CNS endothelium and play crucial roles in regulating barrier function through secretion of signaling factors, regulation of tight junction density, and coordination of neurovascular function [75].
- Astrocytes: Their end feet extensively cover the vascular surface, promoting endothelial cell differentiation and enhancing tight junction stability through release of growth factors like brain-derived neurotrophic factor [75] [74].
- Basement Membrane: This structural support composed of collagen and laminin maintains vascular wall integrity and provides a medium for intercellular signaling [74].
Transport Mechanisms
The BBB regulates molecular transit through several specialized transport mechanisms, each with distinct characteristics and applications for drug delivery:
- Passive Diffusion: Movement of lipophilic small molecules (<500 Da, LogP>2, <6 hydrogen bonds, polar surface area <60-70 Ų) along concentration gradients without energy expenditure [74].
- Carrier-Mediated Transcytosis: Utilizes highly selective transporters (e.g., GLUT1 for glucose, LAT1 for amino acids) to facilitate nutrient movement, which can be exploited for drugs structurally similar to endogenous substrates [74].
- Receptor-Mediated Transcytosis (RMT): Relies on specific receptors (e.g., transferrin receptor, insulin receptor) on the luminal side of endothelial cells to transport macromolecules via vesicular transport [75] [74].
- Adsorptive-Mediated Transcytosis (AMT): Initiated by electrostatic interactions between positive charges on molecules and negative charges on cell membranes [74].
- Efflux Pumps: ATP-binding cassette transporters (e.g., P-glycoprotein, multidrug resistance-associated proteins) actively expel drugs from endothelial cells, impeding brain entry [75] [74].
Table 1: Blood-Brain Barrier Transport Mechanisms and Characteristics
| Transport Mechanism | Key Features | Substrate Characteristics | Energy Requirement |
|---|---|---|---|
| Passive Diffusion | Follows concentration gradient | Small (<500 Da), lipophilic (LogP>2) | No |
| Carrier-Mediated Transcytosis | Uses specific transporters | Structural similarity to nutrients | Sometimes (ATP-dependent) |
| Receptor-Mediated Transcytosis | Ligand-receptor binding | Macromolecules, nanoparticles | Yes |
| Adsorptive-Mediated Transcytosis | Electrostatic interactions | Cationic molecules/particles | Yes |
| Efflux Pumps | Active expulsion | Diverse substrates (xenobiotics) | Yes (ATP-dependent) |
Cytoskeletal Pathology in Neurodegenerative Diseases
The cytoskeleton, comprising microtubules, neurofilaments, and actin filaments, is essential for neuronal structure, intracellular transport, and synaptic function. Disruption of cytoskeletal components is a hallmark of multiple neurodegenerative diseases [22] [21].
Alzheimer's Disease
AD pathology involves both extracellular amyloid-β plaques and intracellular neurofibrillary tangles (NFTs) composed of hyperphosphorylated tau protein [22] [21]. Tau stabilizes microtubules under physiological conditions, but hyperphosphorylation reduces its affinity for microtubules, leading to microtubule destabilization and tau aggregation into paired helical filaments [21]. NFTs initially appear in transentorhinal and limbic regions, progressively spreading throughout the cortex correlating with cognitive decline [22]. The relationship between amyloid pathology and tau pathology remains complex, with evidence suggesting that cytoskeletal defects may precede and facilitate amyloid accumulation through impairment of vesicular trafficking [21].
Tauopathies
Several neurodegenerative disorders are classified as tauopathies, characterized by filamentous tau deposits in the absence of neuritic plaques [22] [21]. These include:
- Frontotemporal dementia with parkinsonism linked to chromosome 17 (FTDP-17)
- Corticobasal degeneration
- Progressive supranuclear palsy
- Pick's disease
FTDP-17 mutations in the tau gene alter the ratio of three-repeat to four-repeat tau isoforms or impair tau's ability to interact with microtubules [22]. The four-repeat form binds more strongly to microtubules and tends to aggregate more rapidly, leading to neuronal dysfunction [21].
Parkinson's Disease and Synucleinopathies
While PD is primarily characterized by Lewy bodies containing α-synuclein aggregates, emerging evidence indicates significant cytoskeletal involvement [21]. α-synuclein shares physical association with molecular chaperones and may itself function as a chaperone whose mutated form promotes aggregation and hyperphosphorylation [21]. The normal function of α-synuclein in presynaptic terminals suggests roles in synaptic vesicle trafficking and neurotransmitter release that may be disrupted in disease.
Amyotrophic Lateral Sclerosis
ALS involves motor neuron degeneration with characteristic aggregates containing neurofilament and kinesin, suggesting defects in axonal transport [21]. Mutations in copper-zinc superoxide dismutase (SOD1) are linked to familial ALS, but disease mechanisms extend beyond oxidative stress to include direct disruption of tubulin through nitration near dynactin binding sites, impairing microtubule-based transport [21]. This disruption of slow axonal transport represents an early event in ALS pathophysiology.
Intermediate Filamentopathies
Mutations in neuronal intermediate filament genes are pathogenic for peripheral neuropathies and ALS [22]. Neurofilaments, the major intermediate filaments in neurons, provide structural support and regulate axon caliber. Mutations in neurofilament genes (NF-L, NF-M, NF-H) disrupt filament assembly, impair axonal transport, and lead to abnormal accumulations that compromise neuronal function [22].
Table 2: Cytoskeletal Pathology in Major Neurodegenerative Diseases
| Disease | Major Pathological Proteins | Cytoskeletal Components Affected | Genetic Mutations |
|---|---|---|---|
| Alzheimer's Disease | Hyperphosphorylated tau, Amyloid-β | Microtubules, Neurofilaments | APP, PS1, PS2, APOE (risk factor) |
| FTDP-17 | Tau | Microtubules | MAPT (tau gene) |
| Parkinson's Disease | α-synuclein | Presynaptic cytoskeleton, Microtubules | SNCA, LRRK2, Parkin |
| ALS | SOD1, TDP-43, neurofilaments | Neurofilaments, Microtubule motors | SOD1, C9orf72, TARDBP, NF genes |
| Charcot-Marie-Tooth | Peripheral myelin protein 22, Neurofilaments | Neurofilaments | PMP22, NF-L, others |
Figure 1: Molecular Pathways of Cytoskeletal Pathology in Neurodegeneration. This diagram illustrates key pathological mechanisms involving cytoskeletal proteins across neurodegenerative diseases, highlighting common pathways and disease-specific processes.
Strategies for BBB Penetration and Cytoskeletal Targeting
Molecular Delivery Approaches
Receptor-Mediated Transcytosis (RMT) utilizes specific receptors highly expressed on BBB endothelial cells to shuttle therapeutics into the brain [75] [76]. Key receptors exploited for this purpose include:
- Transferrin Receptor (TfR): Transferrin-modified liposomes and nanoparticles have successfully delivered various therapeutics including temozolomide, adriamycin, osthole, and nucleic acids across the BBB [76].
- Lactoferrin Receptor (LfR): Lactoferrin-conjugated systems show particular promise, with demonstrated efficacy in delivering resveratrol, riluzole, paeoniflorin, and chemotherapeutic agents to the CNS [76].
- Low-Density Lipoprotein Receptor (LDLR): Apolipoprotein E-modified nanocarriers exploit this pathway for brain targeting [76].
- Insulin Receptor (IR): Monoclonal antibodies against the insulin receptor have been used to ferry therapeutics across the BBB [76].
Ligand conjugation strategies involve attaching BBB-crossing motifs to therapeutic entities. Cell-penetrating peptides (e.g., TAT, penetratin), transferrin, lactoferrin, and rabies virus glycoprotein peptides have all shown efficacy in enhancing brain delivery [76]. Dual-modified systems combining multiple targeting ligands (e.g., lactoferrin and muscone) demonstrate synergistic effects [76].
Nanotechnology-Based Delivery Systems
Nanocarriers provide versatile platforms for overcoming BBB limitations through multiple mechanisms:
- Liposomes: Spherical vesicles with hydrophilic cores and lipid bilayers can be surface-modified with targeting ligands for RMT. Transferrin-modified liposomes have successfully delivered cisplatin, adriamycin, and nucleic acids to the brain [74] [76].
- Polymeric Nanoparticles: Biodegradable polymers like PLGA (poly(lactic-co-glycolic acid)) offer controlled release profiles and surface functionalization capabilities. Lactoferrin-conjugated PLGA nanoparticles have effectively delivered resveratrol for Parkinson's disease treatment [76].
- Solid Lipid Nanoparticles (SLNs): Offer improved stability compared to liposomes while maintaining high biocompatibility. Insulin receptor antibody-modified SLNs have been used to deliver saquinavir to the brain [76].
- Inorganic Nanoparticles: Gold, silica, and other inorganic nanoparticles provide unique optical, magnetic, or structural properties for therapeutic and diagnostic applications. Lactoferrin-modified hollow mesoporous copper sulfide nanoparticles have been utilized for glioblastoma treatment [76].
Physical Methods for BBB Disruption
Physical techniques temporarily disrupt BBB integrity to facilitate drug entry:
- Focused Ultrasound (FUS): When combined with microbubbles, FUS can transiently open tight junctions through acoustic cavitation effects, allowing therapeutic agents to enter the brain [73] [76]. This approach offers spatiotemporal control and has been used to enhance delivery of antibodies, chemotherapy agents, and neurotrophic factors.
- Magnetic Field-Guided Delivery: Magnetic nanoparticles can be directed to specific brain regions using external magnetic fields, enhancing localized drug accumulation [76].
Biological and Cellular Approaches
- Cell-Mediated Delivery: Stem cells and immune cells possess innate BBB-penetrating capabilities and can be loaded with therapeutic cargo. Mesenchymal stem cells have been engineered to deliver neurotrophic factors or enzyme replacements to the CNS [73].
- Exosome-Based Delivery: Natural exosomes or engineered exosome-mimetics leverage endogenous vesicular transport systems for brain delivery. CpG oligonucleotides anchored to endogenous serum exosomes have been used to deliver tanshinone IIA and glycyrrhizic acid for glioblastoma treatment [76].
- Viral Vectors: Adeno-associated viruses (AAVs) and other viral vectors can be engineered for CNS-targeted gene delivery. Dual-AAV CRISPR approaches are being developed for Huntington's disease treatment [73].
Table 3: Advanced Delivery Systems for BBB Penetration and Cytoskeletal Targeting
| Delivery System | Mechanism of BBB Penetration | Therapeutic Applications | Advantages | Limitations |
|---|---|---|---|---|
| Ligand-Decorated Nanoparticles | Receptor-mediated transcytosis | Wide range (small molecules, proteins, nucleic acids) | High specificity, versatility | Complex manufacturing, potential immunogenicity |
| Liposomes | Membrane fusion, endocytosis | Chemotherapy, enzyme replacement | High loading capacity, biocompatibility | Stability issues, rapid clearance |
| Polymeric Nanoparticles | Passive diffusion, RMT | Sustained drug release, gene therapy | Controlled release, protection of cargo | Polymer degradation products, potential toxicity |
| Exosomes | Natural trafficking mechanisms | RNA delivery, protein replacement | Native targeting, low immunogenicity | Production scalability, loading efficiency |
| Focused Ultrasound | Temporary BBB disruption | Antibodies, chemotherapy | Non-invasive, spatially controlled | Requires specialized equipment, safety concerns |
| Cell-Based Therapies | Cellular migration | Neurotrophic factors, enzyme delivery | Active targeting, multifunctionality | Cell survival, tumorigenesis risk |
Experimental Protocols and Methodologies
In Vitro BBB Models
Protocol 1: Construction of a Triple-Culture BBB Model
- Culture Brain Microvascular Endothelial Cells: Isolate primary human brain microvascular endothelial cells (HBMECs) or use established cell lines (e.g., hCMEC/D3). Culture on collagen-coated Transwell inserts (3.0μm pore size) in endothelial growth medium.
- Add Pericytes: Culture human brain vascular pericytes on the bottom of the Transwell plates in pericyte medium. Allow establishment for 24-48 hours.
- Incorporate Astrocytes: Plate human astrocytes on the underside of the Transwell inserts (inverted orientation) for 4 hours, then revert to normal orientation.
- Validation Measurements: Assess transendothelial electrical resistance (TEER) using volt-ohm meter, with values >150 Ω×cm² indicating intact barrier function. Perform permeability assays using marker molecules (e.g., sodium fluorescein, 376 Da; dextran, 70 kDa).
Application: This model enables screening of candidate therapeutics for BBB permeability and assessment of cytoskeletal-targeting compounds on barrier integrity [75] [74].
Ligand-Conjugated Nanoparticle Preparation
Protocol 2: Transferrin-Modified Liposome Fabrication
- Lipid Film Formation: Dissolve phospholipids (e.g., DSPC, cholesterol, PEG-DSPE) in chloroform at 10:3:1 molar ratio. Evaporate solvent under reduced pressure to form thin lipid film.
- Hydration and Extrusion: Hydrate lipid film with aqueous solution containing therapeutic agent (e.g., oligonucleotides, small molecules). Freeze-thaw cycle five times, then extrude through polycarbonate membranes (100nm pore size) using mini-extruder.
- Ligand Conjugation: Activate transferrin with Traut's reagent (2-iminothiolane) for thiolation. Separate excess reagent using desalting column. Incubate activated transferrin with maleimide-functionalized liposomes for 12 hours at 4°C.
- Purification and Characterization: Remove unconjugated transferrin by size exclusion chromatography. Characterize particle size (dynamic light scattering), surface charge (zeta potential), ligand density (BCA assay), and drug loading efficiency (HPLC) [76].
Assessment of Cytoskeletal Drug Effects
Protocol 3: Evaluation of Microtubule Stabilization
- Neuronal Culture: Differentiate SH-SY5Y cells or primary cortical neurons for 7 days in vitro.
- Treatment Application: Incubate with test compounds (e.g., tau aggregation inhibitors, microtubule-stabilizing agents) for 24-48 hours.
- Immunofluorescence Staining: Fix cells with 4% paraformaldehyde, permeabilize with 0.1% Triton X-100, block with 5% BSA. Incubate with primary antibodies (anti-α-tubulin, anti-acetylated tubulin, anti-tau) overnight at 4°C, then with fluorescent secondary antibodies.
- Image Acquisition and Analysis: Capture images using confocal microscopy with consistent settings. Quantify microtubule density, network integrity, and post-translational modifications using ImageJ software with customized macros [22] [21].
Figure 2: Integrated Experimental Workflow for BBB-Cytoskeleton Therapeutic Development. This diagram outlines the key stages in developing and evaluating therapeutics that target cytoskeletal pathology following BBB penetration, highlighting the connection between in vitro screening and in vivo validation.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for BBB and Cytoskeletal Studies
| Reagent Category | Specific Examples | Research Applications | Key Features |
|---|---|---|---|
| BBB Model Systems | hCMEC/D3 cell line, Primary HBMECs, In vitro BBB kits | Permeability studies, Transport mechanism elucidation | Human origin, Barrier properties, Expression of relevant transporters |
| Cytoskeletal Markers | Anti-tau antibodies (AT8, PHF1), Anti-α-tubulin, Anti-neurofilament | Pathology assessment, Drug efficacy evaluation | Phospho-specificity, Isoform recognition, Modification sensitivity |
| Nanoparticle Components | DSPC phospholipids, PEG-DSPE, PLGA polymers | Drug carrier fabrication, Delivery optimization | Biocompatibility, Functionalization capacity, Controlled release |
| Targeting Ligands | Transferrin, Lactoferrin, RVG29 peptide | BBB translocation enhancement, Tissue-specific targeting | Receptor specificity, Low immunogenicity, Conjugation compatibility |
| Kinase Modulators | GSK-3β inhibitors (CHIR99021), CDK5 inhibitors (Roscovitine) | Tau phosphorylation studies, Pathway analysis | Selectivity, Potency, Cellular permeability |
| Animal Models | APP/PS1 mice, P301L tau mice, SOD1G93A mice | Therapeutic efficacy evaluation, Biodistribution studies | Pathological relevance, Reproducibility, Translational value |
Emerging Therapeutic Approaches and Clinical Translation
Kinase-Targeted Strategies for Cytoskeletal Pathology
Protein kinases represent promising therapeutic targets for modulating cytoskeletal pathology in neurodegenerative diseases [66]. Several kinase pathways have been implicated in aberrant phosphorylation of cytoskeletal proteins:
- GSK-3β (Glycogen Synthase Kinase-3β): Hyperphosphorylates tau at multiple sites and is linked to both amyloid and tau pathology in AD [66]. GSK-3β inhibitors have shown promise in reducing tau phosphorylation and improving cognitive function in preclinical models.
- CDK5 (Cyclin-Dependent Kinase 5): Activated by p25/p35 fragments, CDK5 phosphorylates tau, neurofilaments, and other substrates [66]. Dysregulation of CDK5 contributes to neurodegeneration through cytoskeletal disruption.
- LRRK2 (Leucine-Rich Repeat Kinase 2): Mutations in LRRK2 are associated with familial PD and may impact cytoskeletal dynamics through regulation of microtubule assembly and vesicular trafficking [66].
- MAPKs (Mitogen-Activated Protein Kinases): Multiple MAPK pathways (JNK, p38) are activated in neurodegenerative conditions and contribute to cytoskeletal protein phosphorylation [66].
Kinase inhibitor development faces challenges including selectivity, brain penetration, and long-term safety. However, novel approaches such as antisense oligonucleotides (ASOs) and gene therapy vectors offer alternative strategies for modulating kinase activity in the CNS [66].
Gene Editing and Oligonucleotide Therapies
Advanced genetic therapies show considerable promise for directly targeting cytoskeletal pathology:
- Antisense Oligonucleotides (ASOs): Tofersen, an ASO targeting SOD1 mRNA, has demonstrated efficacy for ALS treatment [73]. Similarly, ASOs targeting tau (BIIB080/IONIS-MAPTRx) and SNCA (α-synuclein gene) are in clinical development [73] [66].
- CRISPR-Based Approaches: Gene editing technologies enable direct correction of disease-causing mutations or modulation of disease-associated genes. Dual-AAV CRISPR systems are being developed for Huntington's disease, targeting mutant huntingtin expression while preserving normal gene function [73].
- RNA-Targeting CRISPR: CRISPR-Cas13 systems can target RNA rather than DNA, offering potential for transient modulation of gene expression without permanent genomic changes [73].
Clinical Translation Challenges and Solutions
The translation of BBB-penetrating cytoskeletal therapies from preclinical models to clinical application faces several hurdles:
- Species Differences: BBB biology and disease pathology often differ between animal models and humans, complicating prediction of therapeutic efficacy [73].
- Biomarker Development: Sensitive and specific biomarkers are needed to monitor target engagement, disease progression, and treatment response [31].
- Manufacturing Complexity: Sophisticated delivery systems (e.g., ligand-decorated nanoparticles, viral vectors) present challenges for scalable, reproducible manufacturing under Good Manufacturing Practice standards [73].
- Regulatory Pathways: Novel therapeutic-diagnostic combinations and advanced delivery systems may require development of new regulatory frameworks [73].
Potential solutions include improved animal models that better recapitulate human disease, advanced imaging techniques for monitoring target engagement, and iterative design processes incorporating artificial intelligence for nanoparticle optimization [76].
The convergence of advanced BBB penetration strategies with precise targeting of cytoskeletal pathology represents a promising frontier in neurodegenerative disease therapeutics. The integration of multiple approaches—nanoparticle-mediated delivery, biological transport mechanisms, and physical barrier modulation—offers the potential to overcome the longstanding challenge of CNS drug delivery. Simultaneously, growing understanding of cytoskeletal dysfunction mechanisms across neurodegenerative diseases provides increasingly sophisticated molecular targets for therapeutic intervention.
Future progress will likely depend on several key developments: First, personalized approaches that match specific delivery strategies to individual patient characteristics, including BBB properties and disease subtype. Second, combination therapies that simultaneously address multiple aspects of neurodegeneration, including protein aggregation, neuroinflammation, and cytoskeletal disruption. Third, advanced diagnostic techniques that enable early intervention and precise monitoring of treatment effects. Finally, continued innovation in delivery platform engineering, particularly the integration of artificial intelligence for rational design of BBB-penetrating therapeutics.
The successful translation of these innovative approaches will require interdisciplinary collaboration between neuroscientists, drug delivery experts, clinicians, and regulatory specialists. While significant challenges remain, the current trajectory of research offers genuine hope for effective treatments that can alter the progression of neurodegenerative diseases by targeting their fundamental cytoskeletal pathology.
The timing of therapeutic intervention is a pivotal factor influencing success in treating neurodegenerative diseases. Mounting evidence confirms that early intervention, during mild cognitive impairment (MCI) or prodromal stages, provides significantly superior outcomes compared to treatment initiated after overt structural degeneration and clinical symptoms have manifested. This technical guide examines the critical window for intervention within the context of cytoskeletal defects in neurodegeneration, synthesizing current research on pathological timelines, detection methodologies, and emerging therapeutic strategies. For researchers and drug development professionals, understanding these temporal considerations is essential for designing effective clinical trials and developing disease-modifying therapies that target the earliest phases of neuronal decline, when cytoskeletal integrity remains largely intact and neuronal loss is potentially reversible.
The Clinical Imperative for Early Intervention
The approval of disease-modifying Alzheimer's disease (AD) therapies has exposed a critical challenge in healthcare systems: identifying patients during the mild cognitive impairment (MCI) stage when interventions demonstrate optimal efficacy. Clinical trials for lecanemab showed a 27% reduction in cognitive decline compared to placebo, with notably stronger effects in earlier-stage patients, while donanemab demonstrated 35% slowing of progression in early symptomatic AD [77]. Post-hoc analyses from these studies consistently indicate that therapeutic benefit directly correlates with intervention timing.
The biological rationale for this critical window is well-characterized. In Alzheimer's disease, amyloid accumulation begins approximately 15-20 years before clinical manifestation, followed by tau pathology, neurodegeneration, and eventual cognitive symptoms [77]. The MCI stage represents the earliest clinically identifiable phase of this continuum and the optimal intervention point for disease-modifying therapies. As one neurologist emphasized in stakeholder interviews: "The battle against Alzheimer's will be determined by our ability to identify and treat patients during the MCI window" [77].
The consequences of delayed detection are profound. For patients, delayed diagnosis means irreversible neurodegeneration and cognitive decline that might have been prevented with earlier intervention. From a systems perspective, late-stage dementia care requires substantially more resources than early intervention, with increased costs stemming from more intensive medical needs, safety concerns, and eventual residential care requirements [77].
Table 1: Efficacy of Interventions Based on Disease Stage
| Disease Stage | Therapeutic Goal | Representative Efficacy | Cytoskeletal Integrity |
|---|---|---|---|
| Preclinical | Prevention | Potentially maximal (data limited) | Largely intact |
| Mild Cognitive Impairment (MCI) | Disease modification | 27-35% slowing of decline [77] | Early cytoskeletal modifications detectable |
| Early Dementia | Symptomatic + disease modification | Modest slowing of decline | Significant tau pathology & cytoskeletal disruption |
| Established Dementia | Palliative/symptomatic | Minimal disease modification | Widespread neuronal loss & cytoskeletal collapse |
Cytoskeletal Defects as Early Pathological Hallmarks
Cytoskeletal abnormalities represent one of the earliest detectable pathological changes in neurodegenerative disease processes, often preceding overt structural degeneration by months or years. Research across multiple neurodegenerative conditions demonstrates that cytoskeletal modifications serve as sensitive indicators of initial neuronal stress.
Temporal Sequence of Cytoskeletal Disruption
In the DBA/2J mouse model of glaucoma, a systematic examination of cytoskeletal protein modifications revealed a distinct spatiotemporal progression. Phosphorylated neurofilament-heavy chain (pNF-H) elevations appeared within the optic nerve and superior colliculus of 8-10 month-old mice, but were not evident in the retina until 12-15 months, suggesting cytoskeletal modifications first appear in distal retinal projections [78]. Similarly, elevations in hyperphosphorylated tau occurred in optic nerve and superior colliculus between 3-8 months, while retinal accumulations occurred at 12-15 months [78].
Perhaps most significantly, elevations in calpain-mediated spectrin breakdown products appeared in optic nerve and superior colliculus at the earliest ages examined, well before axonal transport deficits become evident [78]. This suggests that spectrin proteolysis may represent one of the initial cytoskeletal alterations in neurodegenerative processes, potentially making it a sensitive marker for early detection.
Table 2: Timeline of Cytoskeletal Protein Modifications in Neurodegeneration
| Cytoskeletal Element | Modification Type | Earliest Detection | Functional Consequence |
|---|---|---|---|
| Spectrin | Calpain-mediated cleavage (SBDP 145/150) | Pre-symptomatic stage [78] | Membrane destabilization, loss of cytoskeletal anchoring |
| Tau | Hyperphosphorylation (ptau-231) | Early symptomatic stage [78] | Microtubule destabilization, impaired axonal transport |
| Neurofilament | Hyperphosphorylation (pNF-H) | Early symptomatic stage [78] | Altered axonal caliber, impaired transport |
| Tubulin | Decreased β-tubulin levels | Symptomatic stage [78] | Microtubule network destabilization |
Cytoskeletal Integrity and Nodal Stability
Research on the cytoskeletal scaffolding protein ankyrin G (AnkG) at nodes of Ranvier provides crucial insights into the relationship between cytoskeletal integrity and neuronal function. Studies demonstrate that early loss of AnkG creates immature nodes with abnormal morphology that undergo accelerated destabilization within a month, resulting in rapid voltage-gated sodium channel and βIV spectrin loss [79]. In contrast, late ablation of AnkG from established nodal complexes leads to slow but progressive destabilization over 10 months, primarily affecting βIV spectrin, followed by sodium channels [79].
These findings reveal the differential vulnerability of cytoskeletal components based on developmental stage and suggest that early cytoskeletal disruptions create cascading effects on neuronal excitability and function. The time-dependent disintegration of nodal components following AnkG ablation underscores the importance of early intervention to preserve cytoskeletal integrity before compensatory mechanisms are overwhelmed.
Methodologies for Detecting Early Cytoskeletal Pathology
Advanced Protein Quantification Techniques
Capillary-based electrophoresis and multiplex immunosorbent assays enable precise quantification of cytoskeletal protein modifications in tissue specimens and biofluids. These techniques allow researchers to detect subtle changes in post-translationally modified cytoskeletal proteins, including:
- Hyperphosphorylated neurofilament-heavy chain (pNF-H)
- Phosphorylated tau (ptau-231)
- Calpain-mediated spectrin breakdown products (SBDP 145/150)
- β-tubulin isoforms
- Amyloid-β42 (indirect cytoskeletal effects) [78]
These assays can be performed on tissue homogenates from specific neuroanatomical regions to map the spatiotemporal progression of cytoskeletal pathology, as demonstrated in the DBA/2J glaucoma model where distal-to-proximal progression of cytoskeletal modifications was observed [78].
Digital Biomarkers and Neurophysiological Monitoring
Next-generation assessment tools are revolutionizing early detection capabilities for neurodegenerative processes. Digital biomarkers represent a promising avenue for identifying subtle functional changes associated with early cognitive decline:
- Speech analysis tools can detect subtle linguistic changes through automated assessment of semantic content, syntactic complexity, and acoustic features [77]
- Eye movement tracking reveals attentional and executive function changes
- Fine motor assessments through digital devices provide information about cognitive status [77]
Neurophysiological markers, particularly quantitative electroencephalography (EEG) and event-related potentials, complement behavioral digital biomarkers by providing direct insight into brain function. These measures are sensitive to subtle cognitive changes associated with MCI and offer the advantage of being non-invasive and cost-effective for longitudinal monitoring [77].
Early Detection Workflow: Multimodal biomarker integration for identifying early cytoskeletal pathology.
Experimental Protocol: Cytoskeletal Protein Analysis in Neurodegeneration Models
Objective: To quantify cytoskeletal protein modifications and their relationship to axonal transport deficits in experimental neurodegeneration.
Materials:
- Animal model (e.g., DBA/2J mice for glaucoma, transgenic tauopathy models)
- Primary antibodies against pNF-H, ptau-231, spectrin breakdown products, β-tubulin
- Capillary electrophoresis system (e.g., Simple Western/ProteinSimple)
- Multiplex immunosorbent assay platform
- Confocal microscopy system
- Anterograde tract tracing reagents (e.g., cholera toxin B subunit)
Procedure:
- Staging and Grouping: Group animals by age and disease stage (pre-symptomatic, early symptomatic, late symptomatic)
- Anterograde Tract Tracing: Administer tract tracer to assess axonal transport integrity
- Tissue Collection and Processing: Euthanize animals and dissect relevant CNS regions
- Protein Extraction and Quantification: Homogenize tissues and quantify protein concentration
- Capillary Electrophoresis: Separate and detect cytoskeletal proteins using specific antibodies
- Multiplex Immunosorbent Assay: Simultaneously quantify multiple cytoskeletal markers
- Immunofluorescence and Confocal Microscopy: Visualize spatial distribution of cytoskeletal proteins
- Data Analysis: Correlate cytoskeletal protein levels with transport outcomes and age [78]
Key Controls:
- Age-matched non-transgenic or disease-resistant controls (e.g., DBA/2J-Gpnmb+ for glaucoma studies)
- Verification of antibody specificity using knockout tissues
- Normalization to housekeeping proteins
- Blinded analysis to prevent experimental bias
Therapeutic Implications and Intervention Strategies
Targeting Early Cytoskeletal Pathology
The recognition that cytoskeletal defects occur early in neurodegenerative processes presents unique therapeutic opportunities. Interventions that stabilize microtubules, inhibit pathological tau phosphorylation, or prevent spectrin proteolysis may be most effective when administered during pre-symptomatic or early symptomatic stages.
Recent advances in blood biomarkers for detecting early tau pathology provide a critical tool for identifying candidates for early intervention. These biomarkers can detect emerging pathology long before PET imaging reveals later-stage tau accumulation, enabling researchers to enroll participants in clinical trials at optimal timepoints for therapeutic efficacy [80].
Emerging Therapeutic Approaches
Stem cell therapies and engineered exosomes represent promising approaches for addressing cytoskeletal defects in neurodegeneration. Mesenchymal stem cell-derived exosomes can cross the blood-brain barrier to deliver therapeutic molecules directly to the brain, reducing neuroinflammation, oxidative stress, and promoting neuronal regeneration [81]. Recent advances in exosome engineering, including surface modifications and therapeutic agent loading, have improved targeting, stability, and delivery across the blood-brain barrier [81].
Holistic anti-aging strategies complement targeted therapeutic approaches. Given that ageing is the primary risk factor for neurodegenerative diseases, interventions that target fundamental aging processes may provide broader protection against multiple neurodegenerative conditions [82]. This integrated approach represents a promising strategy to effectively prevent, pause, or slow progression of neurodegenerative diseases.
Table 3: Research Reagent Solutions for Cytoskeletal Defect Investigation
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Antibodies for Cytoskeletal Proteins | Anti-pNF-H, anti-pTau (AT270/AT180), anti-spectrin breakdown product | Protein quantification, immunohistochemistry, Western blot | Phospho-specificity validation required |
| Digital Assessment Tools | Speech analysis software, eye-tracking systems, digital motor tasks | Early detection, longitudinal monitoring | Practice effects must be accounted for in repeated measures |
| Stem Cell-Derived Exosomes | MSC-exosomes, engineered exosomes with targeting ligands | Therapeutic delivery, neuroprotection, cytoskeletal stabilization | Loading efficiency, biodistribution, and targeting specificity |
| Animal Models of Cytoskeletal Defects | DBA/2J mice, AnkG ablation models, tauopathy models | Pathogenesis studies, therapeutic screening | Species-specific differences in cytoskeletal organization |
The timing of therapeutic intervention is unequivocally critical in neurodegenerative diseases, with early intervention during MCI or pre-symptomatic stages offering substantially greater potential for meaningful clinical impact. Cytoskeletal defects represent particularly promising targets for early intervention strategies, as they appear early in disease processes and contribute directly to neuronal dysfunction.
Future research directions should prioritize:
- Validation of ultrasensitive cytoskeletal biomarkers in biofluids for early detection
- Development of cytoskeleton-stabilizing compounds with favorable blood-brain barrier penetration
- Advanced delivery systems (e.g., engineered exosomes) for targeted cytoskeletal therapy
- Multimodal intervention strategies that combine cytoskeletal stabilization with proteostasis restoration and anti-inflammatory approaches
For researchers and drug development professionals, focusing on the "critical window" of early disease stages and leveraging advanced detection methodologies will be essential for developing effective therapies that meaningfully alter neurodegenerative disease trajectories.
Addressing Compensatory Mechanisms and Pathway Redundancies
The progressive nature of neurodegenerative diseases reflects a complex interplay between primary pathological insults and the nervous system's capacity to mitigate damage through compensatory mechanisms and pathway redundancies. Rather than representing simple linear progression of protein aggregation or neuronal loss, conditions like Alzheimer's disease (AD), Parkinson's disease (PD), and Huntington's disease (HD) involve sophisticated biological responses that initially preserve function despite underlying pathology. The cytoskeletal network serves as both a target for degeneration and a platform for compensatory restructuring, with emerging evidence suggesting that septin cytoskeletal proteins function as crucial regulators in neuronal resilience. Understanding these adaptive processes provides critical insights for therapeutic development, particularly for interventions aimed at enhancing endogenous compensation or delaying symptomatic onset.
Compensatory evolution represents a fundamental biological principle wherein systems develop alternative mechanisms to overcome functional deficits. Research on yeast genomes demonstrates that 68% of gene knock-out genotypes reached near wild-type fitness through accumulation of adaptive mutations elsewhere in the genome, demonstrating the remarkable capacity for biological systems to compensate for even fundamental genetic losses [83]. In neurodegenerative contexts, this principle manifests as cellular compensation that masks early disease pathology, with motor symptoms in PD only materializing after 50-60% of dopaminergic neurons in the substantia nigra have degenerated [84]. This delayed symptom onset suggests effective compensatory mechanisms operating during preclinical stages, highlighting the potential for therapeutic strategies that enhance or prolong these natural adaptive responses.
Analytical Frameworks for Studying Compensation
Quantitative Assessment of Compensatory Capacity
Research across biological systems has established methodologies for quantifying compensatory potential and mapping its genomic and phenotypic manifestations. These approaches allow researchers to measure compensatory capacity and identify key molecular players in redundant pathways.
Table 1: Quantitative Metrics for Assessing Compensatory Mechanisms
| Metric | Measurement Approach | Experimental System | Key Findings |
|---|---|---|---|
| Relative Fitness Improvement (RFI) | (Evolved fitness/Initial fitness)-1 | Yeast gene knock-out models | Rapid fitness recovery observed in 68% of deleted gene genotypes [83] |
| Relative Compensation (RC) | Fraction of initial fitness defect compensated | Laboratory evolution experiments | Genotypes with lower initial fitness more likely to be compensated [83] |
| Symptom Threshold | Percentage of neuronal loss before symptom onset | PD post-mortem studies | Motor symptoms emerge only after 50-60% dopaminergic neuron loss [84] |
| Pathway Redundancy Index | Activation magnitude of parallel pathways upon primary pathway inhibition | Signaling pathway analysis in cell models | Two core proliferation pathways can substitute for each other in cancer resistance [85] |
Conceptual Models of Compensation
The genotype network model provides a framework for understanding how compensatory mechanisms operate across biological systems. In this model, nodes represent genotypes connected by single mutational steps, with populations occupying multiple nodes potentially accessing different phenotypes from each genotype [86]. This model reveals that cryptic genetic sequences with attenuated effects can build up across individuals, providing alleles that may later contribute to adaptation when co-opted. For quantitative traits influenced by multiple cryptic sequences, even clonal populations may access diverse adaptive phenotypes through co-option of different cryptic sequences, demonstrating that adaptive potential resides in genomes rather than just population diversity [86].
In neurodegenerative diseases, compensatory mechanisms operate across multiple temporal scales, from developmental compensation that establishes altered neural circuits early in life to acute compensatory responses to ongoing pathology. Evidence suggests that HD has a developmental component, with tissues from human fetuses expressing mutant HTT exhibiting defects in neuro-progenitor cell polarity, differentiation, and cell cycle progression [84]. These developmental alterations may represent failed compensation or alternatively establish neural circuits that are inherently more vulnerable to later-life degeneration.
Experimental Approaches for Mapping Compensatory Pathways
Methodologies for Pathway Analysis
Elucidating compensatory mechanisms requires sophisticated experimental approaches that can detect both primary pathways and redundant backup systems. The following methodologies have proven particularly valuable for mapping these complex biological networks:
Gene Deletion and Evolutionary Compensation Studies
- Protocol: Initiate laboratory evolutionary experiments with gene knock-out mutant strains showing slow but non-zero growth compared to wild-type controls
- Propagation: Cultivate populations in parallel (four replicates per null mutation) with 0.5% of each culture diluted into fresh medium every 48 hours
- Duration: Propagate populations for approximately 400 generations to allow compensatory evolution
- Fitness Assessment: Monitor growth rates in liquid cultures for all starting and evolved populations
- Genomic Analysis: Identify compensatory mutations through whole-genome sequencing of evolved lines [83]
Signaling Pathway Redundancy Mapping
- Experimental Design: Inhibit primary pathways using targeted inhibitors or genetic approaches and monitor activation of alternative pathways
- Measurement Techniques: Phospho-proteomic profiling, RNA sequencing, and metabolic flux analysis
- Cross-Species Validation: Utilize models from yeast to human stem cells to identify evolutionarily conserved compensatory networks [84]
Table 2: Experimental Models for Studying Compensatory Mechanisms in Neurodegeneration
| Model System | Applications | Advantages | Limitations |
|---|---|---|---|
| Yeast gene knock-out libraries | Study of evolutionary compensation | High-throughput, controlled genetics | Simplified model distant from human neurobiology |
| Human embryonic stem cells (hESCs) | Developmental aspects of neurodegeneration | Human-relevant, can model patient-specific mutations | Ethical considerations, limited maturity of differentiated neurons |
| Induced pluripotent stem cells (iPSCs) | Patient-specific disease modeling | Personalized approach, recapitulates human genetics | Variable differentiation efficiency between lines |
| Animal models (mouse, rat, Xenopus) | In vivo pathway analysis and behavioral correlates | Intact neural circuits, behavioral assessment | Species-specific differences in neurobiology |
| Post-mortem human brain tissue | Validation of human relevance | Direct human pathology evidence | Limited to end-stage disease, post-mortem changes |
Visualization of Compensatory Pathway Activation
The following diagram illustrates the conceptual framework of compensatory evolution following neuronal pathway disruption:
Compensatory Mechanisms in Neurodegenerative Diseases
Cytoskeletal Compensation: Septins as Central Regulators
The cytoskeleton serves not only as structural framework but as a dynamic signaling platform that undergoes substantial reorganization in response to neurodegenerative stressors. Septins, GTP-binding cytoskeletal proteins, have emerged as crucial components in neuronal resilience, functioning as scaffolding components and diffusion barriers at specialized membrane domains including dendritic spines, axon initial segments, and synaptic terminals [87]. In the nervous system, specific septin isoforms including SEPT3, SEPT5, and SEPT7 contribute to dendritic spine formation, neurotransmitter vesicle trafficking, and axonal integrity, positioning them as key players in structural compensation against neurodegeneration.
Septins facilitate cytoskeletal crosstalk between microtubules and actin filaments, creating a coordinated compensatory response to maintain neuronal structure and function. Recent research has revealed that septins regulate how microtubules guide actin filament growth, particularly in the formation of growth cones that direct neuronal development [87]. This microtubule-actin interaction represents a fundamental compensatory mechanism wherein the architecture of microtubules functions as a template for actin polymerization, enabling structural reorganization in response to degenerative insults. Alterations in septin expression or assembly disrupt synaptic architecture and neuroplasticity, emphasizing their role in maintaining neuronal homeostasis against pathological stressors.
Signaling Pathway Compensation
Multiple evolutionarily conserved signaling pathways demonstrate remarkable redundancy in neurodegenerative contexts, providing compensatory routes when primary pathways are compromised:
TGFβ Signaling in Huntington's Disease
- Compensatory Role: Asymptomatic HD patients show low levels of serum TGFβ, with post-mortem examination revealing reduced TGFβ expression in cortical neurons [84]
- Mechanism: Expression of mutant HTT reduces TGFβ mRNA and protein levels in cultured astrocytes and striatal cell lines
- Developmental Component: Early TGFβ signaling regulates density-dependent induction of apical/basolateral polarity, with mutant HTT disrupting receptor localization and leading to increased mesendodermal patterning and contracted ectodermal compartment [84]
Wnt Signaling in Parkinson's Disease
- Neuroprotective Role: Wnt signaling regulates neuronal differentiation, axonal extension, synapse formation, and neurogenesis, with decreased activity in PD brains worsening age-dependent inflammation and oxidative stress [84]
- Compensatory Activation: Multiple genes in the Wnt pathway are hypermethylated in PD brains, corresponding to reduced protein expression
- Therapeutic Targeting: LRRK2, commonly mutated in PD, inhibits Wnt/β-catenin pathway while activating Wnt/planar cell polarity pathway, suggesting pathway-specific compensatory effects [84]
Notch Signaling in Alzheimer's Disease
- Developmental Role: Notch signaling regulates quiescence and differentiation of neural stem cells during development [84]
- Compensatory Reactivation: Reactivation of developmental pathways may provide limited compensation in early AD stages
- Therapeutic Implications: Notch pathway modulation represents potential approach for enhancing compensatory mechanisms
The following diagram illustrates key compensatory signaling pathways in neurodegeneration:
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Studying Compensatory Mechanisms
| Reagent/Category | Specific Examples | Research Application | Function in Experimental Design |
|---|---|---|---|
| Stem Cell Models | Mesenchymal stem cells (MSCs), Neural stem cells (NSCs), Induced pluripotent stem cells (iPSCs) | Disease modeling, Transplantation studies | Replace damaged neurons, modulatory neuroinflammation, study developmental compensation [81] |
| Gene Editing Tools | CRISPR-Cas9 systems, RNA interference (RNAi) | Target validation, Pathway manipulation | Selective inhibition of primary pathways to reveal compensatory mechanisms [84] |
| Small Molecule Inhibitors/Activators | LRRK2 inhibitors, GSK3β inhibitors, TGFβ pathway modulators | Signaling pathway analysis | Selective pathway manipulation to test redundancy and compensation [84] |
| Septin Research Tools | SEPT3/5/7 antibodies, Septin GTPase activity assays, Septin polymerization inhibitors | Cytoskeletal compensation studies | Investigate structural compensatory mechanisms in neuronal models [87] |
| Exosome Engineering Tools | MSC-derived exosomes, Surface-modified exosomes, Therapeutic cargo-loaded exosomes | Therapeutic delivery development | Cross BBB to deliver therapeutic molecules, reduce neuroinflammation, promote neuronal regeneration [81] |
| Multi-Omics Platforms | Single-cell RNA sequencing, Spatial transcriptomics, Phospho-proteomics | Comprehensive pathway mapping | Identify compensatory network activation across molecular layers [88] |
Therapeutic Implications and Future Directions
Compensation-Targeted Therapeutic Strategies
The growing understanding of compensatory mechanisms in neurodegeneration opens new avenues for therapeutic intervention aimed at enhancing endogenous resilience pathways:
Septin-Targeted Approaches
- Stabilization Strategies: Development of small molecules that stabilize septin cytoskeletal structures against neurodegenerative insults
- Expression Modulation: Regulatory approaches to maintain appropriate septin isoform expression in vulnerable neuronal populations
- Post-Translational Modification: Targeting phosphorylation states that regulate septin polymerization and function [87]
Pathway Reinforcement Strategies
- Redundant Pathway Activation: Therapeutic enhancement of alternative pathways that can compensate for defective primary pathways
- Developmental Pathway Reactivation: Controlled re-engagement of neurodevelopmental mechanisms that may provide structural and functional compensation
- Combination Therapies: Simultaneous targeting of multiple compensatory pathways to create therapeutic redundancy [85]
Experimental Therapeutics and Clinical Translation
Emerging therapeutic platforms show particular promise for targeting compensatory mechanisms:
Stem Cell-Derived Exosome Therapies
- Mechanism: Exosomes can cross the blood-brain barrier to deliver therapeutic molecules directly to the brain, offering less invasive alternatives to stem cell transplantation
- Compensatory Enhancement: Mesenchymal stem cell-derived exosomes have demonstrated significant potential in preclinical models by reducing neuroinflammation, oxidative stress, and promoting neuronal regeneration [81]
- Engineering Approaches: Surface modifications, therapeutic agent loading, and transgenic modifications improve targeting, stability, blood-brain barrier delivery, and neural cell interactions [81]
Gene Therapy Approaches
- Compensation Engineering: Introduction of genes that enhance compensatory pathway activation or provide redundant functions
- Pathway Modulation: Selective enhancement of alternative pathways that can bypass defective neuronal functions
- Clinical Status: Currently in early to mid-development phases for neurodegenerative applications [81]
The progressive collapse of compensatory mechanisms represents a critical transition point in neurodegenerative diseases. By understanding and therapeutically targeting these adaptive systems, we may develop interventions that prolong the preclinical phase of diseases, delay symptomatic onset, and ultimately preserve neurological function in the face of ongoing pathology. The cytoskeletal framework, particularly septin-mediated structural compensation, provides a promising target for these therapeutic approaches aimed at enhancing the brain's innate resilience mechanisms.
Biomarker Validation for Patient Stratification and Treatment Response Monitoring
In contemporary biomedical research, biomarkers are defined as measurable characteristics that indicate normal biological processes, pathogenic processes, or responses to an exposure or intervention, including therapeutic interventions [89]. They can be derived from radiographic, physiologic, histologic, or molecular features [89]. The validation of these biomarkers is paramount for tailoring treatments and predicting patient outcomes, particularly in complex disease areas such as neurodegeneration and oncology. A Comprehensive Oncological Biomarker Framework that integrates genetic and molecular testing, imaging, histopathology, multi-omics, and liquid biopsy can generate a molecular fingerprint for each patient, supporting individualized diagnosis, prognosis, treatment selection, and response monitoring [89]. Within the context of neurodegeneration, where cytoskeletal defects are increasingly implicated in disease mechanisms, the need for robust, validated biomarkers is critical for early diagnosis, accurate patient stratification, and monitoring treatment efficacy [90] [91].
This guide provides an in-depth technical examination of biomarker validation, focusing on its application for patient stratification and treatment response monitoring, with specific consideration of the role of cytoskeletal alterations in neurodegenerative diseases.
Biomarker Classes and Clinical Applications
Biomarkers are commonly classified into several main categories based on their clinical application [89] [91]. Understanding these classes is the first step in designing a validation strategy.
Table 1: Key Biomarker Classes and Their Clinical Utility
| Biomarker Class | Primary Function | Example in Neurodegeneration | Example in Oncology |
|---|---|---|---|
| Diagnostic | Indicates the presence of a disease or subtype of a disease [89] [91]. | CSF Aβ42 and p-tau for Alzheimer's disease [91]. | PD-L1 expression to confirm eligibility for immunotherapy [89]. |
| Prognostic | Provides information on the likely course of a disease, independent of treatment [91]. | Total tau (t-tau) in CSF as a marker of axonal damage intensity [91]. | Tumor Mutational Burden (TMB) as a general prognostic indicator [89]. |
| Predictive | Identifies individuals more likely to respond to a specific therapeutic intervention [89]. | (Under investigation for cytoskeletal-targeted therapies). | Microsatellite Instability (MSI) predicting response to immune checkpoint inhibitors [89]. |
| Pharmacodynamic | Demonstrates that a biological response has occurred in an individual who has received a therapeutic intervention [89]. | Changes in neurofilament light chains (NFL) following treatment [91]. | Reduction in circulating tumor DNA (ctDNA) post-treatment [89]. |
| Stratification | Used to categorize a patient population into subgroups for clinical trials or treatment. | Cytoskeletal gene expression signatures (e.g., ENC1, NEFM) in Alzheimer's disease [90]. | Integrative multi-omics signatures for patient subgrouping [92]. |
Technical Validation Methodologies
A robust biomarker validation framework relies on a suite of sophisticated analytical techniques. Each method offers distinct advantages and faces specific challenges that must be addressed during validation.
Core Detection Technologies
Table 2: Core Methodologies for Biomarker Detection and Validation
| Methodology | Principle | Key Applications in Validation | Technical Considerations |
|---|---|---|---|
| Immunohistochemistry (IHC) | Uses antibodies to visualize protein targets within tissue sections [89]. | Spatial localization and semi-quantification of protein biomarkers (e.g., tau proteinopathies). | Requires high-quality, validated antibodies; results can be subjective [89]. |
| Enzyme-Linked Immunosorbent Assay (ELISA) | Immobilizes antibodies or antigens on solid surfaces for quantification [89]. | Quantifying specific proteins in biofluids (e.g., CSF Aβ42, t-tau, α-synuclein) [91]. | Potential for cross-reactivity; innovations like streptavidin-biotin complexes enhance sensitivity [89]. |
| Biosensors | Uses biorecognition elements and signal transducers to convert biological events into measurable signals [89]. | Rapid, non-invasive detection of enzymes, antibodies, and microRNAs [89]. | High sensitivity but risk of false positives from contamination [89]. |
| Surface-Enhanced Raman Spectroscopy (SERS) | Leverages electromagnetic enhancements at metal surfaces for ultra-sensitive detection [89]. | Distinguishing structurally similar molecules in complex samples; multi-target detection [89]. | Challenges with substrate stability and reproducibility [89]. |
| Liquid Biopsy | Analysis of circulating biomarkers such as cell-free DNA (cfDNA), circulating tumor cells, or extracellular vesicles (EVs) [89]. | Provides a real-time window into tumor dynamics and treatment response; minimal invasiveness [89]. | Sensitivity to detect low-abundance biomarkers in early disease stages [89]. |
Multi-Omics Integration for Stratification
The integration of multi-omics data is transforming validation by providing a comprehensive view of disease biology. This approach is critical for addressing tumor heterogeneity in oncology and the complex pathology of neurodegenerative diseases [92]. Multi-omics encompasses:
- Genomics: Examines the full genetic landscape, identifying mutations, structural variations, and copy number variations (CNVs) that drive disease initiation and progression via whole genome and whole exome sequencing [92].
- Transcriptomics: Analyzes gene expression, providing a snapshot of pathway activity and regulatory networks. Techniques like RNA sequencing and single-cell RNA sequencing reveal the dynamics of the tissue microenvironment [92].
- Proteomics: Investigates the functional state of cells by profiling proteins, including post-translational modifications, using mass spectrometry and immunofluorescence [92].
By integrating these data layers with computational models, researchers can identify distinct patient subgroups based on molecular and immune profiles for precise patient selection in trials [92]. Tools like IntegrAO, which integrates incomplete multi-omics datasets using graph neural networks, and NMFProfiler, which identifies biologically relevant signatures across omics layers, are essential for robust stratification and biomarker discovery [92].
Experimental Workflow for Biomarker Validation
The following diagram outlines a generalized workflow for the discovery and validation of biomarkers, from sample processing to clinical application.
Cytoskeletal Biomarkers in Neurodegeneration
The cytoskeleton, a network of intracellular filamentous proteins, is essential for maintaining cellular shape, integrity, and generating forces for cellular motility [90]. Growing evidence implicates cytoskeletal disruption in the pathology of age-related neurodegenerative diseases [90]. The validation of cytoskeletal-associated biomarkers offers a promising avenue for patient stratification.
Cytoskeletal Defects as a Therapeutic Gateway
In neurodegenerative diseases, the cytoskeleton's integrity is compromised. In Alzheimer's disease (AD), for instance, microtubule defects in axons cause defective axonal transport, and memory loss could be attributed to microtubule depolymerization [90]. This makes genes and proteins associated with the cytoskeleton prime candidates for biomarker development. An integrative approach combining machine learning models and differential expression analysis has been employed to investigate the transcriptional dysregulation of cytoskeleton-associated genes in pathologies like AD [90]. Using the Recursive Feature Elimination (RFE) technique with a Support Vector Machine (SVM) classifier, which has demonstrated high accuracy in classifying disease states based on gene expression data, researchers can identify a small subset of informative cytoskeletal genes [90].
Key Cytoskeletal Biomarkers and Analytical Approaches
Table 3: Experimentally Identified Cytoskeletal Biomarkers in Age-Related Diseases
| Disease | Identified Cytoskeletal Genes | Proposed Function/Association | Validation Method |
|---|---|---|---|
| Alzheimer's Disease (AD) | ENC1, NEFM, ITPKB, PCP4, CALB1 [90] | Neuronal elasticity, intermediate filaments, signaling [90]. | SVM-based classification; differential expression analysis on transcriptome data (GSE5281) [90]. |
| Hypertrophic Cardiomyopathy (HCM) | ARPC3, CDC42EP4, LRRC49, MYH6 [90] | Actin polymerization, cytoskeletal regulation, myosin heavy chain [90]. | SVM-based classification; differential expression analysis on transcriptome data (GSE32453, GSE36961) [90]. |
| Coronary Artery Disease (CAD) | CSNK1A1, AKAP5, TOPORS, ACTBL2, FNTA [90] | Kinase activity, A-kinase anchoring, prenylation [90]. | SVM-based classification; differential expression analysis on transcriptome data (GSE113079) [90]. |
| Idiopathic Dilated Cardiomyopathy (IDCM) | MNS1, MYOT [90] | Cytoskeletal structure in sarcomere [90]. | SVM-based classification; differential expression analysis on transcriptome data (GSE57338) [90]. |
| Type 2 Diabetes (T2DM) | ALDOB [90] | Altered expression of cytoskeletal structure proteins [90]. | SVM-based classification; differential expression analysis on transcriptome data (GSE164416) [90]. |
Pathway of Cytoskeletal Dysfunction in Neurodegeneration
The following diagram illustrates the hypothesized pathway from cytoskeletal gene dysregulation to neuronal dysfunction, a core mechanism in neurodegenerative diseases.
The Scientist's Toolkit: Research Reagent Solutions
The validation of biomarkers, particularly those related to the cytoskeleton in neurodegeneration, requires a specific set of high-quality research tools. The following table details essential reagents and their functions.
Table 4: Essential Research Reagents for Cytoskeletal Biomarker Validation
| Reagent / Material | Function | Example Application |
|---|---|---|
| Validated Antibodies | Specific detection and quantification of target proteins via IHC and ELISA [89]. | Detecting phosphorylated tau (p-tau) or total alpha-synuclein (t-α-syn) in CSF or tissue sections [91]. |
| Single-Cell RNA Sequencing Kits | Profiling gene expression at single-cell resolution to uncover cellular heterogeneity [92]. | Identifying distinct neuronal and glial subpopulations with cytoskeletal gene dysregulation [90]. |
| SERS Nanoprobes | Ultra-sensitive detection of multiple biomarkers in complex biological samples [89]. | Distinguishing between different protein aggregates in cerebrospinal fluid [89]. |
| Multiplex Immunofluorescence Panels | Simultaneous detection of multiple protein biomarkers on a single tissue section, preserving spatial context [92]. | Co-staining for cytoskeletal markers (e.g., neurofilaments) and immune cell markers in the brain tissue [92]. |
| Patient-Derived Organoids (PDOs) | Three-dimensional models that recapitulate human tumor biology and complex tissue architecture [92]. | Studying cytoskeletal dynamics, tumor heterogeneity, and therapeutic response in a physiologically relevant model [92]. |
| cfDNA Extraction Kits | Isolation of cell-free DNA from blood plasma for liquid biopsy applications [89]. | Monitoring tumor dynamics and treatment response non-invasively [89]. |
The rigorous validation of biomarkers is the cornerstone of precision medicine, enabling effective patient stratification and precise monitoring of treatment response. This process requires a multi-faceted approach, leveraging established techniques like IHC and ELISA alongside cutting-edge technologies such as multi-omics integration, spatial biology, and sensitive biosensors. Within neurodegeneration research, the focus on cytoskeletal defects opens a new frontier for biomarker discovery, as evidenced by computational models identifying key cytoskeletal genes associated with disease. By adhering to robust experimental protocols and utilizing the appropriate research toolkit, scientists and drug developers can translate biomarker candidates into validated tools that ultimately improve patient outcomes.
The therapeutic targeting of the cytoskeleton in neurodegenerative diseases represents a paradigm shift from traditional mono-target approaches. The cytoskeleton, comprising microtubules, actin filaments, and neurofilaments, provides critical structural and functional support for neuronal health. Its collapse is a hallmark of conditions like Alzheimer's disease (AD) and frontotemporal lobar degeneration (FTLD) [3] [24]. This whitepaper delineates the rationale and methodologies for developing combination therapies that integrate cytoskeletal stabilization with modulation of complementary pathways, including proteostasis, neuroinflammation, and growth factor signaling. Such multi-target strategies are essential to address the multifactorial pathology and heterogeneous nature of neurodegenerative diseases, offering a promising avenue for effective disease modification [31].
The neuronal cytoskeleton is a dynamic, interconnected network crucial for maintaining axonal integrity, facilitating intracellular transport, and supporting synaptic plasticity. In neurodegenerative diseases, this network undergoes profound failure. Microtubule destabilization, caused by the loss of functional tau protein, disrupts the essential transport of organelles and proteins, leading to a "dying-back" pattern of neurodegeneration [3] [24]. Concurrently, actin cytoskeleton remodeling impairs dendritic spine stability, directly contributing to early synaptic loss and cognitive decline [24]. Furthermore, aggregation of cytoskeletal proteins like tau and neurofilaments is a common pathological feature, and mutations in genes encoding cytoskeletal proteins (e.g., MAPT, PFN1) or motor proteins (e.g., KIF5A) are directly implicated in disease pathogenesis [3]. This collapse creates a vicious cycle, where initial cytoskeletal disruption promotes further pathology, necessitating therapeutic interventions that simultaneously stabilize the cytoskeleton and target these downstream consequences [31] [24].
Strategic Integration of Therapeutic Pathways
Combination therapies must be designed to act on multiple, synergistic mechanisms. The following table summarizes the core pathological loops and corresponding therapeutic intervention points.
Table 1: Key Pathways for Combination Therapy in Neurodegeneration
| Pathological Loop | Therapeutic Intervention | Molecular Targets | Expected Outcome |
|---|---|---|---|
| Tau-Microtubule Instability [24] | 1. Microtubule Stabilization2. Tau Pathology Reduction | Tubulin, HDAC6, MAPT | Restored axonal transport, reduced tau aggregation |
| Actin-Cofilin Synaptic Deficit [24] | 1. Actin Polymerization Modulation2. Cofilin Inactivation | Rho GTPases, LIMK1, Cofilin | Improved dendritic spine density and synaptic function |
| Proteostasis Failure [31] | 1. Cytoskeletal Stabilization2. Protein Aggregation Clearance | Proteostasis Network (e.g., HSPs, Ubiquitin-Proteasome System) | Reduced pathological protein aggregates (e.g., Tau, Aβ) |
| Neuroinflammation [31] [24] | 1. Cytoskeletal Stabilization2. Glial Cell Modulation | GFAP, Inflammatory Cytokines | Attenuated neuroinflammation and synaptic toxicity |
| Growth Factor Signaling Dysregulation [31] | 1. Cytoskeletal Stabilization2. Growth Factor Potentiation | Neuregulins, ERBB Receptors | Enhanced neuronal survival and network function |
Tau Pathology and Microtubule Stabilization
The dissociation of hyperphosphorylated tau from microtubules is a central event in AD and other tauopathies. A combination approach would pair microtubule-stabilizing agents (e.g., compounds that mimic the function of paclitaxel but are optimized for neuronal use) with kinase inhibitors that reduce pathogenic tau phosphorylation (e.g., GSK-3β inhibitors). This dual strategy not only prevents the initial collapse of the transport network but also directly reduces the pool of toxic, unbound tau, thereby disrupting its prion-like propagation [24].
Actin Dynamics and Synaptic Integrity
At the synapse, the actin cytoskeleton is critical for spine morphology. Pathological tau disrupts actin polymerization, leading to spine loss. Targeting this requires a precise balance: promoting actin polymerization while preventing excessive stabilization. Combining Rho GTPase modulators (to activate profilin and promote actin assembly) with LIMK1 inhibitors (to prevent excessive inactivation of the actin-severing protein cofilin) can restore physiological actin dynamics and protect synaptic structure [24].
Cross-Talk with Proteostasis and Inflammation
Cytoskeletal failure impairs the transport of organelles and proteins, exacerbating proteostasis failure and neuroinflammation. A powerful combination would integrate a cytoskeletal stabilizer with a proteostasis network enhancer (e.g., a drug that boosts chaperone function) and an anti-inflammatory agent targeting glial cells. This triple-therapy approach supports the clearance of aggregated proteins like tau and Aβ while creating a less toxic cerebral environment [31].
Experimental Protocols for Validation
Rigorous in vitro and in vivo models are required to validate the efficacy of combination therapies. The following workflow and detailed protocols provide a framework for preclinical assessment.
Protocol 1: Evaluating Synaptic Rescue in Primary Neurons
This protocol assesses a combination therapy's ability to protect synapses against tau-induced toxicity.
- Primary Cell Culture: Establish cortical or hippocampal neuronal cultures from E18-E19 rodent pups or human induced pluripotent stem cells (hiPSCs). Maintain cultures in Neurobasal medium supplemented with B-27 and GlutaMAX for 14-21 days in vitro (DIV) to allow mature synapse formation [24].
- Pathological Induction & Treatment: At DIV 14, treat cultures with pre-formed fibrils of pathological tau (50-100 nM) to induce endogenous tau aggregation. Concurrently, administer the following: i) Vehicle control, ii) Microtubule-stabilizer (e.g., 10 nM EpoD), iii) LIMK1 inhibitor (e.g., 1 µM), and iv) Their combination [24].
- High-Content Imaging and Analysis: At DIV 21, fix and immunostain neurons for pre-synaptic (e.g., Synapsin I) and post-synaptic (e.g., PSD-95) markers, along with dendritic markers (e.g., MAP2). Image using high-resolution confocal or super-resolution microscopy. Quantify spine density, synaptic puncta density, and co-localization coefficients using automated image analysis software (e.g., ImageJ, Imaris) [24].
Protocol 2: Assessing Efficacy in a Tauopathy Mouse Model
This in vivo protocol evaluates the functional and pathological outcomes of combination therapy.
- Animal Model: Utilize a tauopathy model such as the PS19 mouse (expressing human P301S mutant tau). Randomize animals into four groups (n=12-15/group): i) Wild-type control, ii) PS19 + Vehicle, iii) PS19 + Monotherapy, iv) PS19 + Combination therapy. Begin treatment at 3 months of age, prior to significant pathology [24].
- Drug Administration & Behavioral Testing: Administer compounds via oral gavage or Alzet osmotic minipumps for 3 months. Conduct behavioral assessments monthly:
- Morris Water Maze: Evaluate spatial learning and memory. Record escape latency, path length, and time spent in the target quadrant during the probe trial.
- Y-Maze: Assess spontaneous alternation behavior as a measure of working memory.
- Tissue Collection and Multi-Omics Analysis: Perfuse mice at 6 months of age. Collect brains and hemisect. Process one hemisphere for histology (paraffin or frozen sections). Perform immunohistochemistry for phospho-tau (e.g., AT8 antibody), glial fibrillary acidic protein (GFAP) for astrocytes, and synaptic markers. Quantify tau burden, astrocytosis, and synaptic density in hippocampal and cortical regions. Process the other hemisphere for biochemical analysis, including synaptosome preparation for proteomics and western blotting for cytoskeletal and synaptic proteins [24].
The Scientist's Toolkit: Research Reagent Solutions
Successful research in this field relies on a suite of specialized reagents and tools.
Table 2: Essential Research Reagents for Cytoskeletal Combination Therapy Research
| Reagent / Tool | Function / Target | Example Product/Catalog # | Application Notes |
|---|---|---|---|
| EpoD (Epothilone D) | Microtubule Stabilizer | Sigma-Aldrich, #E3156 | Low nM concentrations; improves axonal transport in models; monitor for peripheral neuropathy in vivo. [24] |
| LIMK1 Inhibitor | Actin Dynamics Modulator | e.g., BMS-5 | Targets LIMK1/2 kinase activity; used to modulate cofilin phosphorylation and actin polymerization status. [24] |
| Pre-formed Tau Fibrils | Pathology Inducer | Recombinantly expressed & sonicated | Seed endogenous tau aggregation in primary neurons and in vivo models; concentration must be titrated. [24] |
| Phospho-Tau Antibodies | Pathology Readout | AT8 (Thermo Fisher, #MN1020) | IHC/ICC for detecting hyperphosphorylated tau (Ser202/Thr205); key for assessing therapeutic efficacy. [24] |
| PSD-95 Antibodies | Synaptic Readout | Cell Signaling Tech, #3450 | Post-synaptic marker for quantifying synaptic density via immunocytochemistry and synaptosome analysis. [24] |
| Live-Cell Actin Probe | Dynamics Visualization | SiR-Actin (Cytoskeleton, Inc.) | Far-red fluorescent probe for real-time, low-perturbation imaging of actin dynamics in live neurons. [93] |
| hiPSC-derived Neurons | Human Model | Commercial vendors (e.g., Fujifilm) | Provide a human-genetic background for screening; can be generated from patient fibroblasts for disease modeling. [31] |
The integration of cytoskeletal-targeting agents with drugs that modulate intersecting pathways represents a transformative approach for treating neurodegenerative diseases. Moving forward, the field must prioritize the development of brain-penetrant, neuron-specific cytoskeletal modulators with improved safety profiles. Furthermore, leveraging single-cell and spatial transcriptomics from animal models and human post-mortem tissue will uncover novel network-level interactions for therapeutic exploitation [31]. The application of machine learning to high-content screening data will be crucial for identifying optimal drug combinations and personalizing treatment strategies for a heterogeneous patient population. By systematically targeting the foundational architecture of the neuron alongside its downstream pathological consequences, combination therapies offer a robust and promising path toward effective disease modification.
Biomarker Validation and Comparative Analysis Across Neurodegenerative Diseases
Neurofilament Light Chain (NfL) has emerged as a pivotal fluid biomarker for quantifying neuroaxonal injury across diverse neurological conditions. As a structural component of the neuronal cytoskeleton, NfL is released into biofluids following axonal damage, providing a sensitive, though non-specific, measure of disease activity and progression. This technical review synthesizes current evidence on the performance of blood-based NfL measurement in Alzheimer's disease (AD), amyotrophic lateral sclerosis (ALS), multiple sclerosis (MS), and cerebral ischemia. We examine analytical platforms, clinical correlations, and methodological considerations for implementing NfL in research and clinical trials. Within the broader context of cytoskeletal defects in neurodegenerative mechanisms, NfL represents a dynamic indicator of active neuronal injury, offering significant utility for diagnostic stratification, prognostic assessment, and therapeutic monitoring.
The neuronal cytoskeleton, a complex network of intermediate filaments, microtubules, and microfilaments, is essential for maintaining structural integrity, facilitating intracellular transport, and supporting synaptic function. Neurofilaments, as class IV neuronal intermediate filaments, are critical structural components particularly abundant in large, myelinated axons. The neurofilament triplet consists of light (NfL, ~68 kDa), medium (NfM, ~145-160 kDa), and heavy (NfH, ~200-220 kDa) chains, with NfL forming the core polymer backbone [94] [95]. Under physiological conditions, neurofilaments exhibit high stability and slow turnover; however, in pathological states, calpain-dependent proteolysis of the cytoskeleton leads to NfL release into extracellular spaces [42].
The significance of NfL extends beyond passive leakage from damaged neurons. Recent evidence indicates that released NfL fragments may actively participate in neuroinflammatory pathways by activating microglial cells, potentially exacerbating neurodegenerative processes [42]. This dual role as both indicator and potential effector in the neurodegenerative cascade positions NfL at the nexus of cytoskeletal pathology and neuroinflammation.
Advances in ultrasensitive immunoassay technologies have enabled reliable quantification of NfL in blood, establishing serum and plasma NfL as accessible biomarkers strongly correlated with cerebrospinal fluid (CSF) concentrations [39] [94]. This correlation has facilitated the non-invasive monitoring of neuroaxonal injury across a spectrum of neurological disorders, revolutionizing biomarker applications in both research and clinical settings.
Analytical Methods for NfL Quantification
The evolution of immunoassay platforms has been instrumental in enabling precise NfL measurement in blood, where concentrations are approximately 40-fold lower than in CSF [94]. Current technologies offer varying levels of sensitivity, precision, and throughput suitable for different research and clinical applications.
Immunoassay Platforms
Table 1: Comparison of Major NfL Immunoassay Platforms
| Manufacturer | Technology Platform | Assay Type | Limit of Detection (pg/mL) | Analytical Measuring Range (pg/mL) | Precision (%CV) |
|---|---|---|---|---|---|
| Quanterix | Simoa HD-X Analyzer | Digital ELISA | 0.085 | 0.345-1140 | Intra-assay: <4.63%, Inter-assay: <8.46% |
| Fujirebio Diagnostics | Lumipulse G1200 | Chemiluminescent Immunoassay (CLIA) | 3.0 | 2.0-5000 | Intra-assay: <3.25%, Inter-assay: <5.50% |
| Roche Diagnostics | Cobas 8000 e 801 | Electrochemiluminescence Immunoassay (ECLIA) | 0.140 | 0.168-1000 | Intra-assay: <5.2%, Inter-assay: <7.2% |
| Siemens Healthcare Diagnostics | Atellica IM Analyzer | Chemiluminescent Immunoassay (CLIA) | 1.3 | 2.5-3000 | Intra-assay: <6.4%, Inter-assay: <12.4% |
| SPEAR Bio | UltraDetect Nf-L | Homogeneous Immunoassay | 0.024 | 0.500 - Not specified | Intra-plate: 3.2%, Inter-plate: 5.4% |
A 2025 method comparison study evaluating five NfL immunoassays (Fujirebio, ProteinSimple, Quanterix, Roche, and Siemens) demonstrated that four of the five assays exhibited exemplary performance in precision and parallelism analyses [96]. While all platforms reliably distinguished healthy controls from individuals with ALS, significant absolute concentration differences were observed across platforms, with plasma NfL concentrations lowest for the Roche assay and highest for the ProteinSimple assay [96]. This underscores the critical importance of method-specific reference ranges and consistency in longitudinal studies.
Methodological Considerations
Pre-analytical factors affecting NfL measurement include:
- Sample Type: NfL concentrations are strongly correlated between EDTA plasma and serum, though plasma levels are approximately 20% lower [40].
- Stability: NfL demonstrates good stability across multiple freeze-thaw cycles and prolonged exposure to room temperature [40].
- Biological Variation: Intra-individual variation of NfL levels in healthy individuals is minimal (mean CV ~7.4%), with no evidence of diurnal rhythmicity, supporting its reliability for longitudinal monitoring [40].
NfL Performance Across Neurological Conditions
Table 2: NfL Performance Characteristics Across Neurological Disorders
| Condition | NfL Elevation vs Controls | Key Diagnostic Utility | Prognostic Correlations | Therapeutic Monitoring Evidence |
|---|---|---|---|---|
| Alzheimer's Disease (AD) | Moderate increase (2.5-15x in CSF) [95] | Limited specificity for AD; best as screening tool to identify candidates for specific biomarker testing [94] | Correlates with rate of cognitive decline and conversion from MCI to dementia [94] | Detects treatment effects in clinical trials; reflects disease-modifying potential [94] |
| Amyotrophic Lateral Sclerosis (ALS) | Marked increase (up to 7x in CSF) [94] | Limited diagnostic value alone; helps distinguish ALS from mimics [97] | Strong correlation with disease progression rate; highly stable longitudinally in individuals [97] | Robust pharmacodynamic biomarker; response to tofersen preceded clinical improvement [97] |
| Multiple Sclerosis (MS) | Variable, dependent on disease activity [97] | No diagnostic specificity; reflects recent disease activity (past 6 weeks) [97] | Predictive of long-term (10-year) disability and atrophy, especially during relapses [97] | Reduction with effective disease-modifying therapies; routine monitoring in specialized clinics [97] |
| Cerebral Ischemia (Stroke) | Acute increase post-event [97] | No role in acute diagnosis; outperforms CT in predicting long-term outcome after cardiac arrest [97] | Levels at 24 hours post-cardiac arrest strongly predict long-term functional outcome [97] | Limited evidence for guiding acute management; potential for outcome prediction |
Alzheimer's Disease
In Alzheimer's disease, NfL elevation reflects the progressive axonal degeneration that accompanies tau-mediated neurofibrillary pathology. While both CSF and plasma NfL are elevated in AD dementia and mild cognitive impairment (MCI) due to AD, the discriminatory accuracy between AD and other neurodegenerative dementias is limited, reflecting the non-specific nature of NfL as a marker of general neuroaxonal injury [94]. Notably, in familial AD, NfL elevations are detectable in mutation carriers as early as 16 years before expected symptom onset, with acceleration in the rate of change approaching clinical manifestation [94].
The association between NfL levels and grey matter atrophy is well-established in AD, though interesting temporal dynamics have been observed: in a study of 567 individuals, CSF NfL levels continued to increase after symptom onset while plasma NfL stabilized, suggesting potential differences in compartmental dynamics as disease progresses [39].
Amyotrophic Lateral Sclerosis
ALS demonstrates some of the most pronounced NfL elevations among neurodegenerative conditions, reflecting the extensive degeneration of motor neurons with large-caliber myelinated axons [94]. The diagnostic utility of NfL in ALS is moderate, primarily helping to distinguish ALS from mimic conditions, though it lacks sufficient specificity for standalone diagnosis [97]. Prognostically, blood NfL levels show strong correlation with progression rate as measured by the ALS Functional Rating Scale, with remarkable longitudinal stability within individuals, mirroring the generally consistent rate of progression observed clinically [97].
The most significant application of NfL in ALS lies in therapeutic development. In the pivotal trial of tofersen for SOD1-related ALS, NfL reduction occurred months before clinical improvement was detectable, leading the FDA to designate it as a "reasonably likely surrogate marker of clinical benefit" [97]. Furthermore, the ATLAS trial pioneered NfL-driven enrollment, randomizing presymptomatic SOD1 mutation carriers to receive tofersen or placebo when NfL levels exceeded a predetermined threshold, representing a paradigm shift in preventive neurology [97].
Multiple Sclerosis
In multiple sclerosis, NfL levels dynamically reflect acute inflammatory activity and associated axonal damage. While lacking diagnostic specificity, NfL measurement provides valuable insights into disease activity independent of clinical relapses, capturing subclinical neuroaxonal injury [97]. The temporal association between inflammatory lesions and NfL elevation is well-characterized, with sharp increases corresponding to lesions developed within the preceding six weeks [97].
The responsiveness of NfL to disease-modifying therapies has established it as a routine monitoring parameter in specialized MS clinics, where reduction in NfL levels within 6-12 months of treatment initiation indicates therapeutic efficacy [97]. This application positions NfL as a valuable pharmacodynamic biomarker for evaluating treatment response in both clinical practice and trial settings.
Cerebral Ischemia
Following acute cerebral ischemia, NfL levels rise in proportion to the extent of neuroaxonal injury. While NfL measurement currently has no role in the acute diagnostic evaluation of stroke, it demonstrates significant prognostic value, particularly after hypoxic-ischemic brain injury following cardiac arrest [97]. NfL levels measured as early as 24 hours post-event outperform clinical measures and CT imaging in predicting long-term functional outcomes [97].
The application of NfL in traumatic brain injury shares similar characteristics, with levels correlating with injury severity and functional outcomes. The return of NfL to normal levels during recovery may provide objective evidence of neurological stabilization, offering clinical utility in managing post-concussive syndromes [97].
Experimental Protocols for NfL Measurement
Plasma NfL Measurement Using SIMOA Technology
Principle: Single Molecule Array (SIMOA) technology employs antibody-coated paramagnetic beads and enzyme-labeled detection antibodies confined within femtoliter-sized wells, enabling digital counting of single immunocomplexes for ultra-sensitive protein detection [39].
Reagents and Materials:
- EDTA plasma samples (avoid repeated freeze-thaw cycles)
- NF-Light Advantage Kit or similar commercial assay kit
- Simoa HD-X Analyzer
- Diluent buffer
- Wash buffers
- Streptavidin-β-galactosidase
- Resorufin-β-D-galactopyranoside substrate
Procedure:
- Sample Preparation: Centrifuge blood samples at 1500-2000×g for 10 minutes within 2 hours of collection. Aliquot plasma and store at -80°C if not analyzed immediately.
- Dilution: Dilute plasma samples 1:4 using appropriate diluent buffer.
- Assay Setup: Combine 100μL of diluted sample with anti-NfL antibody-coated beads. Incubate with shaking for 30 minutes at room temperature.
- Washing: Wash beads twice with wash buffer to remove unbound proteins.
- Detection Antibody Incubation: Add biotinylated detection antibody and incubate with shaking for 30 minutes.
- Enzyme Conjugation: Wash beads, then add streptavidin-β-galactosidase solution. Incubate for 10 minutes.
- Final Wash: Wash beads to remove unbound enzyme.
- Substrate Incubation: Resuspend beads in resorufin-β-D-galactopyranoside substrate solution and load onto Simoa disc.
- Measurement: Analyze on Simoa HD-X instrument, which isolates beads in femtoliter wells, images fluorescence, and calculates concentrations from standard curves.
- Quality Control: Include calibrators and controls in each run. Accept intra-assay CV <10%.
Correlation with Neuroimaging Parameters
Objective: To validate plasma NfL against structural MRI measures of neurodegeneration in AD research.
Protocol:
- Participant Recruitment: Recruit cohort including healthy controls, MCI, and AD dementia participants.
- Sample Collection: Collect plasma samples within 24 hours of MRI acquisition.
- NfL Measurement: Quantify plasma NfL using established immunoassay as described above.
- MRI Acquisition: Obtain 3T MRI including T1-weighted (MPRAGE) for volumetry and T2-FLAIR for white matter hyperintensity assessment.
- Image Analysis:
- Perform automated segmentation of grey matter regions (hippocampus, entorhinal cortex)
- Calculate white matter hyperintensity volumes using lesion segmentation algorithms
- Assess global and regional cortical thickness
- Statistical Analysis:
- Compute Pearson correlations between plasma NfL and imaging metrics
- Perform multiple regression adjusting for age, sex, and clinical diagnosis
- Conduct receiver operating characteristic analysis for disease discrimination
Pathophysiological Framework: NfL in Cytoskeletal Defects
The release of NfL represents a final common pathway of neuroaxonal injury across diverse neurological conditions, reflecting underlying cytoskeletal disintegration. The following diagram illustrates the molecular mechanisms of NfL release and its pathophysiological consequences:
Figure 1: Pathophysiological Mechanism of NfL Release in Neurodegeneration
Beyond its role as a biomarker, emerging evidence suggests that released NfL fragments may actively contribute to neuroinflammatory cascades. Experimental studies demonstrate that NfL application induces transcriptional changes in microglia, while NfL knockout models exhibit reduced microgliosis and delayed symptom onset in SOD1-ALS mice [42]. This suggests a potential feed-forward loop wherein cytoskeletal disintegration actively drives neuroinflammation, amplifying the neurodegenerative process.
The compartmentalization shift of NfL from intracellular structural component to extracellular biofluid marker represents a fundamental process in neurodegenerative diseases. In conditions like AD, this coincides with downregulation of synaptic proteins such as synapsin-2, reflecting comprehensive disruption of neuronal architecture and function [95].
Research Reagent Solutions
Table 3: Essential Research Tools for NfL Investigations
| Reagent/Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Immunoassay Platforms | Quanterix Simoa NF-Light Advantage, Fujirebio Lumipulse, Roche Elecsys, SPEAR UltraDetect Nf-L | NfL quantification in biofluids | Platform selection depends on sensitivity requirements, throughput, and cost; results not directly interchangeable |
| Antibody Reagents | Monoclonal antibodies (clones 2.1, 47.3), anti-NfL biotinylated detection antibodies | Assay development, immunohistochemistry, Western blot | Epitope accessibility varies between intact filaments and cleavage products |
| Sample Matrices | EDTA plasma, serum, cerebrospinal fluid | Biomarker measurement | Plasma preferred over serum (20% lower levels); strong correlation between matrices |
| Reference Materials | Recombinant NfL protein, pooled control samples | Assay calibration, quality control | Enables standardization across laboratories and studies |
| Specialized Kits | SPEAR UltraDetect Nf-L (1μL sample volume, LOD: 0.024 pg/mL) | High-sensitivity applications, limited sample volumes | Homogeneous, wash-free format with low CV% (3.2% intra-assay) |
Integrated Workflow for NfL Research
The following diagram outlines a comprehensive research workflow for investigating NfL in neurodegenerative disease mechanisms:
Figure 2: Comprehensive Research Workflow for NfL Investigations
Neurofilament Light Chain has established itself as a robust, though non-specific, biomarker of neuroaxonal injury across Alzheimer's disease, amyotrophic lateral sclerosis, multiple sclerosis, and cerebral ischemia. Its performance characteristics vary significantly across conditions, reflecting differences in underlying disease dynamics and pathological tempo. In the context of cytoskeletal defects in neurodegeneration, NfL represents both a quantitative measure of structural neuronal integrity and a potential active participant in neuroinflammatory pathways.
Future directions include standardized cut-off values adjusted for age and comorbidities, harmonization of assays across platforms, and validation of NfL as a pharmacodynamic biomarker in therapeutic trials across neurodegenerative conditions. The integration of NfL with other fluid biomarkers and imaging modalities will further enhance its utility in delineating disease-specific patterns of neuroaxonal injury and monitoring therapeutic interventions aimed at preserving neuronal structural integrity.
The neuronal cytoskeleton, a complex and dynamic network of microtubules, neurofilaments, and microfilaments, constitutes the fundamental architectural framework that determines neuronal shape, facilitates intracellular transport, and maintains structural integrity. In neurodegenerative diseases (NDDs), cytoskeletal defects emerge as a central pathological hallmark, disrupting these critical functions and driving disease progression [3] [22]. These defects manifest as abnormalities in the cytoskeleton's structural and functional organization, which are intimately associated with impaired axonal transport of essential cargo, including proteins, lipids, and organelles such as mitochondria [3]. This collapse of the internal transport system within highly polarized neurons leads to a 'dying-back' pattern of degeneration, starting at the most distant synaptic terminals [3] [22].
The discovery of mutations in genes encoding core cytoskeletal proteins and their regulators has unequivocally established that cytoskeletal dysfunction is not merely a secondary consequence but a primary pathogenic mechanism sufficient to cause neurodegeneration [22]. This whitepaper provides a comprehensive analysis of the commonalities and distinctions in cytoskeletal pathology across major NDDs, framing these insights within the broader context of neurodegeneration mechanisms research. By integrating recent findings from large-scale consortia and advanced model systems, we aim to provide researchers and drug development professionals with a detailed technical guide to this critical area of investigation.
Molecular Composition and Functional Organization of the Neuronal Cytoskeleton
The neuronal cytoskeleton comprises three principal polymeric structures distinguished by their protein composition and diameter: microtubules (composed of tubulin), intermediate filaments (primarily neurofilaments in neurons), and actin-based microfilaments [3]. These components interact cooperatively to enable neurons to construct, maintain, and modify their complex architecture over a lifetime.
Table 1: Core Components of the Neuronal Cytoskeleton
| Component | Subunit Composition | Primary Functions | Associated Motor Proteins |
|---|---|---|---|
| Microtubules | α/β-Tubulin heterodimers | Structural support, intracellular transport, mitotic spindle | Kinesin (anterograde), Dynein (retrograde) |
| Intermediate Filaments | Neurofilament Triplet (NF-L, NF-M, NF-H), α-Internexin, Peripherin | Determination of axonal caliber, mechanical strength | Not applicable |
| Microfilaments | Actin polymers | Growth cone dynamics, spine morphology, cell motility | Myosin |
| Microtubule-Associated Proteins | Tau, MAP2, MAP4 | Microtubule stabilization, spacing, dynamics modulation | - |
This intricate cytoskeletal network facilitates the organization and transport of intracellular cargoes and mitochondria along neuronal processes, supporting energy homeostasis and synaptic function [3]. The interplay between actin and microtubules is particularly critical in growth cone dynamics and synapse formation, with cytoskeletal-associated proteins such as plakins cross-linking different cytoskeletal elements [3]. Regulatory proteins, including Rho GTPases, LIM domain kinase 1 (LIMK1), and p21-activated kinase 3 (PAK3), coordinate cytoskeletal remodeling in response to developmental cues and synaptic activity [3].
Core Pathogenic Mechanisms in Cytoskeletal Pathology
Protein Aggregation and Filamentous Inclusions
The accumulation of abnormal protein aggregates represents a fundamental pathological feature across multiple NDDs. These proteinaceous inclusions often consist of cytoskeletal components or associated proteins that have undergone aberrant post-translational modifications or proteolytic processing [22].
Tauopathies: A broad spectrum of NDDs, including Alzheimer's disease (AD), frontotemporal dementia with parkinsonism linked to chromosome 17 (FTDP-17), corticobasal degeneration (CBD), and progressive supranuclear palsy (PSP), is characterized by the accumulation of hyperphosphorylated tau protein in neurofibrillary tangles, neuropil threads, and glial inclusions [22]. Mutations in the MAPT gene encoding tau result in abnormal tau phosphorylation, leading to detachment from microtubules, microtubule destabilization, and ultimately, breakdown of the neuronal cytoskeleton [3]. The discovery of MAPT mutations in FTDP-17 provides direct evidence for the importance of altered cytoskeletal function in neurodegenerative diseases [3] [22].
Neurofilament Inclusions: Abnormal aggregates of neurofilament proteins are observed in amyotrophic lateral sclerosis (ALS), Charcot-Marie-Tooth disease (CMT), and neuronal intermediate filament inclusion disease [22]. These aggregates form a liquid crystal gel network that disrupts axonal transport and impairs neuronal function [3]. Mutations in the gene encoding neurofilament light chain (NEFL) cause CMT disease type 2E, with mutant NEFL interfering with neurofilament assembly and transport [3].
Axonal Transport Deficits
The cytoskeleton provides the railway system for axonal transport, the process by which essential cargo is moved between the cell body and synaptic terminals. Defects in this transport system are associated with the onset and progression of many neurodegenerative disorders [3].
Motor Protein Dysfunction: Mutations in genes encoding motor proteins, such as kinesin family member 5A (KIF5A) and dynactin (DCTN1), are linked to ALS and peripheral neuropathies [3]. These mutations disrupt the proper subcellular distribution of vesicles and organelles, affecting energy metabolism and synaptic function [3].
Mitochondrial Transport Defects: The collapse of the cytoskeleton leads to improper subcellular distribution of mitochondria, indirectly affecting energy metabolism and synaptic function [3]. In ALS, mutations in SOD1 selectively interact with neurofilament light chain mRNA and induce cytoskeletal defects that alter axonal transport [3].
Cytoskeletal Signaling Pathways
Several key signaling pathways regulate cytoskeletal dynamics, and their dysregulation contributes to neurodegenerative processes:
LIMK1-Cofilin Pathway: LIM domain kinase 1 (LIMK1) acts downstream of Rac1 and RhoA, phosphorylating and inactivating the actin depolymerization factor ADF/cofilin, thereby controlling actin dynamics [3]. Studies in LIMK1 knockout mice revealed abnormal spine morphology, with dramatically decreased spine head size and thicker spine necks, as well as enhanced hippocampal long-term potentiation [3].
MicroRNA Regulation: MicroRNAs such as miR-132 and miR-134 regulate dendritogenesis, spine formation, and synaptogenesis. miR-134 negatively regulates dendritic spine size by inhibiting LIMK1 translation, while miR-132 modulates neurite outgrowth by targeting p250GAP, a Rac/Rho family GTPase-activating protein that controls actin cytoskeleton dynamics [3].
The following diagram illustrates the core signaling pathways involved in cytoskeletal pathology:
Figure 1: Core signaling pathways in cytoskeletal pathology. Pathological stimuli trigger neuroinflammatory responses and direct molecular disruptions that converge on cytoskeletal defects, ultimately leading to neuronal death.
Disease-Specific Cytoskeletal Pathology
Alzheimer's Disease (AD)
AD is characterized by two primary pathological hallmarks: extracellular amyloid-beta plaques and intracellular neurofibrillary tangles (NFTs) composed of hyperphosphorylated tau protein [22]. The progression of tau pathology correlates more closely with cognitive decline than amyloid pathology, highlighting the central role of cytoskeletal disruption in AD pathogenesis.
In AD, hyperphosphorylated tau detaches from microtubules, leading to microtubule destabilization and loss of structural integrity [3]. This detachment also allows tau to self-aggregate into paired helical filaments and straight filaments that form NFTs. The mislocalization of tau to synaptic compartments and somatodendritic regions further contributes to synaptic dysfunction and impaired axonal transport [22].
Parkinson's Disease (PD) and Lewy Body Dementias
While PD is primarily characterized by the loss of dopaminergic neurons in the substantia nigra and the presence of Lewy bodies containing aggregated α-synuclein, emerging evidence indicates significant cytoskeletal involvement in PD pathogenesis [22]. Lewy bodies also contain neurofilament proteins, suggesting secondary cytoskeletal pathology [22].
Mutations in the NF-M gene have been associated with PD, indicating a potential direct role of neurofilament dysfunction in the disease [22]. Furthermore, alterations in microtubule organization and axonal transport have been observed in PD models, suggesting broader cytoskeletal disruption beyond α-synuclein pathology.
Amyotrophic Lateral Sclerosis (ALS)
ALS involves the progressive degeneration of upper and lower motor neurons, with prominent cytoskeletal abnormalities in both sporadic and familial forms [22] [98]. Mutations in several genes encoding cytoskeletal proteins or regulators have been identified in ALS:
Table 2: Cytoskeletal-Related Genetic Mutations in ALS
| Gene | Protein Function | Effect of Mutation | Reference |
|---|---|---|---|
| NF-H | Neurofilament heavy subunit | Disrupted assembly, protein aggregation | [22] |
| KIF5A | Motor protein | Impaired axonal transport | [3] |
| PFN1 | Actin-binding protein | Ubiquitinated protein aggregates, cytoskeletal defects | [3] |
| TDP-43 | RNA/DNA-binding protein | Cytoskeletal defects, altered RNA metabolism | [3] |
| C9orf72 | Guanine nucleotide exchange factor | Impaired microglial clearance, cytoskeletal defects | [99] |
In ALS, neurofilament aggregates form proximal axonal swellings that impede axonal transport, leading to a dying-back pattern of degeneration [3]. Notably, neurofilament concentrations in biofluids, particularly neurofilament light chain (NfL), have emerged as promising clinical biomarkers for neurodegeneration across various neurological disorders, including ALS [3] [98].
Frontotemporal Dementia (FTD)
FTD encompasses a heterogeneous group of disorders characterized by progressive degeneration of the frontal and temporal lobes. A significant subset of FTD cases, known as FTDP-17, is caused by mutations in the MAPT gene on chromosome 17, establishing tau dysfunction as a primary mechanism in these forms of FTD [22].
MAPT mutations affect tau function through several mechanisms: (1) reducing tau's ability to bind and stabilize microtubules; (2) promoting tau fibrilization; or (3) perturbing tau gene splicing, leading to an imbalance of tau isoforms with distinct microtubule-binding properties [22]. These alterations ultimately lead to the formation of distinct tau filament structures that characterize different FTD subtypes.
Transdiagnostic Commonalities and Distinctions
Despite their clinical and pathological diversity, NDDs share several common features of cytoskeletal pathology while maintaining distinct characteristics:
Transdiagnostic Commonalities
- Impaired Axonal Transport: Defects in the transport of essential cargo, including mitochondria, vesicles, and proteins, represent a common mechanism across AD, PD, ALS, FTD, and other NDDs [3].
- Protein Aggregation: The accumulation of abnormal filamentous proteins, whether tau, neurofilaments, or other cytoskeletal components, is a shared feature of multiple NDDs [22].
- Dying-Back Neurodegeneration: Many NDDs exhibit a pattern of degeneration that begins at synaptic terminals and progresses retrogradely toward the cell body, reflecting impaired axonal transport and trophic support [3].
- Neuroinflammation-Cytoskeleton Crosstalk: Recent evidence highlights bidirectional interactions between neuroinflammatory processes and cytoskeletal integrity. Microglial activation and subsequent release of inflammatory mediators can drive cytoskeletal alterations in neurons, while cytoskeletal defects in glial cells can exacerbate neuroinflammation [100] [99].
Key Distinctions
Table 3: Distinctive Cytoskeletal Features Across Major NDDs
| Disease | Primary Cytoskeletal Aggregates | Characteristic Inclusions | Key Genetic Mutations |
|---|---|---|---|
| Alzheimer's Disease | Hyperphosphorylated tau | Neurofibrillary tangles, neuropil threads | MAPT (risk alleles) |
| Parkinson's Disease | Neurofilaments (in Lewy bodies) | Lewy bodies (α-synuclein primary) | NF-M (rare) |
| ALS | Neurofilament triplet proteins | Axonal spheroids, hyaline inclusions | NF-H, KIF5A, PFN1 |
| FTD | Tau (in tauopathies), TDP-43 | Pick bodies, tau inclusions | MAPT (causative) |
| CMT | Neurofilament light chain | Neurofilament aggregates | NEFL |
Experimental Models and Methodologies
In Vitro and In Vivo Modeling of Cytoskeletal Pathology
Experimental models are essential for elucidating the molecular mechanisms underlying cytoskeletal pathology in NDDs. These include:
Transgenic Animal Models: Genetically engineered mice expressing mutant forms of human tau, neurofilament proteins, or other cytoskeletal components recapitulate key features of human NDDs, including protein aggregation, axonal transport deficits, and progressive neuronal loss [22].
CRISPR-Cell Models: The generation of isogenic cell lines with precise mutations in cytoskeletal genes enables detailed mechanistic studies. For example, CRISPR-generated TAZ knockout cell lines have been used to study mitochondrial trafficking and function [101].
Imaging Cytoskeleton Dynamics
Advanced imaging techniques enable the visualization of cytoskeletal dynamics in live cells and tissues:
Live-Cell Imaging: Recent advances in the visualization of the microtubule and actin cytoskeleton in multicellular organisms allow researchers to monitor cytoskeletal organization and dynamics in real-time [3].
High-Resolution Microscopy: Super-resolution microscopy techniques, such as STORM and STED, reveal the nanoscale organization of cytoskeletal elements and their alterations in disease states.
The following experimental workflow outlines a comprehensive approach to studying cytoskeletal pathology:
Figure 2: Experimental workflow for studying cytoskeletal pathology. A multi-modal approach integrates protein, imaging, genetic, and functional analyses to comprehensively characterize cytoskeletal defects and identify therapeutic targets.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Cytoskeletal Pathology Studies
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Antibodies for Cytoskeletal Proteins | Anti-tau (phospho-specific), anti-neurofilament, anti-α-tubulin | Immunohistochemistry, Western blot, ELISA | Validate phospho-specific antibodies with appropriate controls |
| Live-Cell Probes | SiR-tubulin, LifeAct-GFP, MitoTracker | Live imaging of cytoskeletal dynamics | Optimize concentration to avoid artifacts |
| CRISPR Reagents | gRNAs for MAPT, NEFL, KIF5A | Generation of isogenic cell models | Use dual gRNA approach with dCas9-FokI for reduced off-target effects [101] |
| Proteomic Platforms | SomaScan, Olink, Mass spectrometry | High-dimensional protein biomarker discovery | Platform selection affects isoform detection [10] |
| Animal Models | Tau transgenic mice, Neurofilament mutant mice | In vivo pathogenesis and therapeutic studies | Consider species-specific differences in protein isoforms |
| Biomarker Assays | Neurofilament light chain (NfL) ELISA/SIMOA | Monitoring neurodegeneration in biofluids | Standardization across platforms needed [98] |
Biomarker and Therapeutic Development
Biomarkers for Cytoskeletal Pathology
The development of biomarkers for cytoskeletal pathology has advanced significantly in recent years:
Neurofilament Light Chain (NfL): Elevated levels of NfL in cerebrospinal fluid and blood have emerged as a promising biomarker for axonal damage across multiple NDDs, including ALS, AD, and FTD [98]. NfL levels robustly correlate with disease progression and treatment response in clinical trials.
Tau Species: Various tau fragments and phospho-tau species in biofluids show promise as specific biomarkers for tauopathies. The Global Neurodegeneration Proteomics Consortium (GNPC) has established one of the world's largest harmonized proteomic datasets to facilitate the discovery of such biomarkers [10].
Microglia-Related Biomarkers: Soluble TREM2 (sTREM2) in CSF is considered a biomarker of microglial activation, with elevated levels observed in AD during early symptomatic stages [99]. These biomarkers reflect non-cell-autonomous mechanisms contributing to cytoskeletal pathology.
Therapeutic Strategies Targeting Cytoskeletal Defects
Several therapeutic approaches are being developed to target cytoskeletal pathology in NDDs:
Microtubule-Stabilizing Agents: Drugs that modulate microtubule stability, such as eporhilones and taxanes, have shown beneficial effects in preclinical models of tauopathies by counteracting microtubule loss and improving axonal transport [3].
Inhibitors of Pathological Post-Translational Modifications: Compounds affecting the levels of tubulin acetylation and other post-translational modifications of cytoskeletal components constitute promising therapeutic interventions [3].
Gene-Targeted Therapies: Antisense oligonucleotides (ASOs) targeting mutant genes responsible for cytoskeletal defects, such as MAPT mutations in FTDP-17, are under development [98]. Similarly, ASOs targeting SOD1 and C9orf72 have shown promise in ALS clinical trials [98].
Microglia-Targeted Therapies: Therapeutic strategies targeting microglial function, such as TREM2-activating antibodies (AL002, VHB937) and small-molecule agonists (VG-3927), aim to enhance clearance of protein aggregates and reduce neuroinflammation [99].
The field of cytoskeletal pathology in NDDs is rapidly evolving, with several promising research directions emerging:
Multi-Omic Integration: The integration of proteomic, genomic, transcriptomic, and metabolomic data from large consortia like the GNPC provides unprecedented opportunities to identify novel biomarkers and therapeutic targets [10]. These approaches enable the identification of transdiagnostic proteomic signatures and disease-specific patterns of protein abundance [10].
Single-Cell and Spatial Technologies: Single-cell omics and spatial transcriptomics allow researchers to characterize cell-type-specific cytoskeletal alterations and map their spatial distribution within vulnerable brain regions [99].
Advanced Biomarker Development: Emerging technologies, including extracellular vesicle-based biomarkers and artificial intelligence (AI)-driven integration of multimodal data, offer new opportunities to align biomarker profiles with evolving disease states and improve patient stratification [99].
Personalized Therapeutic Approaches: Building on the model of companion diagnostics in oncology, integrating multimodal biomarker strategies holds promise for guiding personalized interventions across the neurodegenerative spectrum [99].
In conclusion, cytoskeletal defects represent a central pathological hallmark shared across major NDDs, while maintaining disease-specific characteristics. The comprehensive understanding of commonalities and distinctions in cytoskeletal pathology provides a framework for defining pathogenic mechanisms, categorizing different NDDs, stratifying patients, and designing multi-targeted, personalized therapies. As research in this field continues to advance, targeting cytoskeletal pathology holds significant promise for developing effective treatments that can halt or slow the progression of these devastating disorders.
The cytoskeleton, a dynamic network of intracellular filaments, is fundamental to neuronal health, governing cellular shape, integrity, intracellular transport, and synaptic function. A compelling body of evidence positions the breakdown of this critical infrastructure as a central mechanism in the pathogenesis of numerous neurodegenerative diseases [69] [21]. This dysregulation manifests in various forms, including the collapse of transport systems, aberrant actin dynamics, and the formation of pathological aggregates that sequester essential cytoskeletal components. In Alzheimer's disease (AD), for instance, hyperphosphorylated tau protein dissociates from microtubules, leading to cytoskeletal instability and the formation of neurofibrillary tangles [21]. Similarly, in Amyotrophic Lateral Sclerosis (ALS), impairments in axonal transport are linked to defects in motor proteins and their cytoskeletal tracks [21]. The identification of specific cytoskeletal genes associated with age-related diseases through modern computational methods further underscores this connection, highlighting targets such as ARPC3, CDC42EP4, and ENC1 [9]. This whitepaper delineates how transgenic animal models, from fruit flies to large animals, serve as indispensable tools for moving these potential cytoskeletal targets from initial discovery through preclinical validation and into the therapeutic pipeline.
Identifying Cytoskeletal Targets: From Omics to Organisms
The initial discovery of candidate cytoskeletal targets for neurodegenerative diseases has been revolutionized by integrative computational approaches. A recent study employed an integrative machine learning framework to analyze transcriptional changes of cytoskeletal genes across five age-related diseases: Alzheimer's disease (AD), Hypertrophic Cardiomyopathy (HCM), Coronary Artery Disease (CAD), Idiopathic Dilated Cardiomyopathy (IDCM), and Type 2 Diabetes Mellitus (T2DM) [9]. The research utilized Support Vector Machine (SVM) classifiers combined with Recursive Feature Elimination (RFE) to identify a minimal set of cytoskeletal genes capable of accurately discriminating between patient and normal samples [9]. This methodology achieved high accuracy across the diseases studied and pinpointed a concise set of potential biomarkers.
Table 1: Machine Learning-Identified Cytoskeletal Gene Targets for Age-Related Diseases
| Disease | Identified Cytoskeletal Genes | Primary Function | Validation Accuracy |
|---|---|---|---|
| Alzheimer's Disease (AD) | ENC1, NEFM, ITPKB, PCP4, CALB1 [9] | Microtubule organization, neuronal signaling | High (SVM classifier) [9] |
| Hypertrophic Cardiomyopathy (HCM) | ARPC3, CDC42EP4, LRRC49, MYH6 [9] | Actin polymerization, myosin function | High (SVM classifier) [9] |
| Coronary Artery Disease (CAD) | CSNK1A1, AKAP5, TOPORS, ACTBL2, FNTA [9] | Kinase signaling, actin binding, prenylation | High (SVM classifier) [9] |
| Idiopathic Dilated Cardiomyopathy (IDCM) | MNS1, MYOT [9] | Cytoskeletal organization in sarcomere | High (SVM classifier) [9] |
| Type 2 Diabetes (T2DM) | ALDOB [9] | Glycolysis, cytoskeletal interactions | High (SVM classifier) [9] |
Furthermore, cross-disease analysis revealed shared cytoskeletal pathology, with genes like ANXA2 and TPM3 found to be common to multiple conditions, including AD, T2DM, and CAD [9]. This suggests these genes may regulate core cytoskeletal pathways vulnerable in diverse age-related pathologies. The convergence of computational biology with traditional molecular techniques provides a powerful, data-driven starting point for target selection, setting the stage for validation in living organisms.
Experimental Protocols: From Model Generation to Phenotypic Analysis
Establishing Transgenic Models
The creation of transgenic models to probe cytoskeletal function in neurodegeneration relies on several well-established protocols. The general workflow involves gene identification, vector construction, model generation, and multi-level phenotypic validation.
Table 2: Key Transgenic Model Generation Techniques
| Technique | Underlying Principle | Application Example | Considerations |
|---|---|---|---|
| Pronuclear Microinjection | Direct microinjection of DNA constructs into fertilized oocytes [102] [103] | APP transgenic mice for AD [102] | Random integration, variable copy number, insertional mutagenesis risk. |
| Lentiviral Transgenesis | Utilization of lentiviral vectors for gene delivery into oocytes or embryos [104] | HD transgenic monkeys expressing mutant huntingtin [104] | Potentially lower copy number, more stable expression. |
| CRISPR/Cas9 Gene Editing | Precise genome editing using CRISPR/Cas9 system [104] | Large animal models (pigs, monkeys) for ALS, HD [104] | Enables precise gene knock-in/knock-out; requires careful off-target analysis. |
| Somatic Cell Nuclear Transfer (Cloning) | Transfer of genetically modified nucleus into enucleated oocyte [104] | SOD1 G93A transgenic pig model of ALS [104] | Technically challenging, used for large animal model generation. |
A specific example is the generation of a transgenic mouse model for autosomal dominant cataract, which involved subcloning sequences encoding either mutant (R116C) or wild-type human αA-crystallin into a promoter vector containing the mouse αΑ-crystallin promoter [103]. The transgene fragment was then released and microinjected into fertilized B6CBA F1 hybrid embryos. Founders were screened via PCR, and independent lines were established [103].
Phenotypic Characterization and Workflow
Once models are generated, a rigorous multi-stage phenotypic analysis is conducted to validate cytoskeletal dysfunction and its neurological consequences.
Molecular and Cellular Analyses: At the molecular level, the expression of the transgene and its impact on endogenous proteins must be confirmed. This involves techniques such as quantitative Western blot analysis to determine the abundance of transgenic and endogenous proteins in both soluble and insoluble fractions [103]. RT-PCR is used to verify transcriptional activity [103]. Crucially, cytoskeletal integrity is assessed by examining specific pathologies. For example, the formation of cofilin-actin rods, which are induced by oxidative stress and disrupt synaptic transport, can be monitored, though standard probes like Lifeact do not bind these structures, necessitating specialized approaches [69]. The use of specific antibodies for immunohistochemistry allows for the visualization of protein localization and aggregation, such as hyperphosphorylated tau or mutant α-synuclein [103] [21].
Organism-Level Phenotyping: To translate molecular deficits into functional outcomes, a range of behavioral and physiological tests are employed. In Drosophila models, high-throughput screens can assess locomotor function, learning, and memory [105]. In rodent and large animal models, more complex motor coordination tests and cognitive assays (e.g., water maze for spatial memory) are standard [102] [104]. A scoring system for specific morphological defects, such as the lens opacities and posterior sutural defects in αA-crystallin mutant mice, allows for quantitative phenotypic assessment [103].
The Scientist's Toolkit: Essential Research Reagents
The experimental protocols described rely on a curated set of reagents and tools, each serving a distinct function in the validation pipeline.
Table 3: Key Research Reagent Solutions for Cytoskeletal Target Validation
| Reagent/Tool | Category | Primary Function in Research | Example Application |
|---|---|---|---|
| His-Tag Monoclonal Antibody [103] | Immunological Reagent | Detection and quantification of recombinant transgenic proteins in Western blot and IHC. | Detecting His-tagged human αA-crystallin in transgenic mouse lenses [103]. |
| Anti-Cofilin Antibodies [69] | Immunological Reagent | Identification and study of cofilin-actin rods, hallmarks of cytoskeletal stress in neurodegeneration. | Investigating actin dysregulation in AD models [69]. |
| Limma Package (R) [9] | Bioinformatics Tool | Batch effect correction, normalization, and differential expression analysis of transcriptome data. | Identifying dysregulated cytoskeletal genes in age-related diseases [9]. |
| DESeq2 [9] | Bioinformatics Tool | Differential gene expression analysis of RNA-seq data. | Identifying dysregulated cytoskeletal genes in age-related diseases [9]. |
| CRISPR/Cas9 System [104] | Gene Editing Tool | Precise knockout or knock-in of disease-associated genes in zygotes for model generation. | Creating isogenic large animal (pig, monkey) models of ALS and HD [104]. |
| Adeno-Associated Virus (AAV) Vectors [106] | Gene Delivery Vehicle | In vivo delivery of therapeutic transgenes (e.g., neuroprotective factors) or gene-silencing constructs. | Clinical trials for SOD1 ALS; delivering ASOs in animal models [106]. |
| Antisense Oligonucleotides (ASOs) [106] | Therapeutic Modality | Silencing pathogenic genes by targeting their mRNA for degradation. | Intrathecal delivery of Tofersen for SOD1-ALS in clinical trials [106]. |
Pathway to Therapy: Validating Targets and Translating Findings
The ultimate goal of using transgenic models is to translate discoveries into effective therapies. This involves not only validating the pathogenic role of a target but also testing interventions designed to engage it. The journey of cytoskeletal-targeting therapies from bench to bedside follows a critical pathway, from mechanistic insight to clinical application.
A prime example of this pipeline in action is the development of gene therapies for genetic forms of ALS. Transgenic models expressing mutant SOD1 or C9orf72 genes have been instrumental in validating these targets and testing antisense oligonucleotides (ASOs) designed to reduce levels of the toxic proteins [104] [106]. The success of these approaches in animal models has led to clinical trials, such as the phase 1-3 trial of Tofersen, an ASO targeting SOD1 mRNA [106]. This demonstrates a direct route from genetic discovery and target validation in transgenic animals to a potential therapy for patients.
Furthermore, modeling cytoskeletal defects in large animals has proven to be particularly informative for translation. Unlike rodent models, SOD1 G93A transgenic pigs show clear neuronal degeneration and exhibit nuclear accumulation of mutant SOD1 and ubiquitinated nuclear aggregates, a pathology observed in some ALS patients but not in mouse models [104]. Similarly, transgenic monkeys expressing mutant huntingtin develop key clinical features like dystonia and chorea, which are not typically seen in mice, and show early degeneration in neuronal processes [104]. These findings from large animals provide critical pathophysiological insights that bridge the gap between rodent models and human patients, de-risking the therapeutic development process and providing more relevant systems for evaluating biomarker and treatment efficacy.
Transgenic animal models provide an indispensable, multi-stage platform for validating cytoskeletal targets in neurodegenerative diseases. The journey begins with computational biology pinpointing candidate genes, proceeds through rigorous phenotypic characterization in models ranging from flies to primates, and culminates in the testing of targeted therapies. The consistent recapitulation of cytoskeletal pathology—from cofilin-actin rods in AD to axonal transport defects in ALS—across these models confirms the central role of the cytoskeleton in neurodegeneration. As genetic engineering technologies like CRISPR/Cas9 continue to advance, the fidelity of these models will only increase, enabling more accurate prediction of therapeutic outcomes in humans. The continued refinement of this pipeline, bolstered by insights from large animal models, promises to accelerate the development of effective treatments that stabilize the neuronal cytoskeleton and halt the progression of devastating neurological disorders.
Neurodegenerative diseases (NDs), including Alzheimer's disease (AD), Parkinson's disease (PD), Amyotrophic Lateral Sclerosis (ALS), and Huntington's disease (HD), represent a growing global health burden, affecting over 57 million people worldwide [10]. Despite their distinct clinical presentations and primarily affected brain regions, these conditions share remarkable commonalities at the subcellular level, particularly regarding cytoskeletal defects that disrupt neuronal structure, function, and viability [31] [14]. The progressive loss of neuronal structure and connectivity, hallmarks of neurodegeneration, are fundamentally rooted in the dysregulation of the intricate cytoskeletal networks comprising actin filaments, microtubules, and neurofilaments.
The therapeutic landscape for NDs has witnessed both notable successes and perplexing failures. While disease-modifying therapies for genetic forms of ALS and monoclonal antibodies targeting amyloid-β in AD have recently emerged, many clinical trials targeting singular pathological proteins have yielded disappointing results [10] [31]. This whitepaper examines therapeutic efficacy across neurodegenerative diseases through the lens of shared cytoskeletal pathology, arguing that transdiagnostic mechanisms—including aberrant protein aggregation, neuroinflammation, synaptic dysfunction, and cytoskeletal disintegration—represent critical targets for the next generation of interventions. By analyzing patterns of success and failure across clinical trials, we derive strategic insights for researchers and drug development professionals aiming to develop effective treatments for these devastating disorders.
Shared Cytoskeletal Pathology Across Neurodegenerative Diseases
Cytoskeletal Defects as a Convergent Mechanism
The neuronal cytoskeleton is dynamically regulated to maintain structural integrity, facilitate intracellular transport, and support synaptic plasticity. Across major neurodegenerative conditions, this precise regulation is disrupted, leading to characteristic pathological features.
Actin cytoskeleton dysregulation manifests through the formation of specific pathological aggregates. Cofilin-actin rods, which form under oxidative and energetic stress conditions such as ATP depletion, are increasingly recognized as a feature common to AD, PD, and HD [14]. These rod-like structures sequester actin and cofilin, leading to synaptic loss by eliminating excitatory synapses. Recent research has identified that specific mutations at the actin-ATP interface (K18A, D154A, G158L, K213A) promote the formation of these disease-associated actin-rich structures, including cofilin-actin rods and Hirano bodies, without causing immediate apoptotic cell death [14]. This suggests a direct mechanistic link between actin nucleotide binding and the development of persistent pathological aggregates that disrupt neuronal function.
Microtubule-associated pathology is prominently exemplified by tau protein abnormalities in tauopathies, including Alzheimer's disease. The microtubule-associated protein tau undergoes pathological hyperphosphorylation, leading to its dissociation from microtubules and subsequent aggregation into neurofibrillary tangles. This process destabilizes microtubules, impairing axonal transport and ultimately compromising neuronal connectivity and function [107]. The central role of cytoskeletal disruption across neurodegenerative diseases underscores its potential as a therapeutic target for conditions including Alzheimer's disease, Parkinson's disease, and Amyotrophic Lateral Sclerosis [14].
Table 1: Key Cytoskeletal Pathologies Across Neurodegenerative Diseases
| Disease | Primary Cytoskeletal Pathologies | Key Proteins Involved | Functional Consequences |
|---|---|---|---|
| Alzheimer's Disease | Neurofibrillary tangles, cofilin-actin rods, Hirano bodies | Tau, actin, cofilin | Microtubule destabilization, synaptic loss, impaired transport |
| Parkinson's Disease | Lewy bodies, cofilin-actin rods, actin inclusions | α-synuclein, tau, actin | Neuritic degeneration, synaptic dysfunction |
| Amyotrophic Lateral Sclerosis | Neurofilament aggregates, cofilin pathology | TDP-43, SOD1, neurofilaments | Axonal transport defects, motor neuron degeneration |
| Huntington's Disease | Actin-rich inclusions, mutant huntingtin aggregates | Huntingtin, actin | Transcriptional dysregulation, synaptic dysfunction |
Transdiagnostic Proteomic Signatures
Large-scale consortium efforts are revealing shared molecular pathways across neurodegenerative diseases. The Global Neurodegeneration Proteomics Consortium (GNPC), one of the world's largest harmonized proteomic datasets, has identified transdiagnostic proteomic signatures of clinical severity across AD, PD, FTD, and ALS [10]. This comprehensive resource includes approximately 250 million unique protein measurements from more than 35,000 biofluid samples, providing unprecedented power to detect conserved molecular pathways.
Notably, the GNPC has described a robust plasma proteomic signature of APOE ε4 carriership that is reproducible across multiple neurodegenerative conditions, suggesting shared downstream pathological mechanisms related to this major genetic risk factor [10]. Additionally, distinct patterns of organ aging have been observed across these conditions, potentially reflecting systemic manifestations of fundamentally neurodegenerative processes. These findings highlight the existence of common pathological mechanisms operating across traditional diagnostic boundaries and suggest promising targets for therapeutic intervention with potential efficacy in multiple conditions.
Clinical Trial Landscape: Quantitative Analysis of Success and Failure
Stem Cell Therapy Trials
Stem cell therapies represent a promising approach for neurodegenerative diseases due to their potential to repair damaged tissues, replace lost neurons, and modulate neuroinflammation. A systematic evaluation of 94 stem cell clinical trials for AD, PD, ALS, and HD reveals the current state of this therapeutic modality [81].
Table 2: Stem Cell Clinical Trials for Major Neurodegenerative Diseases
| Disease | Total Trials | Phase 3 Trials | Phase 2 Trials | Participants (Estimated) | Predominant Cell Types |
|---|---|---|---|---|---|
| Alzheimer's Disease | ~65% of total | 0 | 2 ongoing | ~5,600 | Mesenchymal stem cells (MSCs), Neural stem cells (NSCs) |
| Parkinson's Disease | Information Missing | 0 | 2 completed, 1 ongoing | Information Missing | NSCs, induced pluripotent stem cells (iPSCs) |
| Amyotrophic Lateral Sclerosis | Information Missing | 1 completed, 1 ongoing | 2 completed, 2 ongoing | Information Missing | MSCs, NSCs |
| Huntington's Disease | Information Missing | 1 ongoing | 1 completed | Information Missing | MSCs |
Most trials remain in early developmental phases, with only three Phase 3 studies conducted across all four diseases (one completed and one ongoing in ALS, and one ongoing in HD) [81]. The limited progression to late-stage trials reflects both the technical challenges of stem cell therapies and potentially inadequate patient stratification strategies. Delivery methods have included intravenous or intrathecal injection and direct transplantation into the brain, with varying degrees of success reported across conditions.
A significant challenge in stem cell therapies is the risk of tumorigenesis, particularly with pluripotent stem cells, alongside limitations in cell survival and integration into host tissue [81]. These hurdles have prompted the exploration of alternative approaches, including stem cell-derived exosomes, which offer several advantages including reduced risk of immunological rejection and tumorigenesis, easier traversal of the blood-brain barrier, and greater practicality for clinical applications [81].
Targeted Molecular Therapies
Targeted approaches, including monoclonal antibodies, gene therapies, and small molecule inhibitors, have yielded both promising successes and notable failures across neurodegenerative conditions:
Immunotherapy trials targeting amyloid-β in Alzheimer's disease exemplify the mixed outcomes in this space. While aducanumab received FDA approval despite ongoing debates about its clinical efficacy, semorinemab (targeting tau) has shown more equivocal results [81]. These variable outcomes highlight the challenges of targeting protein aggregates after significant pathological progression has occurred.
Gene therapy approaches have demonstrated promise particularly in monogenic neurodegenerative disorders. Strategies such as gene silencing to reduce mutant huntingtin protein levels in Huntington's disease represent a potentially disease-modifying approach [81]. Similarly, antisense oligonucleotides (ASOs) have shown efficacy in genetic forms of ALS. However, these approaches face significant delivery challenges, particularly in traversing the blood-brain barrier and ensuring stable expression in target neurons [81] [108].
Small molecule inhibitors targeting specific pathological processes have demonstrated variable success. For example, bosutinib, ropinirole, and ezogabine for ALS, and bromocriptine for familial AD have advanced to clinical trials based on promising preclinical data, often utilizing iPSC models [109]. However, many small molecule programs have failed in late-stage development due to limited efficacy or adverse effects.
The high failure rate of targeted therapies (with only 8% of treatments tested in Phase I trials ultimately reaching the market) underscores the complexity of neurodegenerative diseases and the limitations of single-target approaches in conditions characterized by multifaceted pathology [108].
Experimental Models and Protocols for Cytoskeletal Research
Actin Mutant Phenotyping Protocol
The following detailed methodology enables the investigation of actin nucleotide-binding residues in the formation of anomalous cytoskeletal structures associated with neurodegenerative diseases [14]:
Cell Culture and Transfection:
- Maintain HeLa cells and primary cortical neurons in appropriate culture conditions.
- Transfect cells with Actin.CIB.GFP fusion constructs containing point mutations in the actin-ATP binding site (e.g., K18A, D154A, G158L, S14V, K213A).
- Include Actin.WT.CIB.GFP transfection as a control to establish baseline phenotype.
Optogenetic System Application (CofActor):
- Utilize the CofActor system, consisting of Cry2-Cofilin.S3E-mCherry and betaActin-CIB-GFP fusions.
- Activate the system with 470nm blue light to induce cofilin-actin cluster formation.
- Image cells every 30 seconds post-activation to monitor cluster dynamics.
- Apply energetic stress (ATP depletion) to examine stress-induced phenotype formation.
Phenotypic Characterization:
- Fix cells at appropriate timepoints and process for immunohistochemistry.
- Visualize actin distribution and anomalous structures via widefield microscopy.
- Quantify actin cluster formation using FIJI/ImageJ Analyze Particles feature.
- Assess co-localization with cofilin and other actin-binding proteins.
- Evaluate nuclear integrity to exclude apoptotic cells from analysis.
Data Analysis:
- Compare the distribution of mutant actin constructs to wild-type controls.
- Quantify the prevalence of disease-associated structures (rods, inclusions) under homeostatic and stress conditions.
- Analyze the sequestering effect of mutant actin on endogenous actin in co-transfection experiments.
This protocol has identified that mutations disrupting direct interactions with the phosphate tail of ATP (K18A, D154A, G158L, K213A) are particularly disruptive to normal actin dynamics and promote pathological structures resembling those found in neurodegenerative diseases [14].
High-Dimensional Proteomic Profiling
Large-scale proteomic analysis, as employed by the Global Neurodegeneration Proteomics Consortium, provides a powerful approach to identify shared molecular signatures across neurodegenerative conditions [10]:
Sample Preparation and Platform Integration:
- Collect plasma, serum, and CSF samples from well-characterized patient cohorts.
- Analyze samples using multiple proteomic platforms (SomaScan, Olink, mass spectrometry) to maximize coverage and enable cross-platform validation.
- Process samples according to standardized protocols to minimize technical variability.
Data Harmonization and Analysis:
- Employ the AD Workbench, a secure cloud-based environment, for data aggregation and analysis.
- Perform principal component analysis to evaluate data structure and identify matrix effects (e.g., serum vs. plasma).
- Conduct differential abundance analysis to identify disease-specific protein signatures.
- Implement machine learning approaches to derive transdiagnostic signatures of disease severity.
This approach has enabled the identification of conserved proteomic alterations across neurodegenerative conditions, revealing shared pathways and potential therapeutic targets with relevance to multiple diseases [10].
Visualizing Shared Pathological Pathways and Research Workflows
The following diagrams illustrate key shared pathological pathways and experimental approaches in cytoskeletal neurodegeneration research.
Shared Pathways in Neurodegeneration
Experimental Workflow for Cytoskeletal Research
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Cytoskeletal Neurodegeneration Research
| Reagent/Platform | Function | Application in Neurodegeneration Research |
|---|---|---|
| CofActor Optogenetic System | Light- and stress-gated reporter of cofilin-actin cluster formation | Investigating real-time dynamics of pathological actin structure formation [14] |
| SomaScan Platform (SOMAmer-based) | High-throughput proteomic profiling measuring ~7,000 proteins | Large-scale biomarker discovery and transdiagnostic signature identification [10] |
| Olink Proximity Extension Assay | High-sensitivity proteomic platform | Validation of proteomic findings and inflammatory pathway analysis |
| Tandem Mass Tag Mass Spectrometry | Multiplexed quantitative proteomics | Deep profiling of protein expression and post-translational modifications [10] |
| Induced Pluripotent Stem Cells (iPSCs) | Patient-specific disease modeling | Drug screening and personalized therapeutic development [109] |
| Actin-ATP Interface Mutants (K18A, D154A, etc.) | Specific perturbation of actin nucleotide binding | Investigating molecular mechanisms of actin pathology [14] |
| Mesenchymal Stem Cell-Derived Exosomes | Therapeutic nanovesicles for drug delivery | Crossing BBB to deliver therapeutic molecules with reduced immunogenicity [81] |
| Antisense Oligonucleotides (ASOs) | Gene silencing and splicing modulation | Targeting mutant proteins in monogenic neurodegenerative diseases [108] |
Strategic Framework for Future Clinical Development
Biomarker-Driven Patient Stratification
The failure of many neurodegenerative disease trials stems in part from heterogeneous patient populations and inadequate biomarkers for patient selection and monitoring. Promisingly, fluid biomarkers are increasingly available to address these challenges. Measurement of neurofilament light chain (NfL) in serum provides a sensitive marker of axonal damage that correlates with disease progression across multiple neurodegenerative conditions [108]. Additionally, the GNPC has identified specific plasma proteomic signatures associated with APOE ε4 carriership and clinical severity that are reproducible across AD, PD, FTD, and ALS [10].
Implementing a precision medicine approach that incorporates genotypic, phenotypic, and biomarker data will enable more targeted therapeutic development. This strategy is particularly important for cytoskeletal-directed therapies, as the manifestation of cytoskeletal pathology may vary across individuals despite similar clinical presentations.
Advanced Clinical Trial Designs
Traditional randomized controlled trials have proven inefficient for neurodegenerative drug development, with only approximately 8% of treatments tested in Phase I trials ultimately reaching the market [108]. Innovative trial designs offer promising alternatives:
Multi-arm, multi-stage (MAMS) platform trials enable the simultaneous evaluation of multiple therapeutic candidates against a shared control group, increasing efficiency and reducing costs [108]. Such designs have been successfully implemented in oncology and multiple sclerosis, and could be adapted for neurodegenerative conditions with shared cytoskeletal pathology.
Basket trials represent another efficient design, particularly for targeted therapies. In this approach, patients with different neurodegenerative conditions sharing a specific molecular characteristic (e.g., specific cytoskeletal pathology biomarkers) can be enrolled to test a therapy targeting that shared mechanism [108].
Therapeutic Delivery Innovation
A critical challenge for neurodegenerative disease therapies, particularly biologics and gene therapies, is effective delivery across the blood-brain barrier. Several innovative approaches are in development:
Intrathecal delivery currently represents the most direct route for CNS-targeted therapies but carries limitations including patient discomfort and potential complications [108].
Nanotechnology drug delivery systems show promise for enhancing BBB penetration while minimizing invasiveness. Stem cell-derived exosomes represent a particularly promising delivery vehicle, as they naturally cross the BBB and can be engineered to carry therapeutic cargo [81].
Focused ultrasound techniques that temporarily disrupt the BBB are also under investigation to facilitate therapeutic delivery to target brain regions [108].
The analysis of successful and failed trials across neurodegenerative diseases reveals crucial insights for future therapeutic development. First, targeting shared pathological mechanisms, particularly cytoskeletal defects, offers promise for developing treatments with efficacy across multiple conditions. Second, biomarker-driven patient stratification is essential for identifying individuals most likely to respond to specific mechanism-based therapies. Third, innovative trial designs that improve efficiency and enable precision medicine approaches are critical for accelerating therapeutic development.
The convergence of large-scale molecular datasets (e.g., GNPC), advanced cellular models (e.g., iPSCs), and innovative therapeutic modalities (e.g., engineered exosomes, gene therapies) creates unprecedented opportunities for developing effective treatments for neurodegenerative diseases. By focusing on the shared cytoskeletal pathology that underlies diverse neurodegenerative conditions and implementing the strategic frameworks outlined in this whitepaper, researchers and drug development professionals can meaningfully advance the treatment of these devastating disorders.
Integrating Cytoskeletal Biomarkers with Other Hallmarks of Neurodegeneration
The cytoskeleton, a dynamic network of intracellular filaments, is fundamental to neuronal health, governing cellular shape, intracellular transport, and synaptic plasticity. In neurodegenerative diseases (NDDs), dysregulation of this critical infrastructure is not merely a secondary consequence but a core driver of pathology that intersects with all other major hallmarks of neurodegeneration [69]. The cytoskeleton comprises three primary polymer systems: microfilaments (actin), intermediate filaments, and microtubules, each of which becomes compromised in NDDs [9]. A growing body of evidence positions cytoskeletal dysfunction as a pivotal convergent mechanism in conditions like Alzheimer's disease (AD), Parkinson's disease (PD), and amyotrophic lateral sclerosis (ALS) [22] [69]. The integration of cytoskeletal biomarkers with other pathological indicators offers a transformative approach for understanding disease progression, developing targeted therapies, and creating precise diagnostic tools. This whitepaper examines the molecular interplay between cytoskeletal elements and key neurodegenerative pathways, providing a technical framework for researchers and drug development professionals seeking to exploit these connections for therapeutic innovation.
The mechanistic relationship between cytoskeletal pathology and protein aggregation—a hallmark of NDDs—is particularly revealing. In AD, pathological forms of tau protein dissociate from microtubules and aggregate into neurofibrillary tangles (NFTs), directly compromising cytoskeletal integrity and axonal transport [110]. Similarly, in PD, α-synuclein aggregates into Lewy bodies, which disrupt neuronal cytoskeletal architecture [110]. These aggregates do not exist in isolation; they actively impair cytoskeletal function while their formation is influenced by cytoskeletal status, creating a vicious cycle of degeneration. Furthermore, recent research has illuminated how cytoskeletal defects initiate and amplify neuroinflammatory responses by activating microglia, the CNS-resident immune cells [99]. Understanding these interconnected pathways provides unprecedented opportunities for developing multi-target therapeutic strategies and biomarker panels that reflect the complex pathophysiology of NDDs.
Cytoskeletal Biomarkers in Neurodegenerative Pathways
Molecular Interplay Between Cytoskeletal Proteins and Aggregation-Prone Proteins
The protein interactomes of amyloid-β precursor protein (APP), microtubule-associated protein tau (MAPT), and α-synuclein (SNCA) reveal extensive interconnections with cytoskeletal regulatory systems. Integrated network analyses have identified BACE1, PSEN1, SORL1, GSK3B, CDK5, SNCAIP, PRKN, and APOE as high-confidence physical and functional interactors with these central pathogenic proteins [110]. These interactions frequently manifest as regulatory modules involving cleavage, phosphorylation, and ubiquitination—post-translational modifications that directly control cytoskeletal dynamics [110]. For instance, glycogen synthase kinase 3β (GSK3B) and cyclin-dependent kinase 5 (CDK5) phosphorylate tau, reducing its affinity for microtubules and promoting its aggregation into NFTs [110]. This process directly links kinase signaling pathways to both cytoskeletal destabilization and protein aggregation.
The following table summarizes key cytoskeletal-associated proteins and their roles in neurodegenerative processes:
Table 1: Key Cytoskeletal-Associated Proteins in Neurodegeneration
| Protein/Gene | Primary Function | Role in Neurodegeneration | Associated Diseases |
|---|---|---|---|
| MAPT (Tau) | Microtubule stabilization and axonal transport | Hyperphosphorylation leads to NFT formation | AD, FTD, PSP, CBD [22] |
| SNCA (α-Synuclein) | Presynaptic vesicle trafficking | Misfolding and aggregation into Lewy bodies | PD, DLB, MSA [110] |
| Cofilin | Actin depolymerization | Forms cofilin-actin rods under stress | AD, PD [69] |
| NF-L | Neuronal intermediate filament structure | Mutations disrupt axonal integrity | CMT, ALS [22] |
| TREM2 | Microglial phagocytosis and activation | Variants impair clearance of protein aggregates | AD, PD, FTD, ALS [99] |
Cytoskeletal integrity significantly influences the aggregation kinetics of pathogenic proteins. Cofilin-actin rods, which form in response to oxidative and energetic stress, serve as accumulation sites for APP and facilitate tau accumulation and fibril formation [69]. These rods, comprised primarily of dephosphorylated (active) cofilin and ADP-actin in a 1:1 ratio, represent a critical point of convergence between stress signaling pathways and cytoskeletal pathology [69]. The presence of Aβ activates the Cdc42 pathway leading to subsequent downregulation of RhoA and LIMK, resulting in cofilin dephosphorylation and further rod formation [69]. This self-reinforcing cycle directly connects amyloid pathology with cytoskeletal dysfunction through well-defined signaling cascades.
Cytoskeletal Dysregulation as a Driver of Neuroinflammation
Microglial dysfunction represents another core hallmark of NDDs that is intimately connected to cytoskeletal pathology. Microglia rely on their actin cytoskeleton for critical functions including phagocytosis, process motility, and cytokine release. Recent research has identified several microglial genes with strong associations to NDDs, such as TREM2, CD33, and progranulin (PGRN), which are now emerging as promising therapeutic targets [99]. These genes regulate microglial phagocytosis of protein aggregates, including Aβ, TDP-43, and α-Syn, with their dysfunction leading to accumulated pathology [99]. The triggering receptor expressed on myeloid cells 2 (TREM2) is particularly significant, as its variants confer substantial risk for AD, PD, FTD, and ALS [99].
The relationship between cytoskeletal elements and neuroinflammation is bidirectional. While microglial activation influences neuronal cytoskeletal integrity through inflammatory mediators, neuronal cytoskeletal breakdown products further activate microglial responses. Disease-associated microglia (DAM), neurodegenerative microglia (MGnD), and other activated microglial states exhibit distinct cytoskeletal arrangements that enable their pathological functions [99]. Therapeutic strategies targeting TREM2, such as AL002 (Alector) and VG-3927 (Vigil Neurosciences), aim to enhance microglial phagocytic function by modulating downstream signaling pathways that ultimately reorganize the microglial cytoskeleton to improve clearance of pathological protein aggregates [99].
Computational Identification of Cytoskeletal Biomarkers in Age-Related Diseases
Advanced computational approaches have accelerated the identification of cytoskeletal biomarkers with diagnostic and prognostic potential. One recent integrative study employed machine learning-based models and differential expression analysis to investigate transcriptional changes of cytoskeletal genes in five age-related diseases: Hypertrophic Cardiomyopathy (HCM), Coronary Artery Disease (CAD), Alzheimer's disease (AD), Idiopathic Dilated Cardiomyopathy (IDCM), and Type 2 Diabetes Mellitus (T2DM) [9]. Using Support Vector Machines (SVM) classifiers with Recursive Feature Elimination (RFE), researchers identified 17 cytoskeletal genes strongly associated with these conditions, achieving high classification accuracy between patient and normal samples [9].
Table 2: Machine Learning-Identified Cytoskeletal Biomarkers for Age-Related Diseases
| Disease | Identified Cytoskeletal Biomarkers | Potential Functional Significance |
|---|---|---|
| Alzheimer's Disease (AD) | ENC1, NEFM, ITPKB, PCP4, CALB1 | Neuronal structure, calcium signaling, synaptic function [9] |
| Coronary Artery Disease (CAD) | CSNK1A1, AKAP5, TOPORS, ACTBL2, FNTA | Kinase activity, actin regulation, protein prenylation [9] |
| Hypertrophic Cardiomyopathy (HCM) | ARPC3, CDC42EP4, LRRC49, MYH6 | Actin nucleation, GTPase regulation, myosin function [9] |
| Idiopathic Dilated Cardiomyopathy (IDCM) | MNS1, MYOT | Ciliary function, sarcomeric organization [9] |
| Type 2 Diabetes Mellitus (T2DM) | ALDOB | Glucose metabolism and cytoskeletal interactions [9] |
The study revealed important overlapping genes between conditions, suggesting shared cytoskeletal pathways across age-related diseases. For instance, ANXA2 was common to AD, IDCM, and T2DM, while TPM3 connected AD, CAD, and T2DM [9]. The SPTBN1 gene was shared across AD, CAD, and HCM [9]. These overlapping signatures highlight potential common pathological mechanisms and suggest opportunities for developing broad-spectrum therapeutic approaches targeting cytoskeletal dysregulation in multiple age-related conditions.
Experimental Approaches for Cytoskeletal Biomarker Research
Methodologies for Mapping Protein Interactomes
Elucidating the complex protein-protein interaction (PPI) networks centered on cytoskeletal elements requires sophisticated methodological approaches. A robust protocol for identifying direct interactors involves using the Search Tool for the Retrieval of Interacting Genes/Proteins (STRING) database with high-confidence interaction thresholds (combined score ≥ 0.9) [110]. This approach should be followed by network analysis using platforms like Cytoscape to construct and visualize PPI networks, with subsequent identification of hub proteins through topological algorithms and centrality measures [110]. Key analytical metrics include the number of nodes (interacting proteins), edges (protein-protein associations), average node degree, average local clustering coefficient, and PPI enrichment p-value [110].
For researchers specifically investigating cytoskeletal interactions, the following workflow is recommended:
- Selection of NDD Protein Targets: Focus on major causative proteins for selected NDDs, particularly APP and MAPT for AD, and SNCA for PD [110].
- Identification of Interacting Proteins: Use STRING with organisms set to "Homo sapiens," applying high-confidence interactions (combined score ≥ 0.9) and selecting a maximum of 100 interactors in the first shell [110].
- PPI Network Analysis: Import PPI data into Cytoscape and compute topological parameters using Network Analyzer, focusing on centrality measures like node degree distribution and edge betweenness [110].
- Hub Protein Identification: Utilize the CytoHubba plugin in Cytoscape to rank proteins based on multiple centrality measures [110].
- Functional Enrichment Analysis: Perform Gene Ontology and pathway analysis to identify biological processes, molecular functions, and disease-driving pathways significantly enriched among interacting proteins [110].
This integrated approach successfully identified BACE1, PSEN1, SORL1, GSK3B, CDK5, SNCAIP, PRKN, and APOE as key interactors with APP, MAPT, and SNCA, providing novel insights into potential therapeutic targets [110].
Detection and Monitoring of Cofilin-Actin Rods
The formation of cofilin-actin rods represents a specific cytoskeletal pathology with relevance to multiple NDDs. These rods are largely comprised of dephosphorylated (active) cofilin and ADP-actin in a 1:1 ratio and form in response to various stressors, including ATP depletion, hydrogen peroxide exposure, and glutamate excitotoxicity [69]. Standard protocols for inducing cofilin-actin rods in cultured hippocampal neurons include treatment with 10 mM NaN₃ and 6 mM 2-deoxyglucose for 30 minutes (ATP depletion), 10 μM hydrogen peroxide for 60 minutes, or 150-300 μM glutamate for 30 minutes [69].
A significant methodological challenge is that conventional actin visualization tools like Lifeact and phalloidin are ineffective for monitoring cofilin-actin rods; Lifeact does not bind to these structures, and phalloidin stains them weakly or not at all [69]. Therefore, researchers must employ alternative detection methods:
- Immunofluorescence staining using antibodies specific to cofilin or phosphorylated cofilin [69]
- Live-cell imaging with cofilin fusion proteins (e.g., CFP-cofilin) [69]
- Site-directed mutagenesis to identify critical residues involved in rod formation, such as intramolecular cofilin oxidation sites (C147-C139 and C80-C39) [69]
Recent studies using Dictyostelium discoideum have revealed that hyperosmotic shock (200-400 mM sorbitol) induces cofilin-actin rod formation accompanied by a drop in intracellular pH, suggesting a mechanistic link between pH-regulated phase separation and cytoskeleton-associated disease progression [69].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Research Reagent Solutions for Cytoskeletal Biomarker Investigations
| Reagent/Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Cell Culture Models | Immortalized cell lines (HeLa, HEK 293), Primary hippocampal neurons, Dictyostelium discoideum | Proof-of-principle experiments, study of rod formation [69] | Neuronal cultures more biologically relevant but harder to maintain |
| Actin Visualization Tools | Lifeact, Phalloidin, Cofilin antibodies | Monitoring actin-rich structures and rods [69] | Lifeact and phalloidin ineffective for cofilin-actin rods |
| Stress Inducers | Sodium azide, 2-deoxyglucose, Hydrogen peroxide, Glutamate, Hyperosmotic shock (sorbitol) | Induction of cofilin-actin rods [69] | Concentration and duration critical for specific rod formation |
| Computational Tools | STRING database, Cytoscape with CytoHubba plugin, SVM classifiers with RFE | PPI network analysis, hub protein identification, biomarker discovery [110] [9] | High-confidence interaction scores (≥0.9) reduce false positives |
| Microglial Modulators | TREM2-activating antibodies (AL002), VG-3927 (small molecule TREM2 agonist) | Targeting microglial-cytoskeletal interactions [99] | Monitor for potential microglial senescence with prolonged activation |
Visualization of Integrated Pathways
The following diagram illustrates the core signaling pathway linking major neurodegenerative triggers to cytoskeletal pathology through cofilin-actin rod formation:
The integrated relationship between cytoskeletal biomarkers and other hallmarks of neurodegeneration can be visualized through the following experimental framework:
The integration of cytoskeletal biomarkers with other hallmarks of neurodegeneration represents a paradigm shift in our understanding and approach to NDDs. Rather than viewing cytoskeletal pathology as a downstream consequence, evidence now firmly establishes it as a central driver that intersects with all major neurodegenerative processes, including protein aggregation, neuroinflammation, synaptic dysfunction, and axonal transport deficits [110] [99] [69]. The identification of specific molecular players, such as cofilin-actin rods, and the mapping of comprehensive protein interactomes centered on APP, MAPT, and SNCA provide unprecedented opportunities for therapeutic intervention [110] [69]. Furthermore, computational approaches leveraging machine learning algorithms have demonstrated remarkable efficacy in identifying cytoskeletal gene signatures with diagnostic and prognostic value across multiple age-related diseases [9].
Future research directions should prioritize the development of novel detection methodologies for cytoskeletal pathologies, particularly improved tools for monitoring cofilin-actin rod dynamics in living cells and organisms [69]. Additionally, the therapeutic potential of targeting cytoskeletal-regulatory proteins such as TREM2, GSK3B, and CDK5 warrants expanded investigation through rigorously designed clinical trials [110] [99]. The emerging paradigm of companion diagnostics, already established in oncology, should be adapted for neurodegenerative diseases to enable patient stratification based on cytoskeletal biomarker profiles and to monitor treatment responses [99]. By embracing this integrated approach that positions cytoskeletal biomarkers at the forefront of neurodegenerative disease research, the scientific community can accelerate the development of effective strategies to combat these devastating conditions.
Conclusion
Cytoskeletal defects represent a fundamental pathological mechanism shared across diverse neurodegenerative diseases, contributing to axonal transport deficits, mitochondrial mislocalization, and eventual neuronal death. The integration of research from foundational mechanisms to therapeutic applications reveals promising targets, including microtubule stabilizers, HDAC inhibitors, and ROCK pathway modulators. However, significant challenges remain in optimizing blood-brain barrier penetration, timing interventions appropriately, and developing validated biomarkers for patient stratification. Future research should focus on personalized approaches that account for disease-specific cytoskeletal vulnerabilities, combination therapies targeting multiple hallmarks of neurodegeneration, and advanced biomarker development to track treatment efficacy. The cytoskeleton presents not only a pathological feature but a promising therapeutic frontier for potentially modifying the progression of neurodegenerative disorders.
References
- 1. The Cytoskeleton – Fundamentals of Cell Biology [https://open.oregonstate.education/cellbiology/chapter/cytoskeleton/]
- 2. Cytoskeleton [https://en.wikipedia.org/wiki/Cytoskeleton]
- 3. Cytoskeletal Defects - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/neuroscience/cytoskeletal-defects]
- 4. The Cytoskeleton and Cell Behavior - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK26930/]
- 5. Cytoskeleton dysfunction of motor neuron in spinal muscular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11638312/]
- 6. Imaging microtubule dynamics: A new frontier in biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12455249/]
- 7. The role of neurofilament aggregation in neurodegeneration [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-019-0318-4]
- 8. The Interaction of Neurofilaments with the Microtubule Motor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC524780/]
- 9. A computational framework for identifying cytoskeletal ... [https://www.nature.com/articles/s41598-025-97363-y]
- 10. The Global Neurodegeneration Proteomics Consortium [https://www.nature.com/articles/s41591-025-03834-0]
- 11. Hallmarks of neurodegenerative diseases - PubMed - NIH [https://pubmed.ncbi.nlm.nih.gov/36803602/]
- 12. Hallmarks of neurodegenerative diseases [https://profiles.wustl.edu/en/publications/hallmarks-of-neurodegenerative-diseases]
- 13. Cell mechanics and the cytoskeleton - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC2851742/]
- 14. Identification of actin mutants with neurodegenerative ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2025.1543199/full]
- 15. Cytoskeletal protein abnormalities in neurodegenerative ... [https://mayoclinic.elsevierpure.com/en/publications/cytoskeletal-protein-abnormalities-in-neurodegenerative-diseases/]
- 16. Novel therapeutic approaches to target neurodegeneration [https://pmc.ncbi.nlm.nih.gov/articles/PMC10952850/]
- 17. The role of the cytoskeleton in fibrotic diseases [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1490315/full]
- 18. Disruption of axonal transport in neurodegeneration [https://www.jci.org/articles/view/168554/figure/1]
- 19. Axonal transport of CHMP2b is regulated by kinesin ... [https://pubmed.ncbi.nlm.nih.gov/40021219/]
- 20. 生命学院王彤组发现钙信号调控下的核糖核蛋白颗粒在神经 ... [https://www.shanghaitech.edu.cn/2025/1110/c1006a1116734/page.htm]
- 21. Neurodegeneration: diseases of the cytoskeleton? [https://www.nature.com/articles/4400764]
- 22. The cytoskeleton in neurodegenerative diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3011821/]
- 23. Links of Cytoskeletal Integrity with Disease and Aging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9496670/]
- 24. Cytoskeletal Proteins and Alzheimer's Disease Pathogenesis [https://www.mdpi.com/2218-273X/15/6/831]
- 25. Cytoskeletal Proteins and Alzheimer's Disease Pathogenesis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12190275/]
- 26. Tau and Alpha Synuclein Synergistic Effect in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7404325/]
- 27. α-synuclein and tau: interactions, cross-seeding, and the ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1570553/full]
- 28. Alpha-synuclein and tau: teammates in neurodegeneration? [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/1750-1326-9-43]
- 29. Structural basis of a distinct α-synuclein strain that ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11982472/]
- 30. 2025 NIH Alzheimer's Disease and Related Dementias ... [https://www.nia.nih.gov/about/2025-nih-dementia-research-progress-report]
- 31. Novel Insights into Neurodegenerative Diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12597681/]
- 32. 神经丝蛋白的结构功能及其在肌萎缩侧索硬化症早期诊断中的研究 ... [https://ykxb.scu.edu.cn/cn/article/id/2d6141c5-5b27-4386-8b60-1d1b387901d3]
- 33. 基于定制反义寡核苷酸的神经丝相关型夏科-马里-图斯病疗法。 [https://suppr.wilddata.cn/browses/detail/pubmed/39008620]
- 34. A Conserved Cytoskeletal Signaling Cascade Mediates Neurotoxicity... [https://pubmed.ncbi.nlm.nih.gov/29138281/]
- 35. Frontotemporal dementia and parkinsonism linked to chromosome [https://en.wikipedia.org/wiki/Frontotemporal_dementia_and_parkinsonism_linked_to_chromosome_17]
- 36. Frontotemporal dementia and parkinsonism linked to chromosome ... [https://ojrd.biomedcentral.com/articles/10.1186/1750-1172-1-30]
- 37. TREM2与小胶质细胞 [https://biospective.com/zh/resources/trem2-and-microglia]
- 38. 共蛋白病新视角:重新审视神经退行性疾病的蛋白聚集网络 [https://www.ebiotrade.com/newsf/2025-11/20251108083943564.htm]
- 39. Advancing Clinical Use of Neurofilament Light Chain [https://pmc.ncbi.nlm.nih.gov/articles/PMC12575937/]
- 40. Introducing neurofilament light chain measure in psychiatry [https://www.nature.com/articles/s41380-024-02524-6]
- 41. Neurofilament light chain in Alzheimer's disease [https://www.sciencedirect.com/science/article/abs/pii/S0009898125004590]
- 42. Secreted neurofilament light chain after neuronal damage ... [https://www.sciencedirect.com/science/article/pii/S2211124725001536]
- 43. Serum neurofilament light at diagnosis: a prognostic ... [https://www.nature.com/articles/s41531-024-00768-1]
- 44. Plasma neurofilament light chain as prognostic marker of ... [https://alzres.biomedcentral.com/articles/10.1186/s13195-024-01593-7]
- 45. Serum neurofilament light chain as a diagnostic and ... [https://pubmed.ncbi.nlm.nih.gov/39680179]
- 46. Clinical utility of neurofilament light chain as a biomarker ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1660344/full]
- 47. Relevance of serum neurofilament light chain ... [https://www.sciencedirect.com/science/article/pii/S0213485325000842]
- 48. Trends in clinical studies evaluating neurofilament light chain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12453014/]
- 49. Repositioning Microtubule Stabilizing Drugs for Brain ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2018.00226/full]
- 50. Microtubule Stabilizing Agents as Potential Treatment for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3493881/]
- 51. Recent progress with microtubule stabilizers: new compounds ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4167679/]
- 52. Phase 1 trial of TPI 287, a microtubule stabilizing agent ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10849833/]
- 53. Microtubule-stabilizing agents: a growing class of important ... [https://www.sciencedirect.com/science/article/abs/pii/S1367593100002258]
- 54. Histone Deacetylases in Neurodegenerative Diseases and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567126/]
- 55. Histone deacetylase 6: A new player in oxidative stress‑ ... [https://www.spandidos-publications.com/10.3892/ijmm.2025.5578]
- 56. Advancing histone deacetylase 6 (HDAC6) as a promising ... [https://www.frontiersin.org/journals/drug-discovery/articles/10.3389/fddsv.2025.1662691/full]
- 57. HDAC6 inhibition as a mechanism to prevent ... [https://www.sciencedirect.com/science/article/pii/S2405844024106184]
- 58. The regulatory mechanisms and treatment of HDAC6 in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12497803/]
- 59. Design, synthesis, and biological evaluation of quinazolin ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523425009493]
- 60. Discovery of selective HDAC6 inhibitors driven by artificial ... [https://www.sciencedirect.com/science/article/pii/S2095177925001558]
- 61. Histone Deacetylase (HDAC) 6 Pipeline Landscape 2025 [https://finance.yahoo.com/news/histone-deacetylase-hdac-6-pipeline-091600474.html]
- 62. Histone deacetylase 6: a potential therapeutic target for ... [https://pubmed.ncbi.nlm.nih.gov/40902510/]
- 63. RhoA/ROCK/GSK3β Signaling: A Keystone in Understanding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11854763/]
- 64. RhoA/ROCK/GSK3β Signaling: A Keystone in ... [https://www.mdpi.com/1467-3045/47/2/124]
- 65. Effect of the Rho-Kinase/ROCK Signaling Pathway on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9957420/]
- 66. Protein kinases in neurodegenerative diseases [https://www.nature.com/articles/s41392-025-02179-x]
- 67. Alpha synuclein-mediated cytoskeletal dysfunction impairs ... [https://link.springer.com/article/10.1007/s00401-025-02933-z]
- 68. Inhibition of invasion by glycogen synthase kinase-3 beta ... [https://www.sciencedirect.com/science/article/abs/pii/S0006291X15301960]
- 69. Cytoskeletal dysregulation and neurodegenerative disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC9535683/]
- 70. Deep learning revolutionizes cytoskeleton research [https://www.sciencedaily.com/releases/2025/03/250318141822.htm]
- 71. Quantifying cytoskeletal organization from optical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10792062/]
- 72. Computational Approaches to Revisiting Plant ... [https://pubmed.ncbi.nlm.nih.gov/40474669/]
- 73. Overcoming the Blood–Brain Barrier: Advanced Strategies in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388969/]
- 74. Strategies for delivering drugs across the blood-brain ... [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2025.1644633/full]
- 75. The blood–brain barrier: Structure, regulation and drug ... [https://www.nature.com/articles/s41392-023-01481-w]
- 76. Advances in brain-targeted delivery strategies and natural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12107825/]
- 77. The mild cognitive impairment window for optimal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12365431/]
- 78. Early Cytoskeletal Protein Modifications Precede Overt ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2016.00494/full]
- 79. Early and Late Loss of the Cytoskeletal Scaffolding Protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5354314/]
- 80. 'A tipping point': An update from the frontiers of Alzheimer's ... [https://news.yale.edu/2025/08/08/tipping-point-update-frontiers-alzheimers-disease-research]
- 81. Stem Cell Clinical Trials and Promise of Engineered Exosomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC12409071/]
- 82. Antiageing strategy for neurodegenerative diseases [https://www.nature.com/articles/s41392-025-02145-7]
- 83. The Genomic Landscape of Compensatory Evolution [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.1001935]
- 84. Exploring potential developmental origins of common ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11440815/]
- 85. A New View of Pathway-Driven Drug Resistance in Tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5403593/]
- 86. Compensatory Evolution and the Origins of Innovations [https://pmc.ncbi.nlm.nih.gov/articles/PMC3606098/]
- 87. Septins in the nervous system: from cytoskeletal dynamics to ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02430-6]
- 88. Systemic Neurodegeneration and Brain Aging: Multi-Omics ... [https://www.mdpi.com/2227-9059/13/8/2025]
- 89. A Comprehensive Oncological Biomarker Framework Guiding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466961/]
- 90. A computational framework for identifying cytoskeletal genes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12033331/]
- 91. Biomarkers of Neurodegenerative Diseases - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9313182/]
- 92. The Future of Clinical Trials: Incorporating 'Omics for ... [https://blog.crownbio.com/the-future-of-clinical-trials-incorporating-omics-for-enhanced-stratification]
- 93. Complementary cytoskeletal feedback loops control signal ... [https://www.nature.com/articles/s41467-025-62799-3]
- 94. Neurofilaments Light Chain in Neurodegenerative Dementias [https://pmc.ncbi.nlm.nih.gov/articles/PMC10968996/]
- 95. Neurofilament Light (NF-L) Chain Protein from a Highly ... [https://www.heraldopenaccess.us/openaccess/neurofilament-light-nf-l-chain-protein-from-a-highly-polymerized-structural-component-of-the-neuronal-cytoskeleton-to-a-neurodegenerative-disease-biomarker-in-the-periphery]
- 96. Measuring neurofilament light in human plasma and ... [https://pubmed.ncbi.nlm.nih.gov/40958756/]
- 97. Blood level of neurofilament light chain as a biomarker for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11749884/]
- 98. Global research trends in biomarkers, therapeutic targets, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12009895/]
- 99. Biomarkers and therapeutic strategies targeting microglia in ... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-025-00867-4]
- 100. Comparative analysis of neuroinflammatory pathways in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12069400/]
- 101. Identification of Novel Mitochondrial Localization Signals in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5801207/]
- 102. Transgenic animal models of neurodegeneration based on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3084899/]
- 103. A Transgenic Mouse Model for Human Autosomal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1855087/]
- 104. CRISPR/Cas9: a powerful genetic engineering tool for ... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-015-0031-x]
- 105. Animal Models of Neurodegenerative Disease [https://www.frontiersin.org/journals/molecular-neuroscience/articles/10.3389/fnmol.2022.883358/full]
- 106. Gene therapy breakthroughs in ALS: a beacon of hope for 20 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12001736/]
- 107. Chapter 2 The Neuronal Cytoskeleton [https://www.sciencedirect.com/science/chapter/bookseries/abs/pii/S1566312408600528]
- 108. Neurodegenerative diseases - Improving clinical trial ... [https://neurotorium.org/next-steps-for-improving-clinical-trial-outcomes-neurodegenerative-disease/]
- 109. Drug discovery research with the iPSC models of ... [https://www.sciencedirect.com/science/article/pii/S0168010225001683]
- 110. Amyloid-β, Tau, and α-Synuclein Protein Interactomes as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12500485/]