Advanced Strategies for Cytoskeletal Drug Target Compound Screening: From Foundational Concepts to Clinical Translation
This article provides a comprehensive overview of modern compound screening strategies targeting the cytoskeleton for drug discovery.
Advanced Strategies for Cytoskeletal Drug Target Compound Screening: From Foundational Concepts to Clinical Translation
Abstract
This article provides a comprehensive overview of modern compound screening strategies targeting the cytoskeleton for drug discovery. It covers the foundational biology of microtubules, actin, and other cytoskeletal components as validated therapeutic targets, explores established and emerging high-throughput screening methodologies including tubulin polymerization assays and phenotypic profiling, addresses key challenges in specificity and predictive value, and examines advanced validation techniques. Aimed at researchers and drug development professionals, this resource synthesizes current knowledge to guide the development of next-generation cytoskeletal-targeted therapeutics with improved efficacy and reduced side effects for cancer and other diseases.
The Cytoskeleton as a Therapeutic Target: Unveiling Molecular Complexity and Druggable Sites
Frequently Asked Questions (FAQs) & Troubleshooting Guides
FAQ 1: What are the primary cytoskeletal targets in drug discovery, and what associated diseases are being investigated? The cytoskeleton offers several high-value targets for therapeutic intervention, primarily focused on microtubules and actin, with relevance to cancer, neurodegenerative diseases, and bacterial infections. The table below summarizes key targets and their therapeutic context.
Table 1: Key Cytoskeletal Targets in Drug Discovery
| Target Protein | Associated Diseases | Common Assay Types |
|---|---|---|
| Tubulin | Cancer, Gout, Arthritis | Polymerization, Binding, Spin-down, Live cell [1] |
| Kinesin (e.g., KIF18A) | Cancer, Neurodegeneration | Microtubule-activated ATPase [1] |
| Cardiac Myosin | Cardiomyopathies | Actin-activated ATPase, Calcium-activated ATPase [1] |
| FtsZ (Bacterial) | Bacterial Infection | Polymerization, GTPase [1] |
Troubleshooting Guide: Addressing Off-Target Effects in Cytoskeletal Drug Screens
- Problem: A compound designed to inhibit a specific kinesin (e.g., KIF18A) shows unexpected cellular effects, suggesting off-target activity.
- Background: Many cytoskeletal proteins, such as kinesins, belong to large families with homologous structures, increasing the risk of cross-reactivity [1].
- Solution: Implement a comprehensive motor panel counter-screen.
- Protocol: Test your lead compounds against a panel of related motor proteins (e.g., KIF2, KIF3C, KIF11, KIF20A, etc.) to determine IC₅₀ values for each [1].
- Expected Outcome: Confirmation of target specificity. For example, a high-quality inhibitor will be highly specific to KIF18A and its close homologs (KIF18B, KIF19A) while showing minimal activity against other kinesins [1].
- Data Interpretation: Prioritize compounds with a high selectivity index for further development.
FAQ 2: How does the cytoskeleton contribute to drug resistance, particularly to chemotherapeutics like paclitaxel? A novel mechanism of resistance to microtubule-targeting drugs like paclitaxel involves the interplay between tubulin post-translational modifications and the cytoskeletal component septins [2].
- Key Players:
- Tubulin Polyglutamylation: Catalyzed by enzymes TTLL5 (branching initiation) and TTLL11 (chain elongation), this modification alters the microtubule surface [2].
- Septin Overexpression: Specifically, the overexpression of septins (SEPT2, SEPT6, SEPT7, SEPT9_i1) and their relocalization from actin fibers to microtubules is a critical event [2].
- Resistance Mechanism: High levels of tubulin polyglutamylation and SEPT9_i1 create a scaffold on microtubules that enhances the recruitment of proteins like CLIP-170 and MCAK. These proteins increase microtubule dynamics, thereby counteracting the stabilizing effect of paclitaxel and leading to drug resistance [2].
Troubleshooting Guide: Investigating Paclitaxel Resistance in a Cell Model
- Problem: Your previously paclitaxel-sensitive cancer cell line has developed resistance.
- Hypothesis: Resistance is driven by the septin-polyglutamylation pathway.
- Experimental Approach:
- Expected Result: Cells overexpressing the combination of septins and polyglutamylases will show significantly higher survival rates in paclitaxel compared to control cells, confirming the sufficiency of this mechanism to induce resistance [2].
FAQ 3: What is the function of septins in cytoskeletal crosstalk? Septins are considered the fourth component of the cytoskeleton and are crucial for mediating crosstalk between microtubules and actin filaments [3] [4]. They act as a molecular linker that captures and guides the growth of actin filaments along microtubule lattices [3]. This function is essential for cellular morphogenesis, particularly in structures like neuronal growth cones, where it helps maintain the peripheral actin network that fans out from microtubules [3].
Comparative Data Tables
Table 2: Core Structural and Functional Properties of Cytoskeletal Components
| Property | Microfilaments (Actin) | Intermediate Filaments | Microtubules | Septins |
|---|---|---|---|---|
| Diameter | ~7 nm [5] | ~10 nm [5] [6] | ~23 nm [5] [6] | Filamentous GTP-binding proteins [4] |
| Protein Subunit | Actin [5] | Tissue-specific (e.g., Keratin, Vimentin, Neurofilaments, Lamins) [5] [6] | α- and β-Tubulin heterodimer [5] | Hetero-oligomers (e.g., SEPT2-SEPT6-SEPT7) [4] [2] |
| Dynamic Instability | Yes [6] | No [6] | Yes [6] | More stable than actin/MTs; assembly state affects function [4] |
| Primary Functions | Muscle contraction, cell movement, cytokinesis, maintenance of cell shape [5] | Mechanical strength, organelle anchoring, nuclear integrity [5] [6] | Intracellular transport, chromosome segregation, cell motility (cilia/flagella) [5] | Scaffold & diffusion barrier; direct actin-microtubule cross-linking [3] [4] |
Key Experimental Protocols
Protocol 1: In Vitro Tubulin Polymerization Assay for Compound Screening
This assay is a cornerstone for identifying compounds that stabilize or destabilize microtubules, a key mechanism for anti-cancer drugs [1].
- Reagent Preparation: Prepare a solution of purified porcine brain tubulin in a chilled GTP-supplemented polymerization buffer [1].
- Compound Addition: Add the test compound to the tubulin solution on ice. Include controls (e.g., vehicle control, paclitaxel as a stabilizer, vinca alkaloid as a destabilizer).
- Initiate Polymerization: Transfer the solution to a pre-warmed cuvette and immediately place it in a spectrophotometer equipped with a temperature-controlled chamber set to 37°C.
- Data Collection: Monitor the increase in turbidity (optical density) at 340 nm over time. Microtubule polymerization leads to a increase in light scattering, which appears as a sigmoidal curve: a lag phase (nucleation), a growth phase (elongation), and a plateau phase (steady state) [1].
- Data Analysis: Compare the polymerization kinetics of the test sample to controls. Compounds that stabilize microtubules will typically show a shorter lag phase and a steeper growth phase, while destabilizers will suppress the overall increase in OD₃₄₀.
Protocol 2: Reconstitution of Septin-Mediated Actin-Microtubule Crosstalk
This assay visually demonstrates how septins directly couple actin filaments to microtubules [3].
- Component Preparation:
- Purify and stabilize microtubules.
- Purify actin and pre-polymerize into filaments (F-actin) using phalloidin for stabilization.
- Purify recombinant septin complexes (e.g., SEPT2/6/7) [3].
- Assay Assembly for TIRF Microscopy:
- Immobilize stabilized microtubules on a passivated glass chamber.
- Coat the microtubules with a physiological concentration (e.g., 200-500 nM) of the septin complex.
- Introduce pre-polymerized, fluorescently labeled actin filaments into the chamber.
- Image Acquisition: Use time-lapse Total Internal Reflection Fluorescence (TIRF) microscopy to capture binding events.
- Analysis: Quantify the percentage of microtubule length decorated with actin filaments in the presence vs. absence of septins. In the presence of septins, you will observe stable capture and alignment of actin filaments along the microtubule lattice, and even polymerization of actin from the microtubule-bound sites [3].
Signaling Pathways and Workflow Visualizations
Diagram 1: Resistance pathway.
Diagram 2: Septin crosstalk mechanism.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Cytoskeletal Compound Screening Research
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Purified Tubulin | Core subunit for in vitro polymerization and binding assays. | Screening for compounds that modulate microtubule stability [1]. |
| Recombinant Septin Complexes | For reconstituting cytoskeletal crosstalk and studying septin-specific functions. | In vitro assays to test if a compound disrupts septin-mediated actin-microtubule binding [3]. |
| Stabilized Actin Filaments (F-actin) | Pre-formed actin polymers for interaction and motor protein assays. | Studying myosin function or actin-septin interactions [1] [3]. |
| Kinesin Motor Panel | A set of purified kinesin proteins for selectivity screening. | Counter-screening to ensure a kinesin inhibitor is target-specific and avoids off-target effects [1]. |
| Polyglutamylation Enzymes (TTLL5, TTLL11) | To introduce specific tubulin post-translational modifications in vitro. | Modeling the modified microtubule surface found in paclitaxel-resistant cells [2]. |
Troubleshooting Guide: Microtubule-Targeting Agent Research
FAQ 1: What are the primary binding sites on tubulin for clinically approved MTAs, and how do they affect microtubule dynamics?
Microtubule-Targeting Agents (MTAs) exert their effects by binding to specific sites on tubulin, primarily on the β-tubulin subunit, leading to either stabilization or destabilization of microtubules [7] [8]. The table below summarizes the key binding sites and their mechanisms.
- Table 1: Key Tubulin Binding Sites and Mechanisms of Action
| Binding Site | Agent Class | Effect on Microtubules | Mechanism of Action | Representative Approved Drugs |
|---|---|---|---|---|
| Vinca Domain | Vinca Alkaloids | Destabilization | Inhibits tubulin assembly by sequestering tubulin into aggregates; creates a wedge between tubulin dimers [7] [9]. | Vinblastine, Vincristine [9] |
| Taxane Site | Taxanes | Stabilization | Binds to β-tubulin in the microtubule lumen, promoting polymerization and stabilizing the lattice [7] [9]. | Paclitaxel, Docetaxel, Cabazitaxel [9] |
| Colchicine Site | Colchicine, Combretastatins | Destabilization | Prevents the conformational change in tubulin required for polymerization [7]. | Colchicine (non-cancer use) [7] |
| Maytansine Domain | Maytansinoids | Destabilization | Inhibits the addition of tubulin dimers to microtubule plus ends [7] [8]. | mertansine (DM1) used in ADC Kadcyla [10] [7] |
Troubleshooting Tip: If your MTA is not producing the expected cellular phenotype (e.g., mitotic arrest), verify its binding site and intended mechanism. Off-target effects or resistance mechanisms, such as point mutations in the binding site or overexpression of specific tubulin isotypes, can alter drug efficacy [11] [7].
Diagram 1: Cellular outcomes of MTA mechanisms.
FAQ 2: Which MTAs have been successfully developed into Antibody-Drug Conjugates (ADCs), and what are their components?
Antibody-Drug Conjugates (ADCs) represent a major advancement in targeted cancer therapy, linking the cytotoxicity of MTAs to the specificity of monoclonal antibodies [10]. This design allows for precise delivery of the payload to cancer cells, minimizing off-target effects.
- Table 2: Clinically Approved Microtubule-Targeting ADCs
| Drug (Trade Name) | Target | Antibody | Linker | Cytotoxic Payload (MTA Class) | Indication |
|---|---|---|---|---|---|
| Trastuzumab emtansine (Kadcyla) | HER2 | Trastuzumab (IgG1) | Non-cleavable | DM1 (Maytansinoid) [7] | HER2+ Breast Cancer [10] |
| Enfortumab vedotin (Padcev) | Nectin-4 | IgG1 | Cleavable | MMAE (Vinca-site binder) [10] | Urothelial Carcinoma [10] |
| Brentuximab vedotin (Adcetris) | CD30 | Chimeric mAb (cAC10) | Cleavable | MMAE (Vinca-site binder) [10] | Hodgkin Lymphoma, sALCL [10] |
| Belantamab mafodotin (Blenrep) | BCMA | IgG1 | Non-cleavable | MMAF (Auristatin) [10] [12] | Relapsed/Refractory Multiple Myeloma [13] [12] |
| Sacituzumab govitecan (Trodelvy) | TROP-2 | IgG1 | Cleavable | SN-38 (Topoisomerase I inhibitor) | TNBC, Urothelial Carcinoma [10] |
Troubleshooting Tip: When evaluating a novel MTA for ADC development, consider the Drug-Antibody Ratio (DAR) and linker stability. An suboptimal DAR or an unstable linker can lead to premature payload release and systemic toxicity, while a too-stable linker may reduce efficacy [10]. The ADC assembly process, whether via cysteine (Cys) or lysine (Lys) conjugation, can impact DAR homogeneity and pharmacokinetics [10].
FAQ 3: What are the classic, historically significant MTAs and their therapeutic origins?
Many foundational MTAs were derived from natural products and have been used for decades, treating conditions from cancer to inflammatory diseases [7] [9].
- Table 3: Historical Microtubule-Targeting Agents
| Drug Name | Source | Year of Key Discovery/Approval | Primary Historical Use | MTA Class |
|---|---|---|---|---|
| Colchicine | Autumn crocus (Colchicum autumnale) | ~1500 BC (Ebers Papyrus) [7] | Gout, Inflammatory diseases [7] | Destabilizer (Colchicine site) |
| Paclitaxel (Taxol) | Pacific yew tree (Taxus brevifolia) | 1971 (Isolation) [9] | Ovarian, Breast Cancer [9] | Stabilizer (Taxane site) |
| Vinblastine & Vincristine | Madagascar periwinkle (Catharanthus roseus) | 1960s (Approval) [9] | Leukemia, Lymphoma [9] | Destabilizer (Vinca site) |
Troubleshooting Tip: When using classical MTAs like vinca alkaloids or taxanes in cell-based assays, be aware of common off-target effects. A frequent issue is peripheral neuropathy, which is often linked to the disruption of microtubule-dependent axonal transport in neurons [11] [7]. In vitro, this can manifest as altered cell morphology and impaired vesicular trafficking even in non-mitotic cells.
The Scientist's Toolkit: Research Reagent Solutions
This table details key materials and their functions for conducting research on microtubule-targeting agents.
- Table 4: Essential Reagents for MTA Research
| Research Reagent | Function in MTA Research | Key Considerations |
|---|---|---|
| Tubulin Protein (e.g., from bovine brain) | In vitro polymerization assays; binding studies to characterize novel MTAs. | Purity is critical for consistent assay results. Requires GTP and suitable buffers for polymerization. |
| Cell Lines with MTA Resistance | To study resistance mechanisms (e.g., tubulin mutations, efflux pumps). | Commonly used: HeLa, A549, and their drug-resistant derivatives. Verify resistance profile regularly. |
| Immunofluorescence Staining Kits (Anti-α/β-Tubulin) | Visualize microtubule network morphology and mitotic spindles in fixed cells. | Choose validated, high-specificity antibodies. Confocal microscopy is recommended for detailed analysis. |
| High-Throughput Screening (HTS) Assay Kits | Rapidly screen thousands of compounds for effects on tubulin polymerization. | Available in fluorescence- or absorbance-based formats. Ideal for initial hit identification [14]. |
| Reporter Cell Lines | Screen for compounds that affect receptors or pathways using luminescence/fluorescence readouts [14]. | Engineered for robust signal output (e.g., luciferase). Useful for target-based or phenotypic screening. |
Diagram 2: Typical workflow for MTA identification.
Troubleshooting Guides and FAQs
FAQ 1: Why is my tubulin polymerization assay yielding inconsistent results for compounds targeting the Vinca domain?
- Answer: Inconsistent results with Vinca alkaloids are often due to their substoichiometric and concentration-dependent mechanism. At low concentrations, vinca alkaloids can suppress microtubule dynamics without depolymerizing them, while higher concentrations lead to microtubule disintegration.
- Troubleshooting Steps:
- Confirm Drug Concentration: Re-prepare drug stock solutions and perform a dose-response curve (e.g., 0.1 µM to 10 µM) to identify the optimal concentration for your assay system.
- Standardize Tubulin Source and Purity: Use a consistent, high-purity tubulin source (e.g., porcine brain tubulin) to minimize variability [1].
- Control Temperature and Assembly Time: Ensure the polymerization assay is performed at a consistent temperature (typically 37°C) and that readings are taken at the same time point after initiation.
- Include Appropriate Controls: Always include a vehicle control (e.g., DMSO) and a positive control (e.g., paclitaxel for polymerization, vinblastine for depolymerization).
FAQ 2: My colchicine-binding site inhibitor (CBSI) shows high potency in enzymatic assays but poor cellular efficacy. What could be the cause?
- Answer: This discrepancy is common and can arise from several factors:
- Cellular Penetration: CBSIs may have poor membrane permeability. Consider evaluating logP and performing a cell-based uptake assay.
- Efflux by Transporters: Many CBSIs are substrates for multidrug resistance (MDR) transporters like P-glycoprotein. Test efficacy in cell lines with and without MDR overexpression [15] [16].
- Serum Binding: The compound may be highly bound by serum proteins, reducing its free, active concentration. Repeat assays in the presence of serum.
- Binding Site Flexibility: The colchicine binding domain contains flexible loops (e.g., the βT7 loop) whose conformation is highly ligand-dependent, which can affect binding in the cellular context compared to the purified protein environment [15].
FAQ 3: What are the key considerations when designing an Antibody-Drug Conjugate (ADC) using a maytansinoid payload?
- Answer: The primary goal is to enhance tumor specificity and reduce systemic toxicity.
- Linker Stability: The linker connecting the maytansinoid (e.g., DM1 or DM4) to the antibody must be stable in circulation but efficiently cleavable inside the target cancer cell (e.g., by lysosomal enzymes).
- Drug-to-Antibody Ratio (DAR): Optimize the DAR (typically 3-4) to maximize efficacy while maintaining good pharmacokinetics and low aggregation.
- Target Antigen Selection: The target antigen should be highly and uniformly expressed on tumor cells with minimal expression on healthy tissues.
- Payload Mechanism: Remember that maytansine inhibits microtubule assembly by binding to tubulin at the rhizoxin site, strongly suppressing microtubule dynamics and leading to mitotic arrest [17] [18].
FAQ 4: How does the stabilization mechanism of peloruside differ from that of paclitaxel, and how can I demonstrate this experimentally?
- Answer: While both are microtubule-stabilizing agents (MSAs), they bind to distinct sites and have different structural consequences.
- Mechanism: Paclitaxel binds the luminal taxane-site and can induce structural heterogeneity in the microtubule lattice. In contrast, peloruside binds a site on the microtubule exterior and acts primarily at lateral contacts, regularizing the lattice and even overriding the heterogeneity induced by paclitaxel in doubly-bound structures [19] [20].
- Experimental Demonstration:
- Competitive Binding: Perform a binding assay (e.g., a fluorescent anisotropy competition assay) to show that peloruside does not compete with a labeled taxane-site binder for tubulin binding.
- Structural Analysis: Use cryo-EM to compare microtubule structures stabilized by each drug. This can reveal the differences in lattice parameters and seam conformity [19].
- Combination Studies: Show that the combination of peloruside and paclitaxel has a synergistic effect on microtubule assembly and stability [19].
Quantitative Data on Tubulin Inhibitors
Table 1: Summary of Microtubule-Targeting Agents and Their Binding Sites
| Binding Site | Representative Drugs | Primary Mechanism of Action | Key Structural Insights | Main Clinical Toxicities |
|---|---|---|---|---|
| Vinca Domain [21] | Vinblastine, Vincristine, Vinorelbine | Inhibits microtubule assembly by disrupting tubulin dimer addition and suppressing microtubule dynamics. | Binds to tubulin ends, inducing a "kinetic cap" that suppresses growth and shortening. Two high-affinity binding sites per tubulin dimer [21]. | Neutropenia (Vinblastine), Peripheral Neuropathy (Vincristine), Vesicant [21]. |
| Taxane Site [19] [22] | Paclitaxel (Taxol), Docetaxel, Zampanolide | Stabilizes microtubules, inhibits dynamics, and promotes assembly. | Binds to β-tubulin on the luminal side. Can induce lattice expansion and structural heterogeneity. Stabilizes the βM-loop to reinforce lateral contacts [19] [22]. | Peripheral Neuropathy, Neutropenia, Hypersensitivity reactions. |
| Colchicine Site [15] [16] | Colchicine, Nocodazole, Plinabulin | Inhibits microtubule assembly by preventing the curved-to-straight conformational transition of tubulin. | Binds at the interface of α- and β-tubulin. The flexible βT7 loop can adopt a "flipped-in" conformation that occludes the site in the absence of ligand [15]. | Gastrointestinal toxicity (Colchicine), Generally less susceptible to multidrug resistance [15]. |
| Maytansine Site [17] [18] | Maytansine (Maitansine), DM1, DM4 | Destabilizes microtubules by inhibiting assembly and strongly suppressing microtubule dynamics. | Binds to tubulin at the rhizoxin binding site. The binding mode has been characterized, showing it interacts with a specific site on β-tubulin [17]. | Systemic toxicity (parent compound); side effects are target-dependent when used as an ADC payload (e.g., T-DM1: thrombocytopenia, hepatotoxicity) [18]. |
Experimental Protocols for Key Assays
Protocol 1: Tubulin Polymerization Assay
Purpose: To quantitatively measure the effect of a compound on the kinetics of microtubule assembly in vitro. Reagents:
- Purified tubulin (>95% purity) [1]
- G-PEM buffer (80 mM PIPES pH 6.9, 2 mM MgCl₂, 0.5 mM EGTA, 1 mM GTP)
- Test compound dissolved in DMSO
- Vehicle control (DMSO)
- Positive control (e.g., Paclitaxel)
Methodology:
- Prepare a solution of tubulin (e.g., 3 mg/mL) in cold G-PEM buffer.
- Dispense the tubulin solution into a pre-chilled quartz cuvette or a multi-well plate.
- Add the test compound, positive control, or vehicle. Keep the final DMSO concentration consistent and low (typically <1%).
- Immediately place the cuvette/plate in a spectrophotometer or fluorometer (equipped with a temperature-controlled chamber) pre-warmed to 37°C.
- Continuously monitor the increase in turbidity (absorbance at 340 nm) or fluorescence (if using a reporter dye) for 60-90 minutes.
- Analyze the polymerization curves: Lag phase, growth rate (slope), and final plateau (polymer mass).
Protocol 2: Competitive Binding Assay using Fluorescence Anisotropy
Purpose: To determine if a test compound competes for binding with a known, fluorescently-labeled ligand at a specific site (e.g., the maytansine site). Reagents:
- Purified tubulin
- Fluorescent tracer (e.g., a fluorescently-labeled maytansinoid) [17]
- Test compounds
- Reference inhibitor (unlabeled maytansine)
Methodology:
- Prepare a fixed concentration of tubulin and the fluorescent tracer in an appropriate assay buffer.
- Titrate with increasing concentrations of the test compound or the reference inhibitor.
- Incubate the mixture to reach binding equilibrium.
- Measure the fluorescence anisotropy for each sample.
- Analyze the data: A decrease in anisotropy indicates that the test compound is displacing the fluorescent tracer from its binding site. Fit the data to a competitive binding model to calculate the inhibitory constant (Ki).
Research Reagent Solutions
Table 2: Essential Materials for Tubulin Compound Screening
| Research Reagent | Function / Application | Example Use-Case |
|---|---|---|
| Porcine Brain Tubulin [1] | High-purity tubulin for in vitro polymerization and binding assays. | The primary substrate for biochemical assays to directly measure compound effects on microtubule dynamics. |
| Fluorescent Tracers (e.g., for maytansine site) [17] | Enable binding affinity and competition measurements via fluorescence anisotropy. | Determining if a novel compound binds to the maytansine site by competing with the tracer. |
| Stabilized Microtubules | Used in spin-down assays or as substrates for motor protein ATPase assays. | Differentiating between compounds that disrupt existing microtubules versus those that only prevent new assembly. |
| Kinesin Motor Proteins (e.g., KIF18A) [1] | Targets for anti-mitotic drugs; used in ATPase activity assays. | Counter-screening to ensure compound specificity for tubulin and not mitotic kinesins. |
| T2R-TTL Tubulin Complex [22] | A stable tubulin complex used for X-ray crystallography of ligand-tubulin interactions. | Determining high-resolution crystal structures of tubulin in complex with taxanes or other small molecules. |
Mechanism and Experimental Workflow Diagrams
Diagram 1: Mechanism of microtubule-targeting drugs.
Diagram 2: Drug discovery workflow for cytoskeletal targets.
The cytoskeleton, a complex network of protein filaments, is a cornerstone of cellular integrity and function. For decades, it has been a validated target for chemotherapeutics, with drugs like taxanes and vinca alkaloids focusing on a limited set of well-characterized binding sites. However, the emergence of drug resistance and dose-limiting toxicities associated with these classical targets has underscored the urgent need for innovation. This technical support article frames this challenge within the broader context of cytoskeletal drug target compound screening, guiding researchers through the opportunities and technical pitfalls of exploring novel binding sites and underexplored cytoskeletal elements. We detail experimental protocols for targeting these emerging areas, provide troubleshooting guides for common assays, and list essential reagent solutions to equip scientists and drug development professionals with the tools for next-generation discovery.
FAQs: Novel Targets and Screening Strategies
1. What constitutes an "emerging" or "novel" binding site on the cytoskeleton?
Beyond the classical taxane, vinca alkaloid, and colchicine sites, recent research has identified and characterized several novel binding sites on tubulin. These include the sites for maytansine, laulimalide/peloruside A, pironetin, and the recently discovered gatorbulin binding site [23]. Targeting these sites can help overcome resistance mechanisms that have evolved against traditional microtubule-targeting agents (MTAs). Furthermore, the cytoskeleton's role has expanded into new biological contexts, such as the DNA damage response (DDR) and cellular reprogramming, revealing proteins like the Rho/ROCK effectors and YAP/TAZ as underexplored therapeutic targets in these pathways [24] [25].
2. Beyond microtubules, what other cytoskeletal elements are gaining traction as drug targets?
While microtubules remain a prime focus, other cytoskeletal components offer rich, underexplored territory:
- Actin and its Regulators: The actin cytoskeleton is critical in cancer metastasis, neuronal plasticity in substance use disorders, and cellular reprogramming [24] [26]. Key targets include upstream regulators like the Rho GTPase family (e.g., Rac1), their effectors (e.g., the WAVE and WASP complexes), and actin-binding proteins (ABPs) such as cofilin, profilin, and non-muscle myosin II (NmII) [27] [26].
- Tubulin Post-Translational Modifications (PTMs): The "tubulin code," comprising modifications like detyrosination, is frequently altered in cancers and is linked to tumor aggressiveness and poor prognosis. Targeting the enzymes that write, read, or erase these PTMs is a promising new strategy [28].
- Cytoskeleton-Mediated Mechanotransduction: Elements that translate mechanical forces into biochemical signals, such as the perinuclear actin cap and the Linker of Nucleoskeleton and Cytoskeleton (LINC) complex, are emerging as targets to influence nuclear shape, chromatin organization, and cell fate [24].
3. What are the primary technical challenges in screening compounds against these novel targets?
Screening for novel cytoskeletal targets presents unique challenges:
- Dynamic Instability: The inherent polymerization/depolymerization dynamics of filaments can make assay readouts highly variable.
- Functional Redundancy: The cytoskeleton is a dense network of interconnected filaments and binding proteins, leading to compensatory mechanisms that can mask phenotypic effects.
- Context-Dependent Effects: A compound's impact can vary dramatically based on cell type, extracellular matrix stiffness, and cell density, as these factors directly influence cytoskeletal organization and tension [24].
- Off-Target Effects: Many regulatory proteins, like small GTPases, have pleiotropic functions, making it difficult to attribute a phenotypic change to a single intended target.
Troubleshooting Guides
Guide 1: Addressing High Variability in Polymerization Assays
Problem: High well-to-well variability in in vitro tubulin or actin polymerization assays, leading to poor Z'-factors.
| Possible Cause & Solution | Protocol Adjustment |
|---|---|
| Cause: Inconsistent reagent temperatures. Tubulin polymerization is highly sensitive to temperature fluctuations. | Solution: Pre-warm all buffers, assay plates, and tubulin samples to the exact reaction temperature (typically 37°C) before initiating polymerization. Use a thermal cycler or water bath for precise control. |
| Cause: Unstable GTP/ATP supply. Depletion of nucleotide triphosphates (GTP for tubulin, ATP for actin) halts polymerization. | Solution: Include an ATP/GTP-regenerating system in the reaction buffer. For example, for tubulin, add phosphocreatine and creatine phosphokinase to maintain a constant GTP concentration. |
| Cause: Protein quality and purity. Contaminating nucleases or proteases can degrade reagents, and aggregated protein can seed non-physiological polymerization. | Solution: Use high-purity, fresh tubulin/actin. Centrifuge the protein sample at high speed (e.g., 100,000 x g) immediately before the assay to remove any pre-formed aggregates. |
Guide 2: Interpreting Complex Phenotypes in Cell-Based Screening
Problem: A hit compound from a phenotypic screen (e.g., on cell morphology) produces an unexpected or ambiguous cytoskeletal phenotype.
| Possible Cause & Solution | Follow-up Experiment |
|---|---|
| Cause: Off-target engagement on a related cytoskeletal element. A compound intended to inhibit a microtubule motor protein might also affect actin. | Solution: Multiplexed staining. Fix and stain cells for multiple cytoskeletal components simultaneously (e.g., microtubules [green], actin [red], and DNA [blue]). Analyze co-localization and overall architecture using high-content imaging. |
| Cause: Indirect effect via mechanotransduction. The compound may be affecting substrate adhesion or stiffness sensing, indirectly altering the cytoskeleton. | Solution: Check focal adhesions and nuclear shape. Stain for vinculin or paxillin to visualize focal adhesions. Examine nuclear shape irregularities, which can indicate disruption of the LINC complex or perinuclear actin cap [24]. |
| Cause: Activation of compensatory pathways. Inhibiting one cytoskeletal network may upregulate another. | Solution: Time-course and dose-response analysis. Monitor phenotypic changes over time and across a range of concentrations. A rapid effect may be direct, while a delayed effect suggests an indirect or compensatory mechanism. |
Experimental Protocols
Protocol 1: Targeting the Actin Cytoskeleton - A Focus on Profilin and Membrane Interaction
This protocol outlines a method to investigate how small molecules modulate the interaction between the actin-binding protein profilin and membrane phosphoinositides, a key regulatory node in actin dynamics [27].
Principle: Profilin regulates actin polymerization by sequestering G-actin and promoting its addition to formin-bound filaments. Its activity is inhibited by binding to phosphoinositides like PI(4,5)P2 at the plasma membrane. Compounds that disrupt this interaction can shift the balance of actin assembly.
Workflow Diagram: Profilin-Membrane Interaction Screening
Materials:
- Cell Line: HeLa or U2OS cells.
- Plasmids: Mammalian expression vector for human profilin-1 tagged with GFP.
- Lipid Vesicles: Synthetic liposomes containing a defined percentage of PI(4,5)P2.
- Key Reagents: See the "Research Reagent Solutions" table below.
Step-by-Step Method:
- Cell Preparation: Seed cells on glass-bottom 96-well plates at 50-60% confluence. Incubate for 24 hours.
- Transfection: Transfect cells with the Profilin-1-GFP plasmid using a standard lipofection method. Incubate for 24-48 hours to allow for expression.
- Compound Treatment: Treat cells with test compounds from your library for a predetermined time (e.g., 1-4 hours). Include controls (DMSO vehicle, known pathway activators like EGF).
- Stimulation (Optional): To dynamically assess profilin release, stimulate cells with an agent that hydrolyzes PI(4,5)P2, such as an agonist for Gq-coupled receptors or a calcium ionophore.
- Fixation and Imaging: At the endpoint, fix cells with 4% paraformaldehyde for 15 minutes. Acquire high-resolution images using a confocal microscope.
- Image Analysis: Quantify the fluorescence intensity of Profilin-GFP at the cell periphery (plasma membrane) versus the cytosol. A decrease in the membrane-to-cytosol ratio indicates compound-induced dissociation of profilin from the membrane.
Protocol 2: Evaluating Compounds Targeting Tubulin Detyrosination
This protocol describes a cell-based assay to identify compounds that modulate the tubulin detyrosination cycle, a promising PTM target [28].
Principle: Tubulin detyrosination, the removal of the C-terminal tyrosine of α-tubulin, is associated with stable microtubules and is linked to aggressive cancers. This assay uses immunofluorescence to detect levels of detyrosinated tubulin (Glu-tubulin) in compound-treated cells.
Workflow Diagram: Tubulin Detyrosination Compound Screen
Materials:
- Cell Line: Any adherent cancer cell line (e.g., A549, MCF-7).
- Antibodies: Primary antibody against detyrosinated tubulin (e.g., anti-Glu-tubulin). Primary antibody against total α-tubulin. Species-specific secondary antibodies with distinct fluorophores (e.g., Alexa Fluor 488 and 555).
- Key Reagents: See the "Research Reagent Solutions" table below.
Step-by-Step Method:
- Cell Seeding and Treatment: Seed cells in 96-well imaging plates. After 24 hours, treat with test compounds for a duration that allows for microtubule turnover (typically 6-24 hours).
- Fixation and Permeabilization: Fix cells with pre-warmed 4% PFA for 15 min, then permeabilize with 0.1% Triton X-100 in PBS for 10 min.
- Immunostaining: Block cells with 1% BSA in PBS for 1 hour. Incubate with primary antibodies (anti-Glu-tubulin and anti-α-tubulin) diluted in blocking buffer overnight at 4°C. Wash and incubate with fluorescent secondary antibodies for 1 hour at room temperature. Include a nuclear counterstain (e.g., Hoechst).
- Image Acquisition and Analysis: Image plates using a high-content imaging system. Using the analysis software, segment cells based on the nuclear stain and measure the mean fluorescence intensity for both the Glu-tubulin and total tubulin channels within the cytoplasmic region.
- Data Normalization: For each cell, calculate the ratio of Glu-tubulin intensity to total tubulin intensity. Normalize the average ratio per well to the DMSO control. Compounds that significantly decrease this ratio are potential inhibitors of the detyrosination enzyme (vasohibins) or activators of the tubulin tyrosine ligase (TTL).
Research Reagent Solutions
The following table compiles key reagents essential for experiments targeting emerging cytoskeletal elements.
| Reagent Name | Target/Function | Application Note |
|---|---|---|
| Alexa Fluor Phalloidin [29] | F-actin / Binds and stabilizes filamentous actin. | Essential for visualizing actin stress fibers, cortex, and other structures in fixed cells. Available in multiple fluorophores. |
| CellLight Tubulin-GFP/RFP, BacMam 2.0 [29] | Microtubules / Labels endogenous tubulin via baculovirus delivery. | Ideal for live-cell imaging of microtubule dynamics; provides uniform labeling with low cytotoxicity. |
| Recombinant Profilin Protein | Actin Nucleation / Regulates actin monomer availability and formin-mediated elongation. | Critical for in vitro polymerization assays to study compound effects on profilin-actin or profilin-membrane interactions [27]. |
| Anti-Glu-Tubulin Antibody | Detyrosinated Tubulin / Specifically recognizes the detyrosinated form of α-tubulin. | Key reagent for immunofluorescence-based screening of compounds affecting the tubulin detyrosination cycle [28]. |
| YAP/TAZ Antibody | Mechanotransduction / Nuclear effectors of the Hippo pathway, regulated by cytoskeletal tension. | Used to assess compound effects on mechanosignaling; monitor nuclear/cytoplasmic localization [24]. |
| RhoA/Rac1/CDC42 G-LISA Activation Assay | Small GTPase Activity / Measures levels of active, GTP-bound Rho GTPases. | Colorimetric or luminescent ELISA-based kit to quantitatively screen compounds targeting upstream regulators of actin. |
| Tubulin Polymerization Assay Kit | Microtubule Dynamics / Measures tubulin polymerization kinetics in vitro via fluorescence. | A standard biochemical HTS tool for characterizing direct microtubule stabilizers/destabilizers. |
Data Presentation: Quantitative Landscape of Novel MTAs
The table below summarizes key quantitative data on established and emerging Microtubule-Targeting Agent (MTA) binding sites, providing a reference for screening outcomes and compound characterization [23].
| Binding Site Category | Representative Agents | Mechanism of Action | Development Status & Key Challenges |
|---|---|---|---|
| Taxane-site Binders | Paclitaxel, Docetaxel | Microtubule Stabilization | Approved; limited by resistance (e.g., P-gp efflux, βIII-tubulin overexpression) and toxicity (neuropathy). |
| Vinca-site Binders | Vinblastine, Vincristine | Microtubule Destabilization | Approved; challenges include inherent and acquired resistance mechanisms. |
| Colchicine-site Binders | Combretastatin A-4 | Microtubule Destabilization | Orphan drug status; extensive research into novel analogs to improve pharmacokinetics. |
| Laulimalide/Peloruside | Laulimalide, Peloruside A | Microtubule Stabilization (novel site) | Preclinical; shows efficacy in taxane-resistant models but faces formulation challenges. |
| Maytansine-site Binders | Maytansine, DM1 | Microtubule Destabilization | DM1 is an ADC payload (Kadcyla); systemic use limited by toxicity. |
| Gatorbulin-site Binners | Gatorbulin-1 | Tubulin Degradation (novel mechanism) | Early preclinical; induces unique tubulin oligomers leading to proteasomal degradation. |
Frequently Asked Questions & Troubleshooting Guides
This technical support resource addresses common challenges in cytoskeletal drug target screening, providing practical solutions for researchers and drug development professionals.
FAQ: Experimental Design and Model Selection
Q1: What are the key considerations when choosing between 2D and 3D cell culture models for cytoskeletal drug screening?
A1: The choice between 2D and 3D models significantly impacts your screening results and predictive validity.
- Traditional 2D Monolayers are suitable for initial high-throughput screening as they allow for rapid assessment of compound efficacy and cytotoxicity. However, they often overestimate compound effects and lack the physiological relevance of tumor microenvironments [30].
- 3D Spheroid Cultures better mimic solid tumor features, including structural organization, biological responses, gene expression patterns, and drug resistance mechanisms [30]. They develop distinct cellular layers:
Troubleshooting Tip: If your compound shows high efficacy in 2D cultures but fails in later-stage models, validate its activity in 3D spheroid cultures early in your screening pipeline. For instance, colchicine demonstrated potent activity in both 2D (IC~50~: 0.016-0.056 μM) and 3D AT/RT spheroid models (IC~50~: 0.004-0.023 μM), confirming its therapeutic potential across model systems [30].
Q2: How can I address differential chemosensitivity in my cancer cell models during screening?
A2: Differential chemosensitivity is a common challenge that can be leveraged to understand compound mechanisms.
- Strategy: Intentionally use cell lines with known differential sensitivity profiles. For example, in atypical teratoid/rhabdoid tumor (AT/RT) screening, BT-12 cells (chemosensitive) and BT-16 cells (chemoresistant) provide a valuable system for identifying compounds that can overcome resistance mechanisms [30].
- Implementation: Screen compounds in parallel across sensitive and resistant lines. Compounds maintaining efficacy in resistant lines may target alternative pathways or bypass common resistance mechanisms.
Troubleshooting Tip: When encountering inconsistent results across cell lines of the same cancer type, characterize their genetic backgrounds (e.g., SMARCB1 deficiency in AT/RT cells) and establish baseline sensitivity to reference cytoskeletal agents (vinca alkaloids, taxanes) to create internal reference standards [30].
FAQ: Technical Implementation and Optimization
Q3: What controls and validation steps are critical for high-throughput screening of cytoskeletal targets?
A3: Rigorous quality control is essential for generating reliable screening data.
- Control Setup: Implement stringent controls including:
- Positive controls: Known cytoskeletal agents (vincristine, paclitaxel, colchicine)
- Negative controls: Vehicle-only treatments (DMSO)
- Cell viability controls: Untreated cells for normalization [30]
- Validation Metrics: Use statistical quality parameters like Z'-factor >0.5 to ensure robust assay performance and minimize false positives/negatives.
- Secondary Validation: Follow primary screening with dose-response studies to determine IC~50~ values and assess cytotoxicity in relevant normal cells (e.g., human brain endothelial cells and astrocytes) to establish therapeutic windows [30].
Q4: How can I optimize blood-brain barrier penetration for neurological indications?
A4: BBB penetration remains a significant challenge for CNS-targeted cytoskeletal drugs.
- Compound Selection: Prioritize compounds with molecular properties conducive to BBB penetration (lower molecular weight, appropriate lipophilicity). Some microtubule-targeting agents like colchicine show favorable selectivity indices (>2 orders of magnitude) between tumor cells and normal brain cells [30].
- Delivery Strategies: Consider advanced delivery systems including nanoparticles, liposomes, and antibody-drug conjugates (ADCs) that can enhance CNS delivery while minimizing systemic exposure [31].
- Mechanistic Considerations: Evaluate effects on interphase microtubules rather than just antimitotic activity, as this may provide therapeutic benefits in neurological disorders with reduced neurotoxicity [32] [33].
Troubleshooting Tip: If promising compounds show poor BBB penetration in preclinical models, explore structural analogs or prodrug strategies that maintain cytoskeletal targeting while improving brain bioavailability.
Experimental Protocols & Data Interpretation
Protocol 1: High-Throughput Screening for Cytoskeletal-Targeting Compounds
This protocol outlines a robust framework for screening compound libraries against cytoskeletal targets [30] [34].
- Compound Library Preparation: Prepare stock plates (384-, 1536-, or 3456-well formats) of your compound library. Use liquid handling devices to transfer compounds to assay plates [34].
- Cell Culture and Plating:
- Maintain relevant cell lines (e.g., BT-12 and BT-16 for AT/RT) under standard conditions
- Seed cells in assay-compatible plates at optimized densities for 2D (traditional monolayers) or 3D (spheroid) cultures [30]
- Compound Treatment: Treat cells with test compounds (e.g., 10 μM initial concentration), positive controls (doxorubicin, known cytoskeletal agents), and vehicle controls [30].
- Viability Assessment: After appropriate incubation (typically 72 hours), measure cell viability using optimized detection methods (fluorescence intensity, luminescence, colorimetry) [34].
- Data Acquisition and Analysis:
- Use plate readers capable of high-throughput detection
- Normalize data to positive and negative controls
- Identify "hit" compounds that inhibit viability by >80% compared to controls [30]
- Perform dose-response curves for confirmed hits to determine IC~50~ values
Troubleshooting Tip: For 3D spheroid cultures, ensure uniform spheroid size and quality before compound treatment, as size variability can significantly impact compound penetration and response metrics [30].
Protocol 2: Validating Cytoskeletal-Targeting Mechanisms
This protocol confirms whether hit compounds directly target cytoskeletal components [32] [33].
- Immunofluorescence Microscopy:
- Treat cells with compounds at relevant concentrations (IC~50~-IC~80~) for 4-24 hours
- Fix, permeabilize, and stain with antibodies against tubulin (microtubules), actin (microfilaments), or relevant cytoskeletal proteins
- Include markers for DNA to assess mitotic arrest and cellular morphology
- Image using high-content or confocal microscopy
- In Vitro Tubulin Polymerization Assay:
- Incubate purified tubulin with test compounds in polymerization-promoting buffer
- Monitor microtubule formation turbidimetrically (350nm) over time at 37°C
- Compare polymerization kinetics to vehicle controls and reference agents (paclitaxel for stabilizers, vincristine/colchicine for destabilizers)
- Binding Site Characterization:
- Perform competition assays with fluorescently-labeled reference compounds (e.g., colchicine-site, vinca-site binders)
- Use structural biology approaches (crystallography, cryo-EM) for definitive binding site identification
Troubleshooting Tip: If immunofluorescence shows cytoskeletal disruption but in vitro tubulin assays are negative, investigate potential indirect mechanisms through kinase inhibition (MARK4, GSK3β) or effects on microtubule-associated proteins [35].
Table 1: Efficacy Profiles of Selected Cytoskeletal-Targeting Compounds in Preclinical Models
| Compound | Primary Target | Cancer Model efficacy (IC~50~) | Neurological Indication | Therapeutic Window |
|---|---|---|---|---|
| Colchicine | Tubulin (colchicine site) [32] | 0.016-0.056 μM (AT/RT, 2D) [30]0.004-0.023 μM (AT/RT, 3D) [30] | Gout, Pericarditis [32] | >357-fold (vs. astrocytes) [30] |
| Eribulin | Tubulin (vinca site) [32] | Breast cancer, Liposarcoma (clinical) [32] | - | Reverses EMT, improves survival [32] |
| Vinca Alkaloids | Tubulin (vinca site) [32] | Hematological malignancies (clinical) [32] | - | Dose-limiting neurotoxicity [33] |
| Taxanes | Tubulin (taxane site) [33] | Solid tumors (clinical) [33] | Under investigation [31] | Limited by neurotoxicity [33] |
Table 2: Advanced Cytoskeletal-Targeting Modalities in Development
| Therapeutic Approach | Mechanism | Therapeutic Indications | Advantages | Status |
|---|---|---|---|---|
| Antibody-Drug Conjugates (e.g., T-DM1) [32] | Antibody-targeted delivery of maytansinoid DM1 | HER2+ breast cancer [32] | Targeted delivery, reduced systemic toxicity | FDA-approved [32] |
| PROTACs targeting CDKs [36] | Targeted protein degradation of cell cycle regulators | Various cancers [36] | Overcomes resistance, catalytic action | Preclinical/clinical development [36] |
| MARK4 Inhibitors [35] | Inhibition of tau hyperphosphorylation | Alzheimer's disease [35] | Addresses specific neurodegenerative mechanism | Preclinical identification [35] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Cytoskeletal Drug Target Screening
| Reagent / Resource | Function/Application | Specific Examples |
|---|---|---|
| Cell Lines with Differential Sensitivity | Identifying compounds that overcome resistance | BT-12 (chemosensitive) vs. BT-16 (chemoresistant) AT/RT cells [30] |
| 3D Spheroid Culture Systems | Mimicking solid tumor architecture and drug resistance | Layered spheroids with proliferative, quiescent, and necrotic zones [30] |
| High-Content Imaging Systems | Quantifying cytoskeletal and morphological changes | Immunofluorescence analysis of microtubule, actin organization [32] [33] |
| Tubulin Polymerization Assays | Direct assessment of microtubule dynamics | In vitro turbidimetric measurements of microtubule formation [32] |
| OATP Transporter Models | Evaluating cellular uptake mechanisms | OATP1B1/1B3 (hepatic), OATP1A2 (BBB) transporters for MC-LR uptake [37] |
Experimental Workflows and Signaling Pathways
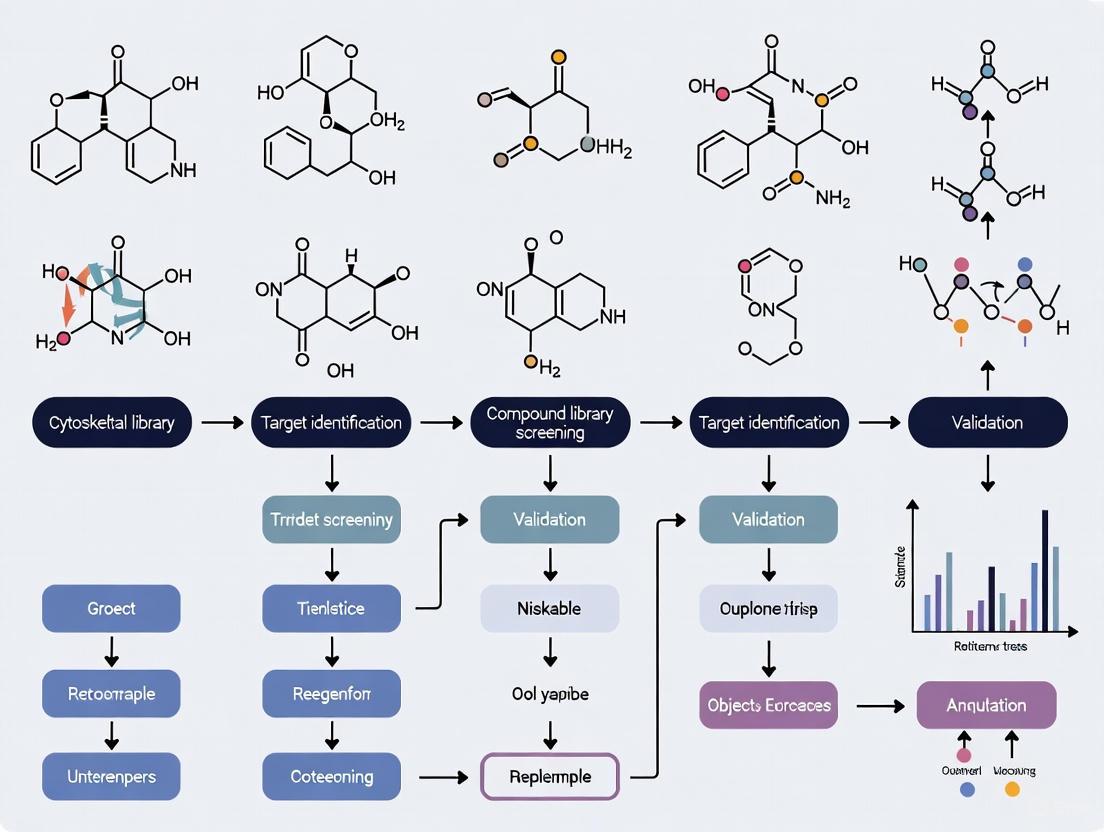
Diagram 1: High-Throughput Screening Workflow for Cytoskeletal-Targeting Compounds. This diagram outlines the key stages in identifying and validating compounds that target the cytoskeleton, from initial screening through mechanistic validation [30].
Diagram 2: Cytoskeletal Dysregulation in Neurodegeneration and Therapeutic Targeting. This pathway illustrates how cytoskeletal stressors lead to neuronal dysfunction and identifies key intervention points for cytoskeletal-targeting therapies [38] [35].
Screening Technologies and Assay Platforms: From Biochemical to Complex Physiological Systems
What is the fundamental principle behind an in vitro tubulin polymerization assay? The assay is an economical and convenient extracellular method that monitors the polymerization of tubulin into microtubules over time under controlled conditions. As tubulin polymerizes, the increasing mass of microtubules in solution changes its optical properties. This change can be measured either by an increase in turbidity (absorbance) or by an increase in the fluorescence of a reporter dye that incorporates into the growing microtubule structures. The resulting polymerization curve allows researchers to qualitatively judge compound binding and quantitatively analyze inhibitory or promotive activity on tubulin polymerization [39].
How is this assay used in drug discovery? In vitro tubulin polymerization is a primary screen for identifying and characterizing Microtubule Targeting Agents (MTAs). It confirms whether a compound directly affects tubulin and determines its mode of action—stabilizing/polymerizing or destabilizing/depolymerizing [40]. The assay is crucial for determining half-maximal effective or inhibitory concentration values (EC₅₀/IC₅₀) and for establishing structure-activity relationships (SAR) during lead compound optimization [39] [41].
Detailed Experimental Protocols
Fluorescence-Based Protocol
This protocol uses a commercially available kit (e.g., Cytoskeleton, Inc. BK011P) and is designed for high-throughput screening [42].
- Principle: A fluorescent reporter dye binds to tubulin and emits a strong signal upon incorporation into the microtubule polymer. Fluorescence intensity increases as polymerization proceeds [42].
- Materials:
- Purified tubulin (>99% pure)
- Tubulin buffer with a fluorescent reporter
- GTP (Guanosine triphosphate)
- Tubulin glycerol buffer
- Control compounds (e.g., Paclitaxel, Vinblastine)
- Half-area 96-well or 384-well black, flat-bottom microtiter plates
- Step-by-Step Procedure:
- Reconstitution: Prepare all reagents according to the kit's datasheet, keeping them on ice.
- Reaction Setup: In a well, combine tubulin protein, fluorescent reporter, and GTP in the appropriate tubulin polymerization buffer. The typical final volume is 50 µL for a 96-well format or 10 µL for a 384-well format.
- Compound Addition: Add the test compound to the reaction mix. Include controls: a no-compound control, a polymerization enhancer control (e.g., paclitaxel), and a polymerization inhibitor control (e.g., vinblastine).
- Data Acquisition: Immediately transfer the plate to a temperature-controlled fluorimeter pre-heated to 37°C. Record the fluorescence intensity (Ex: 360 nm / Em: 420 nm) every minute for 60-90 minutes.
- Data Analysis: Plot fluorescence versus time to generate polymerization curves for each condition.
Absorbance (Turbidity)-Based Protocol
- Principle: Polymerization of tubulin into microtubules increases the turbidity of the solution, which can be measured as an increase in optical density (OD) [39].
- Materials:
- Purified tubulin (often from mammalian brain)
- MES or PEM buffer system
- GTP
- Glycerol (often used at 15-20% to promote polymerization)
- Clear 96-well plates
- Step-by-Step Procedure:
- Sample Preparation: Prepare tubulin in a glycerol-containing polymerization buffer (e.g., MES buffer with 15% glycerol) and keep it on ice [39] [42].
- Reaction Setup: Pipette the tubulin solution into a well. Add test compound or vehicle control.
- Data Acquisition: Transfer the plate to a temperature-controlled plate reader at 37°C. Monitor the absorbance at 350 nm (A350) every minute for 60-90 minutes [39].
- Data Analysis: Plot OD350 versus time. The slope of the curve indicates the rate of polymerization, and the plateau indicates the total mass of polymer formed.
The following diagram illustrates the workflow common to both types of assays.
Quantitative Data and Assay Performance
The table below summarizes key performance characteristics for a standard fluorescence-based tubulin polymerization assay [42].
Table 1: Standard Assay Performance Metrics for a Fluorescence-Based Tubulin Polymerization Assay
| Parameter | Specification / Value | Notes / Context |
|---|---|---|
| Detection Method | Fluorescence (360 nm Ex / 420 nm Em) | |
| Tubulin Purity | >99% | Essential for reliable, reproducible results [42]. |
| Assay Throughput | 96-well or 384-well format | 50 µL (96-well) or 10 µL (384-well) reaction volume [42]. |
| Key Control EC₅₀/IC₅₀ | Paclitaxel EC₅₀: 0.49 µMVinblastine IC₅₀: 0.6 µM | Under standard kit conditions [42]. |
| Assay Variability | Coefficient of Variation (CV): ~11% | Indicates good reproducibility [42]. |
Troubleshooting Common Experimental Issues
We observe a low signal-to-noise ratio or a flat polymerization curve in both control and test samples. What could be wrong? This is typically caused by loss of tubulin activity.
- Cause 1: Improper handling or storage. Tubulin is a labile protein. Always keep it on ice and use glycerol-containing buffers for stability. Avoid multiple freeze-thaw cycles [39].
- Solution: Use fresh, high-purity tubulin. Confirm that positive controls (e.g., paclitaxel) are working. If they fail, the tubulin lot is likely compromised.
- Cause 2: Inaccurate temperature control. Polymerization is highly temperature-sensitive and requires a precise and rapid shift to 37°C [39].
- Solution: Pre-heat the fluorimeter or plate reader to 37°C and ensure the plate equilibrates quickly. Verify the instrument's temperature calibration.
The positive control (e.g., Paclitaxel) works, but our test compound shows high variability between replicates. This often points to issues with compound solubility and preparation.
- Cause: Many discovery compounds are dissolved in DMSO, which can affect tubulin dynamics at high concentrations. Precipitation can lead to inconsistent exposure.
- Solution: Ensure the final concentration of DMSO is consistent and low (typically ≤1%) across all samples, including controls. Centrifuge compound stocks to remove insoluble particles before use.
The shape of our polymerization curve is abnormal, with a sudden drop in signal mid-experiment. This suggests microtubule instability after formation.
- Cause: Physical disturbance of the plate or temperature fluctuations during the reading phase can cause microtubules to depolymerize.
- Solution: Ensure the plate reader is in a stable location, free from vibrations. Confirm that the temperature is maintained consistently at 37°C throughout the entire run.
We get different results when testing the same compound in cell-based assays. Why? This is a common disconnect between in vitro and cell-based readouts.
- Cause 1: The compound may not be cell-permeable.
- Cause 2: The compound might be metabolized or sequestered in the cellular environment.
- Cause 3: Cellular factors, such as Microtubule-Associated Proteins (MAPs) or different tubulin isotypes, can modulate the compound's effect [41]. A positive in vitro result confirms the compound can target pure tubulin, suggesting follow-up live-cell imaging experiments are needed [40].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents and Materials for Tubulin Polymerization Assays
| Reagent / Material | Function / Role in the Assay |
|---|---|
| Purified Tubulin | The core substrate of the assay. High purity (>99%) is critical for reliable results and is typically purified from mammalian brain or recombinant sources [42] [40]. |
| Nucleotides (GTP) | Provides the energy source necessary for the polymerization reaction. It is an essential component of the polymerization buffer. |
| Paclitaxel (Taxol) | Microtubule-stabilizing control compound. Used as a positive control to promote polymerization and validate assay performance [39] [42]. |
| Vinblastine / Colchicine | Microtubule-destabilizing control compounds. Used as positive controls to inhibit polymerization. They bind to distinct sites on tubulin (vinca and colchicine sites, respectively) [42] [43]. |
| Fluorescent Reporter Dye | A dye that exhibits enhanced fluorescence upon binding to polymerized microtubules, enabling real-time, quantitative tracking of polymerization in fluorescence-based assays [42]. |
| Glycerol | A common component of polymerization buffers that promotes and stabilizes microtubule formation by reducing the critical concentration of tubulin required for polymerization [39] [42]. |
Advanced Techniques and Emerging Methods
Are there more advanced methods to study compound effects on tubulin? Yes, beyond standard fluorescence and absorbance assays, several advanced techniques provide deeper mechanistic insights.
- Nano-Differential Scanning Fluorimetry (nanoDSF): This innovative label-free method monitors the intrinsic fluorescence of tubulin's tryptophan residues during a temperature ramp. It provides a dual readout: it can detect compound binding through tubulin thermostabilization (change in melting temperature, Tm) and simultaneously determine the compound's functional effect on the apparent polymerization temperature (Tpoly). This makes it highly valuable for discriminating between different mechanisms of action [41].
- Mechanistic Binding Site Competition Assays: These assays determine if a novel compound binds to a known site (e.g., taxane, vinca, or colchicine sites). They involve measuring the polymerization kinetics of tubulin in the presence of both the novel compound and a well-characterized site-specific inhibitor. If the novel compound's effect is abolished, it likely binds to the same site [40].
- Live-Cell Imaging: Following in vitro confirmation, this technique validates that the compound engages its target in a physiologically relevant context, disrupting the microtubule cytoskeleton and causing phenotypic changes like cell cycle arrest in G2/M phase [40] [43].
Mechanistic Binding Site Competition Assays
Frequently Asked Questions (FAQs)
1. What is the core principle of a competitive binding assay? A competitive binding assay measures how an unlabeled analyte (like a drug candidate) competes with a labeled reagent for a limited number of binding sites on a target protein. The core principle is that the amount of labeled analyte bound to the target is inversely proportional to the concentration of the competing unlabeled analyte. When the concentrations of the antibody and labeled analyte are constant, the bound labeled analyte decreases as the concentration of the competitive, unlabeled analyte increases [44].
2. Why would my assay show high background signal or poor curve fit? High background or poor data fitting in assays like Differential Scanning Fluorimetry (DSF) can often be traced to compound-related issues. Common culprits include intrinsic fluorescence of the test compound, interactions between the compound and the fluorescent dye, or poor compound solubility leading to aggregation. These factors can produce irregular melt curves that are difficult to interpret [45].
3. My compound shows binding in a biochemical assay but not in a cellular one. What could be wrong? A positive result in a biochemical assay (e.g., using purified protein) that fails to translate to a cellular assay (like CETSA) often points to a cell membrane permeability issue. The test compound must efficiently cross the cell membrane to bind its intracellular target. If the compound cannot enter the cell, no stabilization or destabilization of the target protein will be observed, despite confirmed binding in a cell-free system [45].
4. How do I calculate the binding affinity (Ki) of my unlabeled compound? The inhibitory constant (Ki) for an unlabeled ligand is not measured directly but is calculated from a competition experiment. First, you must determine the dissociation constant (Kd) between your target and a fluorescently labeled competitor. Then, you titrate your unlabeled ligand against a pre-formed complex of the target and the labeled competitor to determine the EC50 (the concentration that displaces 50% of the labeled ligand). The Ki can then be calculated using the Cheng-Prusoff equation: Ki = EC50 / (1 + [C]t / Kd,C + [T]t / Kd,T), where [C]t and [T]t are the total concentrations of the labeled competitor and target, respectively [46].
5. What are the major advantages of label-free binding assays? Techniques like Thermal Shift Assays (TSAs) and Drug Affinity Responsive Target Stability (DARTS) are label-free, meaning neither the drug compound nor the target protein needs to be modified with a fluorescent or radioactive tag. This avoids the risk of the label altering the binding characteristics of the molecule. DARTS, for example, is cost-effective, can be applied to unmodified small molecules, and does not require large quantities of pure protein [45] [47].
Troubleshooting Guide
Table 1: Common Experimental Issues and Solutions
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Irregular or noisy melt curves (DSF) | Compound-dye interactions; compound autofluorescence [45]. | Test compound intrinsic fluorescence beforehand; use a control with compound and dye only [45]. |
| No thermal shift observed | No binding; incorrect buffer conditions; protein already aggregated [45]. | Ensure protein is stable and soluble in chosen buffer; include a positive control ligand [45]. |
| Low signal in competition assays | Insufficient complex formation; labeled ligand concentration too high [46]. | Use target concentration ~1-2x its Kd with the labeled competitor; keep labeled ligand concentration at or below its Kd [46]. |
| High variability between replicates | Protein aggregation or precipitation; inconsistent sample preparation [45]. | Include low concentrations of non-ionic detergents (e.g., 0.01% Tween-20) to improve protein stability [45]. |
| Positive in lysate but not in whole cells (CETSA) | Poor cell permeability of the compound [45]. | Confirm compound permeability; use lysate-based TSAs (PTSA/DSF) as an intermediate step [45]. |
Table 2: Key Buffer and Reagent Considerations
| Parameter | Consideration | Impact on Assay |
|---|---|---|
| Buffer Composition | Additives like detergents or viscosity agents can interfere with fluorescent dyes [45]. | Can cause high background fluorescence or quenched signals [45]. |
| Protein Quality | Protein must be stable, soluble, and not pre-aggregated before the assay [45]. | Unstable protein leads to poor melt curves and unreliable Tm shifts [45]. |
| Labeled Ligand Purity | The purity and specific activity of the labeled antigen are critical for assay accuracy [44]. | Impurities can lead to inaccurate quantification and reduced sensitivity [44]. |
| Loading Control (PTSA) | Use a highly heat-stable protein like SOD1 or APP-αCTF for normalization [45]. | Ensures accurate quantification of the target protein band during densitometry [45]. |
Essential Experimental Protocols
Protocol 1: Competitive Binding Assay with Fluorescent Tracer
This protocol outlines the steps to determine the Ki of an unlabeled ligand by competing it with a fluorescently labeled molecule [46].
Step 1: Determine the Kd of the Labeled Competitor
- Setup: Prepare a titration series of the unlabeled target protein.
- Reaction: Incubate each target concentration with a constant, low concentration of the fluorescent competitor (at or below its expected Kd).
- Measurement: Use a compatible method (e.g., fluorescence anisotropy, TR-FRET) to measure the fraction of bound competitor.
- Analysis: Fit the dose-response data to the law of mass action to extract the Kd for the labeled competitor-target interaction [46].
Step 2: Competition Experiment to Determine EC50
- Setup: Prepare a titration series of the unlabeled ligand of interest.
- Reaction: In each reaction, include a constant concentration of the target (sufficient to form a complex, ~1-2x Kd from Step 1) and a constant concentration of the labeled competitor (same as in Step 1). Add the titrated unlabeled ligand.
- Measurement: Measure the signal corresponding to the bound labeled competitor. As the unlabeled ligand concentration increases, the signal will decrease.
- Analysis: Fit the resulting data with a sigmoidal dose-response curve (Hill equation) to determine the EC50 value [46].
Step 3: Calculate the Ki
Use the Cheng-Prusoff equation to calculate the Ki for your unlabeled ligand:
Ki = EC50 / (1 + [C]t / Kd,C + [T]t / Kd,T)
Where:
- EC50 is from Step 2.
- [C]t is the total concentration of the labeled competitor used in Step 2.
- Kd,C is the dissociation constant for the competitor from Step 1.
- [T]t is the total concentration of the target used in Step 2 [46].
Protocol 2: Cellular Thermal Shift Assay (CETSA)
CETSA evaluates target engagement in a more biologically relevant cellular context [45].
- Sample Preparation: Plate cells according to the desired experimental setup. Treat cells with the test compound or vehicle control for a specified time to allow for cellular uptake and target binding.
- Heating: Aliquot the cell suspensions (intact cells or cell lysates) and heat each aliquot at different temperatures (e.g., from 40°C to 65°C) for a fixed time (e.g., 3 minutes).
- Protein Quantification: Lyse the heated cells (if using intact cells) and separate the soluble protein from aggregates by centrifugation. Quantify the remaining soluble target protein in each sample using Western blot or other immunoassays.
- Data Analysis: Plot the fraction of soluble protein remaining against the temperature. Fit the data to generate melt curves. A rightward shift in the melting temperature (Tm) in the compound-treated sample indicates stabilization and direct binding of the compound to the target protein [45].
Workflow and Pathway Visualizations
Competitive Binding Principle
Competitive Binding Assay Workflow
TSA Progression in Drug Discovery
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials
| Reagent / Material | Function in Binding Site Competition Assays | Example Use-Cases |
|---|---|---|
| Purified Recombinant Protein | The target molecule for biochemical binding studies. High purity and stability are critical [45]. | DSF, PTSA, competitive binding with fluorescent tracer [45]. |
| Monoclonal Antibodies | Provide high specificity for a single epitope, essential for immunometric and detection assays [44]. | Western blot detection in CETSA/PTSA; engineered polyclonal mixtures for complex targets [44] [45]. |
| Polarity-Sensitive Dyes (e.g., SyproOrange) | Bind hydrophobic patches exposed upon protein unfolding; core detection reagent in DSF [45]. | High-throughput screening of compound libraries using DSF [45]. |
| Fluorescently Labeled Ligands | Serve as the competing tracer molecule in fluorescence-based competitive binding assays [46]. | Determining Kd and EC50 values for Ki calculations [46]. |
| Heat-Stable Loading Control Proteins (e.g., SOD1) | Used for normalization in PTSA to account for sample-to-sample variation [45]. | Ensuring accurate quantification of target protein bands in gel-based thermal shift assays [45]. |
| Cytoskeletal Target Proteins | Specific proteins relevant to cytoskeletal research for specialized screening [48]. | Tubulin polymerization assays; kinesin ATPase assays; myosin activity screens [48]. |
Cell Painting is a high-content, image-based morphological profiling assay that utilizes multiplexed fluorescent dyes to comprehensively characterize cell state in an unbiased manner. By simultaneously labeling multiple cellular components, it generates rich, quantitative data describing cellular morphology, enabling researchers to detect subtle phenotypic changes resulting from genetic or chemical perturbations [49] [50]. This technique is particularly powerful for cytoskeletal drug target compound screening, as it can capture complex phenotypic signatures induced by compounds affecting tubulin, actin, myosin, and other cytoskeletal targets, providing insights into their mechanism of action (MoA) without prior knowledge of the specific target [48] [51] [52].
The assay employs six fluorescent dyes imaged in five channels to reveal eight broadly relevant cellular components: the nucleus, nucleoli, cytoplasmic RNA, the endoplasmic reticulum, mitochondria, the Golgi apparatus, the actin cytoskeleton, and the plasma membrane [49] [53] [50]. Automated image analysis software then identifies individual cells and extracts ~1,500 morphological features (measuring size, shape, texture, intensity, and spatial relationships) to create a morphological "fingerprint" or profile for each treated cell population [49] [50] [54]. These profiles can be compared to suit various goals in drug discovery, including identifying the phenotypic impact of chemical perturbations, grouping compounds into functional pathways based on biosimilarity, and identifying signatures of disease [49] [50] [51].
For cytoskeletal research, Cell Painting offers a distinct advantage. It can identify compounds with a shared MoA, such as cell-cycle modulation, even when they have different annotated protein targets or are structurally diverse [51] [52]. This is crucial for discovering compounds that target non-protein biomolecules or exhibit polypharmacology. Furthermore, the assay can be used to build performance-diverse small-molecule libraries for phenotypic screening, enriching for compounds that produce measurable morphological effects in a specific cell type [50].
Experimental Protocol: Implementing the Cell Painting Assay
Detailed Step-by-Step Workflow
The following diagram outlines the core workflow for a Cell Painting experiment, from cell plating to data analysis:
Protocol Duration: The entire process, from cell culture to data analysis, typically takes 2 to 4 weeks [49] [53].
Step 1: Cell Plating
- Plate cells in multiwell plates (typically 96- or 384-well format) at an appropriate confluency to ensure isolated cells for accurate segmentation [49] [54]. U-2OS cells are commonly used due to their large, flat morphology and good adherence, but the protocol can be adapted to other cell lines [51].
- Critical Consideration: Include appropriate controls (e.g., vehicle controls, positive control compounds) and account for potential edge effects in the plates [49].
Step 2: Treatment/Perturbation
- Perturb cells with the treatments to be tested (e.g., small molecules from a cytoskeleton-focused library [52]) for a desired duration, often 24-48 hours [49] [54]. A typical concentration range includes multiple doses (e.g., 2 μM, 10 μM) to assess phenotypic concentration dependence [51].
Step 3: Staining and Fixation
- After treatment, cells are fixed, permeabilized, and stained with the multiplexed dye set. The original and updated Cell Painting protocols specify the following stains [49] [53]:
- Hoechst 33342: Labels DNA in the nucleus.
- Concanavalin A conjugated to Alexa Fluor 488: Labels the endoplasmic reticulum.
- Wheat Germ Agglutinin (WGA) conjugated to Alexa Fluor 555: Labels the plasma membrane and Golgi apparatus.
- Phalloidin conjugated to Alexa Fluor 555 or 568: Labels filamentous actin (F-actin).
- SYTO 14 green fluorescent RNA stain: Labels nucleoli and cytoplasmic RNA.
- MitoTracker Deep Red: Labels mitochondria.
- Protocol Update (Cell Painting v3): Recent optimizations have shown that concentrations for some stains (e.g., Phalloidin, WGA, Concanavalin A) can be reduced without compromising data quality, lowering assay cost [53].
Step 4: Image Acquisition
- Image the stained plates on a high-throughput or high-content screening (HCS) microscope capable of automated imaging in five fluorescence channels [49] [54].
- Acquire multiple fields per well to ensure a statistically significant number of cells are captured for analysis.
Step 5: Image Analysis and Feature Extraction
- Use automated image analysis software (e.g., CellProfiler [49] [53], Cellpose [53]) to identify individual cells and their subcellular compartments.
- The software extracts ~1,500 morphological features per cell, quantifying various aspects of size, shape, texture, intensity, and spatial correlations between channels [49] [50] [54].
Step 6: Data Analysis and Profiling
- Generate population-level morphological profiles from the single-cell data.
- Use data processing tools (e.g., Pycytominer [53]) and clustering algorithms to compare profiles across different perturbations. Compounds or genes with similar morphological impacts will cluster together, suggesting a shared MoA [50] [51].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details the essential reagents and materials required to perform a Cell Painting assay.
Table 1: Essential Reagents for the Cell Painting Assay
| Item | Function in the Assay | Examples & Notes |
|---|---|---|
| Fluorescent Dyes | Multiplexed staining of 8 cellular components. | Hoechst 33342 (DNA), Phalloidin (F-actin), WGA (Golgi/PM), ConA (ER), MitoTracker (Mitochondria), SYTO 14 (RNA) [49] [53] [54]. |
| Cell Painting Kit | Pre-optimized reagent set for convenience. | Image-iT Cell Painting Kit (Thermo Fisher) provides all dyes in pre-measured amounts [54]. |
| High-Content Imaging System | Automated image acquisition of multi-well plates. | Systems like the CellInsight CX7 LZR Pro are designed for high-throughput fluorescence imaging [54]. |
| Image Analysis Software | Cell segmentation and feature extraction. | CellProfiler [49] [53] is an open-source standard; Cellpose [53] is a powerful alternative. |
| Data Analysis Tools | Processing and clustering morphological profiles. | Pycytominer [53] for data normalization and aggregation; KNIME [53] for workflow integration. |
Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
Q1: How can Cell Painting specifically benefit cytoskeletal drug discovery? Cell Painting is exceptionally well-suited for cytoskeletal research because it directly visualizes and quantifies changes in cellular structures. It can group compounds based on their phenotypic impact, identifying novel microtubule, actin, or myosin regulators even without prior target knowledge [51] [52]. For instance, it can cluster iron chelators with S/G2 phase cell-cycle regulators based on their shared morphological fingerprint, revealing a common MoA rooted in impaired cell division [51].
Q2: What is the difference between a "mode of action" (MoA) and a "target" in morphological profiling? Morphological profiling primarily identifies Mode of Action (MoA)—the functional, often physiological, change induced in the cell (e.g., cell-cycle arrest, disruption of protein synthesis) [51]. The specific protein target (e.g., KIF18A, tubulin) is often inferred by clustering with well-annotated reference compounds whose targets are known. The assay is powerful because compounds with different annotated targets can share an MoA and thus cluster together [48] [51].
Q3: My positive control compounds are not clustering together as expected. What could be wrong? This indicates an issue with assay robustness. Key areas to check include:
- Cell Culture Health: Ensure consistent passage number and confluency.
- Staining Consistency: Verify dye concentrations, incubation times, and that reagents have not degraded.
- Image Acquisition: Confirm that imaging settings (exposure time, laser power) are consistent across plates and runs.
- Data Normalization: Apply appropriate normalization and batch correction methods to minimize technical variability [49] [53].
Troubleshooting Guide: Staining and Image Artifacts
This guide addresses common experimental problems encountered during the Cell Painting assay.
Table 2: Troubleshooting Common Cell Painting Issues
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Weak or No Staining | Inactive dyes; insufficient dye concentration; over-fixation; incomplete permeabilization. | Use fresh dye aliquots; titrate dyes to optimize concentration [53]; validate staining protocol with a positive control [55]. |
| High Background Fluorescence | Non-specific antibody binding; insufficient washing; endogenous enzymes or biotin. | Optimize dye concentration to reduce non-specific binding [56] [55]; increase number and volume of wash steps; for IHC-detection, use peroxidase blocking solution [56]. |
| Uneven Staining Across Wells | Inconsistent reagent coverage during incubation; plates not level; edge effects. | Use a humidified chamber to prevent evaporation; ensure plates are level during incubations; use specialized plates that minimize edge effects [49] [55]. |
| Autofluorescence | Inherent tissue properties; aldehyde-based fixatives. | For fluorescent detection, use fluorophores in the near-infrared range (e.g., Alexa Fluor 647) [56]; treat samples with autofluorescence quenchers like Sudan Black [56] [55]. |
| Poor Cell Segmentation | Over-confluent cells; low signal-to-noise; incorrect focus during imaging. | Plate cells at lower density; optimize staining and exposure to improve contrast; check image focus and acquisition settings [49] [53]. |
Case Study: Application in Cytoskeletal Compound Screening
A compelling application of Cell Painting in cytoskeletal research is its use in identifying a common MoA for diverse compounds. A 2020 study used the assay to profile the iron chelator deferoxamine (DFO) [51]. The morphological fingerprint of DFO was used as a query to screen a library of 3,580 reference compounds.
- Results: The assay successfully identified known metal chelators (ciclopirox, 1,10-phenanthroline) with high biosimilarity (>90%) to DFO. Furthermore, it revealed high biosimilarity to over 20 additional compounds with diverse annotated targets, including nucleoside analogues, CDK inhibitors, and PARP inhibitors [51].
- MoA Insight: Clustering analysis revealed that the shared MoA among these seemingly disparate compounds was cell-cycle modulation in the S or G2 phase. This is a known physiological consequence of iron depletion, as iron is a cofactor for enzymes essential for DNA synthesis [51]. This case demonstrates how Cell Painting can connect compounds with different targets into a functionally relevant cluster based on a shared phenotypic outcome.
The following diagram illustrates the logical process of this mechanism of action discovery:
Frequently Asked Questions (FAQs) on Organoid Technology
General Organoid Concepts
Q1: What are organoids and how do they differ from traditional 2D cell cultures? Organoids are complex, multicellular three-dimensional (3D) in vitro cell models that closely mimic in vivo organs. Unlike two-dimensional (2D) cultures grown on flat plastic surfaces, organoids are typically derived from stem cells or tissue-specific progenitors and are cultured within a supportive extracellular matrix (ECM). This 3D architecture allows them to self-organize and recapitulate the structural and functional complexity of human tissue more faithfully than is possible in 2D systems, which often lose critical cell-to-cell and cell-to-matrix interactions [57] [58] [59].
Q2: What is the difference between an organoid and a spheroid? While both are 3D models, organoids and spheroids have distinct origins and characteristics. Organoids are derived from stem cells or isolated from primary tissue and contain multiple cell types with complex structures, can have an unlimited lifespan in culture, and are considered phenotypically stable with high physiological relevance. Spheroids, in contrast, are usually formed from single cells derived from immortalized cell lines, contain a single cell type, develop simple structures, and have a limited lifespan as physiologically-relevant models due to the formation of nutrient and hypoxic gradients [57].
Table 1: Key Differences Between Organoids and Spheroids
| Feature | Organoids | Spheroids |
|---|---|---|
| Origin | Stem cells or primary tissue [57] | Immortalized cell lines [57] |
| Cellular Complexity | Multiple cell types [57] | Usually a single cell type [57] |
| Structure | Complex, mimicking organ architecture [57] | Simple, spherical aggregates [57] |
| Lifespan in Culture | Can be expanded indefinitely [57] | Limited [57] |
| Physiological Relevance | High [57] | Lower due to internal gradients [57] |
Q3: How are organoids generated and cultured? Organoids can be derived from two main sources: adult tissue (termed Patient-Derived Organoids or PDOs) or pluripotent stem cells (PSCs) [57]. A critical step is the isolation and expansion of the stem cell population. Once isolated, organoids are cultured embedded in a rich extracellular matrix (ECM) hydrogel, such as Growth Factor Reduced (GFR) Matrigel, and fed with a specialized, serum-free medium. This medium is uniquely formulated for each organoid type and contains a mix of growth factors and supplements (e.g., Wnts, R-spondin, Noggin, EGF) essential for growth and maintenance. Media is replenished every other day, and organoids are typically passaged once per week to prevent necrosis [57].
Q4: Can organoids be cryopreserved for long-term storage? Yes, most patient-derived organoid types can be cryopreserved using optimized freezing media. It is recommended to pre-treat organoids with a RHO-associated kinase (ROCK) inhibitor (Y27632) before freezing to promote cell viability. A common protocol involves freezing the contents of 5-10 Matrigel domes into one cryovial using a controlled-rate freezing container [57].
Organoids in Drug Screening & Cytoskeletal Research
Q5: Why are organoids particularly valuable for cytoskeletal drug target screening? The cytoskeleton, comprising microtubules, microfilaments, and intermediate filaments, is a validated target for cancer therapy, with drugs like taxanes and vinca alkaloids acting on tubulin [11] [52]. Organoids offer a superior model for testing such compounds because they:
- Retain Patient-specific Heterogeneity: Tumor PDOs retain key genetic and phenotypic characteristics of their tissue of origin, including the expression of specific tubulin isotypes which can influence drug response [60] [11].
- Enable Phenotypic Screening: High-content imaging (HCI) of 3D organoids allows for the multiplexed measurement of phenotypic endpoints relevant to cytoskeletal function, such as organoid morphology, nucleus size and shape, and evidence of apoptosis, providing deep insights into a compound's mechanism of action [58] [61].
- Model Complex Biology: They more closely replicate the in vivo environment where cytoskeleton-based processes like cell division, migration, and intracellular transport occur, leading to more clinically predictive data than 2D models [58] [59].
Q6: What specialized assays are used with organoids in drug screening? Due to their 3D nature, traditional assays often require optimization for use with organoids. Common and specialized assays include:
- Viability/Cytotoxicity Assays: Optimized live/dead cell viability assays using stains like calcein-AM (live), propidium iodide (dead), and Hoechst 33342 (all cells) [57].
- High-Content Imaging (HCI) and Analysis (HCA): These technologies use multiplexing to monitor multiple endpoints simultaneously, including nucleus count/size/volume, necrosis/apoptosis markers, epithelium thickness, and polarity [58].
- Functional Assays: Specialized assays like the forskolin-induced organoid swelling assay to measure CFTR function serve as examples of how organoids can model specific physiological functions [57].
Q7: How can screening data from organoids be used for biomarker discovery? Screening a diverse panel of patient-derived organoids with a compound generates valuable data on both responders and non-responders. By combining this pharmacological data with the organoids' genomic (e.g., Whole Exome Sequencing), transcriptomic (e.g., RNA-Seq), and proteomic profiles, researchers can correlate drug sensitivity with specific molecular features. This integrated approach is instrumental for identifying biomarkers that can predict patient response and stratify patients in clinical trials [58]. For robust discovery, it is recommended to have at least 10 sensitive and 10 insensitive models with a sufficient spread in efficacy (e.g., a 10-fold difference in IC50 values) [58].
Troubleshooting Common Experimental Challenges
Low Cell Viability & Organoid Formation
Table 2: Troubleshooting Guide for Organoid Culture
| Problem | Potential Cause | Solution |
|---|---|---|
| Low cell viability after tissue dissociation [60] | Excessive enzymatic or mechanical digestion. | Optimize digestion time and temperature; use gentler pipetting; include a ROCK inhibitor (Y27632) in the medium during and after passaging [57]. |
| Failure to form organoids | Incorrect matrix or poor-quality reagents. | Use a high-quality, lot-qualified hydrogel (e.g., GFR Matrigel); ensure growth factors in the medium are active and the formulation is correct for the specific organoid type [57]. |
| Necrotic centers in organoids [57] | Organoids have grown too large, limiting nutrient diffusion. | Adhere to a strict passaging schedule (typically once per week); mechanically shear organoids into appropriately sized fragments during sub-culture [57]. |
| Microbial contamination | Non-sterile technique during tissue collection or processing. | Supplement transport and wash media with antibiotics (e.g., penicillin-streptomycin); process tissues promptly or use validated cryopreservation methods for storage [60]. |
Challenges in High-Throughput Screening (HTS)
Inconsistent Seeding in 384-Well Plates:
- Challenge: Variability in organoid fragment number and size per well leads to poor assay reproducibility.
- Solution: Use standardized mechanical shearing to create fragments of a consistent size (e.g., 5-20 cells per structure). Employ advanced liquid handling robotics to seed a precise number of fragments per well (e.g., ~300 fragments per well in a 384-well plate) [58]. Using cryopreserved "assay-ready" organoids can also improve consistency and throughput [58].
Difficulty Distinguishing Cytostatic vs. Cytotoxic Effects:
- Challenge: Traditional "bulk" assays like ATP quantification measure overall viability but cannot differentiate between growth inhibition (cytostatic) and cell death (cytotoxic).
- Solution: Implement high-content, label-free live-cell imaging platforms. These systems use AI-driven image analysis to track the growth or death of individual organoids over time, allowing for accurate calculation of metrics like the Normalized Organoid Growth Rate (NOGR), which can separate cytostatic from cytotoxic responses [62].
Experimental Protocols
Protocol 1: Establishing a Patient-Derived Colorectal Organoid Biobank
This protocol is adapted from current methodologies for generating organoids from normal crypts, polyps, and tumors [60].
1. Tissue Procurement and Initial Processing (Timing: ~2 hours)
- Collect human colorectal tissue samples under sterile conditions immediately after colonoscopy or surgical resection, following IRB-approved protocols and informed consent.
- CRITICAL STEP: Transfer samples in a 15 mL tube containing 5–10 mL of cold Advanced DMEM/F12 medium supplemented with antibiotics to prevent contamination. Process promptly to maintain cell viability.
- For short-term storage (≤6–10 hours): Wash tissues with antibiotic solution and store at 4°C in DMEM/F12 with antibiotics.
- For longer delays (>14 hours): Cryopreserve the tissue after an antibiotic wash using a freezing medium (e.g., 10% FBS, 10% DMSO in 50% L-WRN conditioned medium) [60].
2. Tissue Dissociation and Crypt Isolation
- Mechanically dissociate the tissue using a scalpel or scissors, followed by gentle pipetting or brief enzymatic digestion to liberate intact crypts.
- Filter the cell suspension through a strainer (e.g., 100μm) to remove large debris and collect crypts.
3. Culture Establishment
- Resuspend the isolated crypts in a chilled, undiluted extracellular matrix (e.g., GFR Matrigel, ~8 mg/ml or higher).
- Plate the mixture as small domes (e.g., 30-50 μL drops) in a pre-warmed culture plate and allow the matrix to polymerize at 37°C for 20-30 minutes.
- Carefully overlay the domes with organoid-specific complete medium, supplemented with essential factors like EGF, Noggin, R-spondin-1, and a ROCK inhibitor for the first few days to enhance survival.
- Refresh the medium every 2-3 days.
4. Passaging and Expansion
- Once organoids are large and dense (typically after 7-12 days), passage them. Remove the medium, disrupt the Matrigel dome with cold PBS, and collect the organoids.
- Mechanically dissociate the organoids into small fragments using a pipette or enzyme-free dissociation reagents.
- Re-embed the fragments in fresh Matrigel and continue culture with a split ratio of roughly 1:3 to 1:4 [57].
Diagram 1: Workflow for establishing patient-derived colorectal organoids.
Protocol 2: High-Throughput Phenotypic Drug Screening on Organoids
This protocol outlines the process for screening compound libraries against organoid panels [58] [61] [62].
1. Pre-screen Preparation: 'Assay-Ready' Organoids
- Culture and expand the desired organoid lines (e.g., a panel of colorectal cancer PDOs).
- At the appropriate confluency, harvest and dissociate organoids into small fragments.
- Cryopreserve the fragments as "assay-ready" aliquots to ensure a consistent and readily available supply for screening campaigns [58].
2. Assay Plate Seeding
- Thaw "assay-ready" organoids or use freshly prepared fragments.
- Using automated liquid handling robotics, seed organoid fragments into 384-well plates pre-coated with a thin layer of ECM. Seed approximately 300 fragments (5-20 cells per structure) per well, though this number should be optimized for each organoid type and assay duration [58] [62].
- CRITICAL STEP: Allow organoids to recover and form compact 3D structures for 1-3 days before compound addition.
3. Compound Treatment and Incubation
- Prepare compound plates with your library of interest. Include controls (e.g., DMSO vehicle, reference cytotoxic compounds).
- Using a robotic liquid handler, transfer compounds to the assay plates containing organoids.
- Incubate the plates for the desired duration (typically 5-7 days) to observe compound effects [58].
4. Endpoint Readout and Analysis
- For phenotypic screening, use high-content imaging systems to capture 3D images of the organoids. Label-free imaging is preferred to avoid phototoxicity [62].
- Stain with fluorescent markers if needed (e.g., Calcein-AM for viability, propidium iodide for death, antibodies for specific proteins) [57] [61].
- Use AI-driven image analysis software to extract quantitative data on multiple parameters, such as:
- Calculate dose-response curves (IC50), Area Under the Curve (AUC), and Normalized Organoid Growth Rate (NOGR) to quantify cytostatic and cytotoxic effects [58] [62].
Diagram 2: High-throughput phenotypic screening workflow for organoids.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Reagents for Organoid Culture and Cytoskeletal Screening
| Reagent Category | Specific Examples | Function |
|---|---|---|
| Extracellular Matrix (ECM) | Growth Factor Reduced (GFR) Matrigel [57] | Provides a 3D scaffold that mimics the basal membrane, essential for organoid growth and polarization. |
| Basal Medium | Advanced DMEM/F12 [57] [60] | A nutrient-rich base medium for formulating specialized organoid culture media. |
| Essential Growth Supplements | Recombinant proteins: EGF, R-spondin-1, Noggin, Wnt3a [57]. Small molecules: A-83-01, CHIR99021, SB202190 [57]. | Create a niche environment that supports stem cell maintenance and organoid growth. |
| Cryopreservation Medium | 90% FBS + 10% DMSO [60]; or commercial organoid freezing media [57] | Protects cells from ice crystal formation during the freezing and thawing process. |
| Cytoskeleton-Targeting Compound Libraries | Libraries containing Tubulin polymerizers/destabilizers, Actin modulators, Kinesin inhibitors [52] | Collections of small molecules for screening against cytoskeletal targets in phenotypic or target-based assays. |
| Cell Viability & Staining Reagents | Calcein-AM (live cells), Propidium Iodide (dead cells), Hoechst 33342 (nuclei) [57]; Antibodies for ICC/IHC [57] [60] | Enable visualization and quantification of cell viability, death, and specific protein localization in 3D structures. |
| Dissociation Reagents | Enzyme-free passaging reagents; Accutase; Trypsin [57] | Gently break down organoids into smaller fragments or single cells for passaging or seeding. |
| ROCK Inhibitor | Y-27632 (dihydrochloride) [57] | Improves cell survival after passaging, freezing, and thawing by inhibiting apoptosis. |
Imaging Mass Cytometry for Multiparametric Analysis
Frequently Asked Questions (FAQs) and Troubleshooting
This technical support resource addresses common challenges researchers encounter when applying Imaging Mass Cytometry (IMC) to cytoskeletal drug target compound screening.
Table 1: Common IMC Experimental Issues and Solutions
| Problem Category | Specific Issue | Potential Causes | Recommended Solutions |
|---|---|---|---|
| Signal Quality | High background signal [63] | - Sample-related isotopic noise (e.g., Iodine, Platinum)- Metal impurities in reagents- Non-specific antibody binding | - Use mass cytometry-certified, ultra-pure reagents [64]- Optimize plasma temperature to reduce oxides [63]- Include a blocker incubation step before staining [63] |
| Weak or absent marker signal [63] | - Low cell viability- Over-fixation damaging epitopes- Suboptimal antibody titration | - Use fresh live cells with >95% viability [63]- Titrate fixation/permeabilization reagent concentrations [63]- Determine optimal antibody concentration via titration with controls [63] | |
| Sample Preparation | Antibody staining variance [63] | - Inconsistent cell counts between samples- Degraded or improperly stored antibodies | - Standardize the total cell number per sample [63]- Use the same fresh antibody master mix and re-titrate antibodies [63] |
| Cell loss during preparation [63] | - Excessive washing steps- Low centrifuge speed or time | - Minimize the number of washing steps [63]- Slightly increase centrifuge speed and/or centrifugation time [63] | |
| Data Integrity | Poor data quality/contamination | - Trace metal contamination from non-certified plasticware- Residual chemicals from cell isolation | - Use only certified plasticware to avoid Barium contamination [64]- Verify all sample isolation reagents and protocols [64] |
Sample Handling and Shipping
Q: What are the requirements for shipping samples to a core facility?
- A: Whole blood samples must be shipped at 4°C and arrive at the facility no later than two days post-blood draw. Pre-prepared cells can be overnight shipped in a DNA intercalator at 4°C [64].
Q: How should we handle plasticware and reagents to prevent contamination?
Detailed Experimental Protocol for Cytoskeletal Drug Screening
The following methodology is adapted from a proof-of-concept study screening drug-treated breast cancer cell lines, providing a framework for cytoskeletal drug target compound screening [65].
Cell Culture and Seeding
- Cell Lines: Use authenticated, mycoplasma-tested cell lines (e.g., MCF-7, SKBR3). Culture cells in their recommended media (e.g., DMEM for MCF-7 with 0.01 mg·mL⁻¹ insulin) supplemented with 10% bovine serum and penicillin/streptomycin [65].
- Seeding: At 70-80% confluency, detach cells using trypsin/EDTA. Seed cells onto collagen I-coated chamber slides at a concentration of 0.1e6 cells per mL (0.5 mL per chamber). Grow for 48 hours at 37°C with 5% CO₂ prior to drug addition [65].
In Vitro Drug Treatment
- Compound Preparation: Dissolve compounds in 100% DMSO at stock concentrations for long-term storage. Dilute to the final working concentration in full growth media immediately before use [65].
- Dosing: Treat cells for 48 hours. Example compounds and concentrations from the literature include [65]:
- Nocodazole (0.5 µM): Microtubule depolymerization agent.
- Etoposide (10 µM): Genotoxic chemotherapeutic.
- EGF (10 ng·mL⁻¹): Growth stimulatory factor.
- Include controls with vehicle (e.g., 2% DMSO) and fresh media.
Immunostaining for IMC
- Fixation: Following drug treatment, fix live cells in the chamber slides. The specific fixative should be determined by titration to balance epitope preservation and cell structure [63].
- Antibody Panel Design: Proper pairing of antibodies to metal isotopes is critical [63].
- Considerations: Choose isotopes within the instrument's sensitive detection range. Pair high-expression markers with less sensitive isotopes and vice-versa.
- Validation: Validate all antibodies for IMC application. Determine the optimal working dilution for each antibody via titration experiments prior to the main assay [63].
- Staining: Stain the fixed cells with a mixture of metal-tagged antibodies targeting cytoskeletal and relevant signaling markers. The panel may include markers for actin filaments, microtubules, proliferation (Ki-67), and cell signaling (pHistoneH3S28, p4E-BP1) [65]. Incubate on an orbital shaker, then wash thoroughly to remove unbound antibodies.
Data Acquisition and Analysis
- Acquisition: Insert the stained slide into the Hyperion Imaging System. Select regions of interest (ROIs) for ablation. The laser ablates the tissue in 1-µm steps, and the resulting particles are analyzed by the mass cytometer [65].
- Analysis Workflow:
- Single-Cell Identification: Use a tool like CellProfiler to identify single cells and establish cellular boundaries [65].
- Data Extraction: Employ analytical platforms like histoCAT to extract single-cell quantitative information from the multiplexed images [65].
- Visualization and Interpretation: Generate t-SNE plots and heatmaps to visualize cell populations and their marker expression. Analyze changes in cytoskeletal protein expression and modification in response to drug treatments.
The workflow below summarizes the key steps in this protocol.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for IMC-based Cytoskeletal Screening
| Item | Function/Description | Application Note |
|---|---|---|
| Collagen I-coated Slides | Provides a surface for adherent cell growth for in vitro models. | Essential for culturing cells directly on the slide for drug treatment and subsequent staining [65]. |
| Metal-Tagged Antibodies | Antibodies conjugated to pure metal isotopes for target detection. | Panel design is critical. Pair high-expression markers (e.g., cytoskeletal proteins) with less sensitive isotopes [63]. |
| Cell-ID Intercalator | An iridium-based DNA intercalator for cell identification and segmentation. | Used to stain DNA, enabling the computational identification of single nuclei and cells during analysis [65] [66]. |
| F-actin Stabilization Buffer | A specialized buffer that maintains cytoskeletal protein complexes during cell lysis. | Crucial for preserving the native state of filamentous actin and other complexes during sample preparation [67]. |
| Mass Cytometry Certified Reagents | Ultra-pure buffers, salts, and plasticware certified for low metal content. | Prevents background signal and potential damage to the instrument's detector [64]. |
| Pharmacological Compounds | Small-molecule inhibitors or activators to perturb cytoskeletal dynamics. | Examples for screening: Nocodazole (microtubule destabilizer), Latrunculin A (F-actin destabilizer) [65] [67]. |
Overcoming Screening Challenges: Specificity, Translation, and Predictive Value
Addressing Toxicity and Specificity Issues in Actin-Targeted Compounds
Troubleshooting Guides & FAQs
FAQ: Overcoming Major Hurdles in Actin-Targeted Drug Development
Q1: Why are actin-targeted compounds historically considered poor clinical candidates, and how can this be overcome? Historically, direct actin-targeting compounds (e.g., phalloidin, cytochalasin D, jasplakinolide) cause unacceptable toxicity, particularly cardiotoxicity, because they do not distinguish between actin structures in cancer cells and those in essential healthy tissues like the heart and diaphragm [68]. The primary strategy to overcome this is to shift the targeting approach from actin itself to the regulatory proteins that control actin filament populations that are specific to cancer cells [69] [68]. This allows for selective disruption of tumor-specific cytoskeletal functions.
Q2: What specific targets can be used to achieve tumor-selective actin disruption? Targeting specific isoforms of actin-binding proteins that are upregulated in cancers is a promising strategy. Key targets include:
- Tropomyosin 3.1 (Tpm3.1): This isoform is highly and specifically upregulated in cancer cells and is essential for tumor cell viability. Compounds targeting Tpm3.1 disrupt the actin cytoskeleton in tumor cells while showing no adverse impact on cardiac function in models [69] [70] [68].
- Advillin (AVIL): This actin-binding protein has been identified as a novel oncogenic driver in cancers like rhabdomyosarcoma. Targeting such proteins can damage critical cell infrastructure in a cancer-specific manner [71].
Q3: How can the efficacy of low-dose, less toxic cytoskeletal drugs be enhanced? Synergistic drug combinations are a key solution. Research demonstrates that simultaneously targeting the actin cytoskeleton (e.g., with anti-Tpm3.1 compounds) and microtubules (e.g., with low-dose Vincristine) abrogates actin-mediated repair mechanisms, potentiating cytotoxicity and allowing for effective treatment at lower, less toxic doses [70].
Q4: Do different actin-stabilizing compounds have the same biological effect? No. Even structurally related stabilizers can have distinct effects. For example, miuraenamide A and jasplakinolide both stabilize actin, but they differentially regulate gene expression and interact uniquely with actin-binding proteins. Miuraenamide A specifically competes with cofilin for binding to F-actin, while jasplakinolide does not, leading to different functional outcomes [72] [73].
Troubleshooting Guide: Common Experimental Challenges
Problem: High cytotoxicity in non-malignant cell lines during screening.
- Potential Cause: The compound is broadly disrupting all actin filaments, not just cancer-specific populations.
- Solution:
- Employ phenotypic screening using isogenic cell pairs (tumor vs. non-tumor) to identify compounds with inherent selectivity [68].
- Focus on molecular targets that are differentially expressed, such as Tpm3.1 or AVIL [69] [71].
- Validate specificity by testing the compound's impact on cardiac structure and function in relevant models early in the development pipeline [69].
Problem: Inconsistent readouts in actin polymerization or depolymerization assays.
- Potential Cause: The compound may be influencing specific subsets of actin filaments or competing with specific actin-binding proteins, rather than causing global polymerization changes.
- Solution:
- Beyond standard pyrene-actin assays, use TIRF microscopy to visualize filament assembly and morphology directly [73].
- Perform competition assays with key actin-binding proteins like cofilin, gelsolin, and Arp2/3 to characterize the precise binding mode [73].
- Use FRAP (Fluorescence Recovery After Photobleaching) to analyze the compound's effect on actin filament dynamics in live cells [74].
Problem: A lead compound is effective in vitro but shows limited efficacy in vivo.
- Potential Cause: The compound's mechanism may not sufficiently engage cell death pathways or may face pharmacokinetic challenges.
- Solution:
- Investigate the link to apoptosis. Confirm that actin disruption engages the intrinsic apoptosis pathway, characterized by cytochrome c release, caspase-9 activation, and PARP cleavage [74].
- Explore synergistic combinations. Combine your actin-targeting agent with low doses of established microtubule-targeting drugs like Vincristine to enhance potency and overcome resistance [70].
- Analyze downstream signaling. Verify that the compound inhibits pro-survival pathways, such as by trapping and inactivating PKCɛ, a kinase overexpressed in many cancers [74].
Table 1: Cytotoxicity and Selectivity Profiles of Actin-Targeting Compounds
| Compound / Target | Cancer Cell Model | Effect on Viability / Proliferation (IC₅₀) | Effect on Non-Tumor Cells / Key Safety Finding | Reference |
|---|---|---|---|---|
| TR100 (anti-Tpm3.1) | Neuroblastoma, Melanoma models | Reduces tumor cell growth in vitro and in vivo | No adverse impact on cardiac structure and function | [69] |
| Miuraenamide A | HUVEC, HCT116, HepG2, HL-60, U-2OS | ~9 nM (HUVEC proliferation) | N/D (Shows specific competition with cofilin) | [73] |
| Miuraenamide A | HUVEC | ~80 nM (Cell migration) | N/D | [73] |
| Chondramide | MCF7, MDA-MB-231 | Induces apoptosis (300 nM, 48h) | MCF-10A non-tumor breast epithelial cells show resistance; linked to low PKCɛ expression | [74] |
| Anti-Tpm3.1 + Vincristine | Broad range of tumor cells | Synergistic cytotoxicity | Combination allows for effective low-dose Vincristine use | [70] |
Table 2: Transcriptional and Protein Interaction Profiles of Actin Stabilizers
| Parameter | Miuraenamide A (60 nM) | Jasplakinolide (120 nM) | Biological Implication |
|---|---|---|---|
| Genes Regulated | 779 genes | 224 genes | Different compounds induce distinct transcriptional programs, suggesting unique mechanisms beyond simple stabilization [73]. |
| Competes with Cofilin | Yes | No | Miuraenamide A specifically occludes cofilin binding, affecting actin severing and turnover differently than jasplakinolide [73]. |
| Competes with Gelsolin/Arp2/3 | No | N/D | Specificity in protein competition highlights the potential for fine-tuning actin filament function [73]. |
| Binding Site on Actin | Interacts with Tyr133, Tyr143, Phe352; shifts D-loop | Different (presumed) | Unique binding mode explains functional differences and provides a scaffold for designing specific actin binders [73]. |
Experimental Protocols
Protocol 1: FRAP (Fluorescence Recovery After Photobleaching) for Analyzing Actin Dynamics
Purpose: To quantify the dynamics of actin filament turnover in live cells upon treatment with actin-targeting compounds [74].
Methodology:
- Cell Preparation: Seed cells (e.g., MCF7 breast cancer cells) onto glass-bottom dishes and transfect with GFP-tagged β-actin.
- Treatment: Incubate cells with the compound of interest (e.g., 300 nM Chondramide) for a predetermined time (e.g., 30 minutes).
- Photobleaching: Use a confocal microscope with a laser (e.g., 488 nm) to bleach a defined region of interest (ROI) within a cell's actin network.
- Image Acquisition: Acquire time-lapse images immediately after bleaching at short intervals (e.g., every few seconds) to monitor fluorescence recovery.
- Data Analysis: Quantify the fluorescence intensity within the bleached ROI over time. Plot the recovery curve and calculate the half-time of recovery (t₁/₂) and mobile fraction. A decrease in recovery rate indicates inhibited actin dynamics.
Protocol 2: F-actin / Cofilin Competition Binding Assay
Purpose: To determine if a compound competes with the actin-binding protein cofilin for binding to F-actin [73].
Methodology:
- Prepare F-actin: Polymerize purified G-actin into F-actin in a suitable buffer.
- Set Up Reactions: Incubate F-actin with cofilin in the presence or absence of the test compound (e.g., Miuraenamide A). Include controls with F-actin alone and cofilin alone.
- Sedimentation: Ultracentrifuge the samples to pellet F-actin and any bound proteins.
- Analysis: Separate the supernatant (unbound proteins) and pellet (F-actin and bound proteins) fractions. Analyze both fractions by SDS-PAGE and Western blotting, probing for cofilin and actin.
- Interpretation: A significant reduction of cofilin in the pellet fraction in the presence of the compound indicates competition for binding to F-actin.
Key Signaling Pathways
Diagram: Actin Stabilization-Induced Intrinsic Apoptosis Pathway
Figure 1: Actin hyper-stabilization triggers mitochondrial apoptosis. Actin-stabilizing compounds like Chondramide trap the pro-survival kinase PKCɛ within actin bundles, leading to its inactivation. This disrupts the mitochondrial VDAC/Hexokinase II (HkII) interaction and promotes the dephosphorylation and mitochondrial recruitment of the pro-apoptotic protein Bad. These events promote the Mitochondrial Permeability Transition (MPT), resulting in cytochrome c release and the activation of the intrinsic apoptosis cascade [74].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating Actin-Targeted Compounds
| Reagent / Tool | Function / Application in Research | Key Notes |
|---|---|---|
| Tropomyosin 3.1 (Tpm3.1) Inhibitors (e.g., TR100) | To selectively disrupt cancer-associated actin filament populations. | Demonstrates the feasibility of targeting actin-regulatory proteins to achieve tumor specificity with reduced toxicity [69] [70]. |
| Synergistic Microtubule Agents (e.g., Low-dose Vincristine) | To potentiate the cytotoxicity of actin-targeting compounds. | Used in combination studies to abrogate actin-mediated repair of spindle defects, enhancing anti-mitotic effects [70]. |
| Phenotypic Screening Assays (e.g., using SK-N-SH cells) | For unbiased discovery of compounds that selectively alter the actin cytoskeleton in tumor cells. | Requires cells with a highly conserved and well-organized actin cytoskeleton for a strong signal-to-noise ratio [68]. |
| Actin-Binding Protein Panel (Cofilin, Gelsolin, Arp2/3) | To characterize the precise molecular mechanism and binding mode of new actin-binding compounds. | Essential for moving beyond simple "stabilizer/destabilizer" classification, as compounds can have specific protein competition profiles [73]. |
| mt-Keima Assay | To measure mitophagy and mitochondrial damage in live cells. | Useful for connecting cytoskeletal dynamics to mitochondrial fitness, a key component in cell death and resistance mechanisms [75]. |
Mitigating Resistance to Microtubule-Targeting Agents
Troubleshooting Guides & FAQs
FAQ 1: What are the primary mechanisms by which resistance to Microtubule-Targeting Agents (MTAs) develops?
Resistance to MTAs is a significant challenge in oncology and arises through several key mechanisms. Understanding these is the first step in mitigating their effect.
- Altered Tubulin Isotype Expression: Certain cancers overexpress specific β-tubulin isotypes, particularly βIII-tubulin. This overexpression is clinically associated with resistance to taxane-based therapies (e.g., paclitaxel) in various cancers, including ovarian, non-small cell lung, and breast cancers. It alters microtubule dynamics and impairs drug binding [76].
- Multidrug Resistance (MDR) Efflux Pumps: Upregulation of membrane transport proteins, such as P-glycoprotein (P-gp), leads to increased active efflux of MTAs from cancer cells, reducing intracellular drug concentration. This is a common resistance mechanism for many chemotherapeutic agents [77] [76].
- Mutations in Tubulin Binding Sites: Point mutations in tubulin genes, especially in the taxane and vinca alkaloid binding sites, can directly interfere with the binding of MTAs, rendering them less effective [31].
- Altered Expression of Microtubule-Associated Proteins (MAPs): Changes in the cellular levels of MAPs can modulate microtubule dynamics and stability, indirectly influencing the efficacy of MTAs and promoting cell survival despite treatment [41] [31].
FAQ 2: How can we overcome resistance related to specific tubulin isotypes like βIII-tubulin?
Targeting specific tubulin isotypes that contribute to resistance is a promising strategy.
- Strategy: Develop Isotype-Specific Inhibitors. The goal is to design new MTAs that preferentially bind to the resistant isotype. For βIII-tubulin, this involves targeting its unique structural features.
- Experimental Protocol: Computational Screening for βIII-Tubulin Inhibitors.
- Target Preparation: Generate a high-quality 3D model of the human αβIII-tubulin heterodimer using homology modeling, with a structure like PDB ID 1JFF as a template [76].
- Compound Library Preparation: Curate a large library of natural or synthetic compounds in a suitable format (e.g., PDBQT) for docking. Libraries like ZINC are commonly used [76].
- High-Throughput Virtual Screening: Dock each compound from the library into the target binding site (e.g., the Taxol site on βIII-tubulin) using software such as AutoDock Vina. Rank compounds based on their predicted binding affinity [76].
- Machine Learning Refinement: Train a machine learning classifier on known active and inactive compounds to further refine the virtual screening hits and identify candidates with a high probability of activity [76].
- In Vitro Validation: The top computational hits must be validated experimentally. Key assays include:
- Tubulin Polymerization Assay: Monitor the effect of the hit compound on tubulin polymerization in real-time using methods like nanoDSF or light scattering [41] [77].
- Immunofluorescence Staining: Confirm the disruption of the cellular microtubule network in treated cancer cells using anti-tubulin antibodies and fluorescence microscopy [77].
- Anti-Proliferative Assays: Evaluate the cytotoxicity of the hit compounds against drug-sensitive and drug-resistant cancer cell lines (e.g., MTT or colony formation assays) [77].
FAQ 3: Are there specific binding sites on tubulin that are less prone to inducing resistance?
Yes, the colchicine binding site (CBS) is considered a promising target for overcoming resistance.
- Rationale: Compounds targeting the CBS are typically less susceptible to P-gp mediated efflux due to their smaller molecular size and different physicochemical properties compared to taxanes or vinca alkaloids. This provides a strategic advantage in overcoming multidrug resistance [78] [77].
- Experimental Protocol: Virtual Screening for Novel Colchicine Site Inhibitors.
- Virtual Screening Platform: Establish a screening workflow combining pharmacophore modeling, molecular docking, and interaction fingerprint similarity to filter large chemical databases (e.g., Specs) [78] [77].
- ADME/Tox Filtering: Screen the initial hits for favorable pharmacokinetic and toxicity profiles to prioritize lead compounds with a higher chance of clinical success [78].
- Binding Confirmation: Use molecular dynamics (MD) simulations to validate the stability of the compound-tubulin complex and detailed binding interactions at the colchicine site [77].
- Functional Assays: As in the previous protocol, validate the top candidates using in vitro tubulin polymerization and cellular anti-proliferative assays [78] [77].
Quantitative Data on MTA Resistance and Screening
Table 1: Key Mechanisms of Resistance to Microtubule-Targeting Agents
| Resistance Mechanism | Description | MTAs Affected | Experimental Detection Method |
|---|---|---|---|
| βIII-Tubulin Overexpression | Alters microtubule dynamics, reduces drug binding affinity. | Taxanes (Paclitaxel) [76] | qPCR, Immunoblotting, Immunohistochemistry [76] |
| P-gp Efflux Pump Upregulation | Active transport of drugs out of the cell, reducing intracellular concentration. | Taxanes, Vinca alkaloids [77] [76] | Flow cytometry with fluorescent substrates (e.g., Rhodamine 123) [77] |
| Tubulin Mutations | Point mutations in drug-binding sites (e.g., taxane site) preventing effective binding. | Taxanes, Vinca alkaloids [31] | DNA Sequencing, Molecular Docking studies [31] |
Table 2: Comparison of Screening Technologies for Novel MTAs
| Screening Technology | Key Principle | Advantages | Key Reagents/Software |
|---|---|---|---|
| nanoDSF | Monitors intrinsic protein fluorescence (Tryptophan) to detect ligand binding and its impact on tubulin polymerization & stability [41] | Label-free, dual readout (binding + polymerization), low material consumption, high sensitivity [41] | Purified tubulin, nanoDSF instrument (e.g., NanoTemper) [41] |
| Virtual Screening | Computational docking of compound libraries into a 3D tubulin structure to predict high-affinity binders [78] [76] | High-throughput, cost-effective, can target specific binding sites/isotypes [77] [76] | AutoDock Vina, InstaDock, ZINC/Specs compound libraries [78] [76] |
| Machine Learning Classification | Uses molecular descriptors of known active/inactive compounds to predict activity of new candidates [77] [76] | Can learn complex structure-activity relationships, improves hit rates [77] [76] | PaDEL-Descriptor, Scikit-learn, KNIME [76] |
Experimental Workflow Visualizations
MTA Resistance Research Workflow
Novel MTA Screening Protocol
Research Reagent Solutions
Table 3: Essential Research Tools for MTA Resistance Studies
| Reagent / Tool | Function / Application | Example Use |
|---|---|---|
| Purified Tubulin Protein | In vitro biochemical assays to study direct compound effects on tubulin polymerization. | nanoDSF assays, turbidity-based polymerization assays [41]. |
| nanoDSF Instrumentation | Label-free analysis of protein stability and ligand binding; monitors tubulin polymerization in real-time. | Detecting compound-induced shifts in tubulin polymerization temperature (T_poly) [41]. |
| P-gp Substrate (Rhodamine 123) | Fluorescent probe to assess the activity of multidrug resistance efflux pumps in cells. | Flow cytometry assays to determine if resistance is mediated by increased drug efflux [77]. |
| Virtual Screening Software (AutoDock Vina) | Predicts binding affinity and orientation of small molecules to tubulin. | High-throughput identification of potential colchicine-site or isotype-specific binders [78] [76]. |
| Molecular Dynamics Software (GROMACS) | Simulates the physical movements of atoms and molecules over time. | Validating the stability of tubulin-compound complexes and refining binding modes [77] [76]. |
Q1: Why does the source of tubulin (e.g., recombinant, tissue-purified) significantly impact drug screening assay results?
The tubulin source is critical because different purification methods and species origins result in varying compositions of tubulin isotypes and post-translational modifications (PTMs). These differences directly influence the tubulin's conformational state and dynamics. For instance, the accessibility of key structural regions, like the C-terminal tails, is regulated by the lattice conformation, which is in turn affected by the nucleotide state (GTP vs. GDP) and the presence of microtubule-associated proteins (MAPs) [79]. Assays using tubulin purified from a native source, like porcine or rat brain, will contain a natural mixture of MAPs and PTMs, whereas recombinant tubulin offers purity and consistency but may lack these regulatory components, leading to different compound binding affinities and polymerization kinetics [1] [80].
Q2: What are the primary considerations when choosing a tubulin source for a polymerization assay?
Your choice should be guided by the specific goals of your screening campaign, as detailed in the table below.
| Tubulin Source | Key Characteristics | Best Suited For | Considerations for Assay Optimization |
|---|---|---|---|
| Native Tissue (e.g., Porcine/Bovine Brain) | Contains natural isotype distribution, PTMs, and MAPs [1]. | Mechanistic studies, screening for compounds whose activity is modulated by MAPs or specific PTMs. | Buffer composition must account for endogenous GTP and MAPs. Polymerization kinetics may be more variable. |
| Native Tissue, MAP-Free | Purified from tissue (e.g., rat brain) but processed to remove MAPs via chromatography [80]. | Studying direct compound effects on tubulin dimer polymerization without MAP interference. | Requires the addition of exogenous GTP to initiate polymerization. Provides a cleaner system for binding studies. |
| Recombinant | High purity and consistency, defined isotype composition. | High-throughput screening, structure-activity relationship (SAR) studies, and isotype-specific screening. | May lack the conformational complexity of native tubulin. Must validate that results translate to more physiologically relevant systems. |
Q3: Our team observed a hit compound losing efficacy when switching from recombinant to brain-purified tubulin. What could explain this?
This is a common challenge. The most likely explanation is that your hit compound's mechanism of action is dependent on a specific tubulin conformation or lattice state that is more prevalent in the recombinant system. As research shows, the tubulin conformational state (expanded GTP-state vs. compacted GDP-state) governs the accessibility of binding sites and C-terminal tails [79]. The compound may preferentially bind the expanded lattice promoted by GTP in the recombinant system. In brain-purified tubulin, the presence of MAPs like Tau (which promotes a compacted lattice) or other endogenous regulators may shift the conformational equilibrium, reducing the compound's binding and efficacy [79]. We recommend performing counter-screens against other cytoskeletal targets to check for specificity, a service offered by specialized CROs [1].
Troubleshooting Guide: Common Assay Inconsistencies
| Problem | Potential Causes | Recommendations |
|---|---|---|
| High variability in polymerization kinetics | 1. Inconsistent tubulin purification or storage.2. Variable GTP concentration or quality.3. Presence of contaminants affecting nucleation. | - Use a standardized purification protocol with a final chromatography step to remove MAPs and concentrate tubulin [80].- Aliquot and flash-freeze tubulin in a high-concentration PEM buffer.- Use fresh GTP solutions and confirm concentration spectrophotometrically. |
| Hit compounds from screening do not validate in cellular models | 1. The tubulin source used in biochemical assays lacks critical PTMs or protein partners found in cells.2. Compound permeability or metabolism in cells. | - Complement biochemical screens with cellular assays early in validation. Use live-cell tubulin probes (e.g., Tubulin Tracker) to visualize direct effects on microtubules [29].- Consider using patient-derived organoids that better replicate in vivo tumor heterogeneity for secondary screening [60]. |
| Unexpected polymerization inhibition or enhancement | 1. Compound interacts with buffer components (e.g., DMSO).2. Compound fluoresces at the assay wavelength (e.g., 350 nm), interfering with turbidity readouts. | - Include stringent vehicle controls and keep DMSO concentration consistent across all samples (typically ≤0.5%).- Run a parallel negative control without tubulin to check for compound-related absorbance. Confirm findings with an orthogonal method like circular dichroism (CD) spectroscopy [80]. |
Detailed Experimental Protocol: Tubulin Polymerization Assay
This protocol is adapted from established methods for measuring microtubule polymerization in vitro via turbidimetry [80].
Objective: To quantify the effects of candidate compounds on the polymerization kinetics of tubulin purified from different sources.
Materials:
- Tubulin: Purified from rat brain (MAP-free) or commercial porcine brain tubulin [1] [80].
- Buffer: PEM buffer (80 mM PIPES pH 6.9, 2 mM MgCl₂, 0.5 mM EGTA).
- Nucleotide: Guanosine 5'-triphosphate (GTP), prepared as a 10 mM stock in dH₂O.
- Test Compound: e.g., Δ9-THC or Paclitaxel (positive control inhibitor/promoter) [80].
- Equipment: UV/Vis spectrophotometer with a temperature-controlled cuvette holder.
Method:
- Tubulin Preparation: Thaw tubulin aliquots on ice. Centrifuge briefly before use to remove any aggregates. Keep on ice at all times.
- Reaction Setup: Prepare the polymerization master mix on ice. For a 1 mL reaction, combine:
- Compound Incubation: Pre-incubate the tubulin with the test compound or vehicle control (e.g., DMSO) for 2 minutes on ice [80].
- Data Acquisition:
- Set the spectrophotometer to 37°C and allow it to equilibrate.
- Transfer the reaction mixture to a pre-warmed cuvette.
- Immediately start monitoring the absorbance at 350 nm over time (typically 30-60 minutes) [80].
- Data Analysis: Plot absorbance (A350) versus time. Key kinetic parameters to extract from the curve include:
- Lag Phase: Time before rapid polymerization begins.
- Elongation Rate (Vmax): Maximum slope of the polymerization curve.
- Plateau (Amax): Maximum absorbance, indicating the total polymer mass.
The workflow below illustrates the key steps and decision points in this assay.
Mechanistic Insight: How Tubulin Conformation Affects Compound Binding
Understanding the underlying mechanism is key to troubleshooting. The following diagram illustrates how a compound's effect can be linked to the conformational state of tubulin, which varies by source and condition.
Research Reagent Solutions
The following table lists key materials and tools used in tubulin-based compound screening.
| Reagent / Tool | Function in Research | Example Use-Case |
|---|---|---|
| Porcine Brain Tubulin [1] | Standardized, commercially available native tubulin for biochemical assays. | Polymerization and binding assays in early drug discovery. |
| Tubulin Tracker Probes [29] | Live-cell fluorescent stains for β-tubulin. | Validating compound efficacy and visualizing microtubule dynamics in cellular models. |
| GTP (Guanosine 5'-triphosphate) [80] | Nucleotide required to initiate and sustain tubulin polymerization in vitro. | Essential component in all tubulin polymerization assays. |
| Patient-Derived Organoids (PDOs) [60] | 3D culture models that replicate tumor heterogeneity and patient-specific responses. | Secondary, physiologically relevant screening to triage hits from biochemical assays. |
| Specialized CRO Services [1] | Provide expert compound screening against tubulin and related targets (e.g., kinesins). | Off-target counter-screening and mechanism-of-action studies. |
Bridging the Gap Between Simple Cell Lines and Complex Physiology
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary limitations of using traditional 2D cell lines like Caco-2 for cytoskeletal drug screening? Traditional 2D cell lines, such as Caco-2, are reproducible, cost-efficient, and standardized. However, they demonstrate significant limitations, including impaired cellular complexity, modified cell function due to missing important transporters in the apical membrane, and inadequate expression of tight junction proteins or metabolic enzymes. This results in lower predictivity in drug screenings compared to more complex physiological systems [81].
FAQ 2: How can more physiologically relevant intestinal models be developed for pre-clinical screening? Primary organoid-based human intestinal tissue models represent an advanced system that closely reflects the in vivo situation. To overcome challenges related to the complexity, time, and cost of primary organoid cultures, research has demonstrated the establishment of immortalized, primary organoid-derived intestinal cell lines. These cell lines combine a standardized, cost-efficient culture system with the preservation of key cellular subtypes found in the native intestinal epithelium, offering improved barrier characteristics for bioavailability and toxicity studies [81].
FAQ 3: Which cytoskeletal targets are commonly screened in early drug discovery? Common cytoskeletal targets for compound screening include tubulin, kinesins (e.g., KIF18A), and myosins (e.g., cardiac myosin). These targets are implicated in a range of diseases, such as cancer, neurodegeneration, and cardiomyopathies. Available assays for these targets measure functions like polymerization, ATPase activity, and binding interactions [48].
FAQ 4: My flow cytometry data shows a weak fluorescence signal for my intracellular cytoskeletal target. What could be the cause? Weak or no signal in flow cytometry can stem from several issues related to sample preparation and experimental design [82] [83]:
- Inadequate Fixation/Permeabilization: Ensure you are using an optimized protocol for your specific intracellular target. For cytoskeletal proteins, fixation with 4% formaldehyde followed by permeabilization with saponin, Triton X-100, or ice-cold methanol is often required.
- Low Target Expression: Confirm that your treatment sufficiently induces the expression of the target protein.
- Dim Fluorochrome: Pair a low-abundance target with a bright fluorochrome (e.g., PE) to enhance detection.
- Instrument Settings: Verify that the cytometer's lasers and filter settings are compatible with the fluorochrome's excitation and emission spectra.
Troubleshooting Guides
Table 1: Troubleshooting Compound Screening Assays
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| High Assay Variability | Inconsistent protein quality or cell passage number. | Implement rigorous, multi-parameter QC protocols and use low-passage, authenticated cells [48]. |
| Unexpected IC50 Values | Off-target compound effects on related cytoskeletal proteins. | Run a counter-screen against a panel of motor proteins (e.g., kinesin homologs) to confirm specificity [48]. |
| Poor Predictivity for In Vivo Results | Over-reliance on simple 2D cell culture models. | Transition to more complex models, such as immortalized organoid-derived cell lines, which better mimic in vivo barrier integrity and transport functions [81]. |
Table 2: Troubleshooting Flow Cytometry for Cytoskeletal Studies
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| High Background Fluorescence | Non-specific antibody binding or dead cells. | Block Fc receptors prior to staining; use a viability dye to gate out dead cells; titrate antibodies to optimal concentration [82] [83]. |
| Weak Signal for Intracellular Target | Inefficient cell permeabilization. | Use fresh detergents (e.g., 0.1-0.5% Saponin) or alcohol-based permeabilization (ice-cold methanol) where appropriate [82] [83]. |
| Poor Separation of Cell Populations | Suboptimal instrument compensation or high spillover. | Use single-stained controls for accurate compensation; redesign panel with fluorochromes that have minimal spectral overlap [83]. |
Experimental Models & Protocols
Table 3: Comparison of Intestinal Epithelial Models for Drug Transport Studies
| Model Type | Key Features | Advantages | Disadvantages | Best Use Cases |
|---|---|---|---|---|
| Traditional 2D (Caco-2) | Human adenocarcinoma-derived cell line. | Cost-efficient, standardized, easy to handle [81]. | Low predictivity, missing key transporters, impaired barrier function [81]. | High-throughput initial screens. |
| Primary Organoids | 3D structures derived from human/murine intestinal crypts. | High in vivo similarity, forms crypt-villus axis, multiple cell types [81]. | Complex, time- and cost-intensive setup, variable cell composition [81]. | Mechanistic studies of transport and biology. |
| Immortalized Organoid-Derived Cell Lines | 2D polarized monolayers from lentivirally immortalized organoids. | Cost-efficient, standardized, improved barrier integrity, multiple cell types [81]. | Requires immortalization process. | Pre-clinical bioavailability and toxicity studies [81]. |
Protocol: Establishment of Immortalized Organoid-Derived Intestinal Monolayers
Methodology Summary (adapted fromhttps://pmc.ncbi.nlm.nih.gov/articles/PMC10916479/)
Isolation and Culture of Primary Organoids:
- Isolate intestinal crypts from human or murine tissue via incubation with 2 mM EDTA/HBSS−.
- Embed crypts in Matrigel droplets and culture in spheroid maintenance medium (SM medium) to form organoids.
- For differentiation, culture organoids in SM medium for at least 7 days.
Immortalization:
- Transduce organoids using a lentiviral cocktail containing immortalization genes (e.g., 12 genes for human organoids).
- Add 0.25% polybrene to the medium for 24 hours to enhance transduction efficiency.
- Two strategies can be used:
- Transduction in 2D: Culture primary cells as single cells on fibronectin/collagen-I coated plates before transduction.
- Transduction in 3D: Transduce organoids in suspension after isolating them from Matrigel.
Expansion of Cell Lines:
- After transduction, pick and expand formed colonies on fibronectin/collagen-I coated tissue culture plates.
- Culture the established immortalized cell lines in 2D for a standardized, cost-efficient model.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Reagents for Cytoskeletal Compound Screening
| Reagent / Material | Function in Research | Example Application in Screening |
|---|---|---|
| Porcine Brain Tubulin | A key cytoskeletal protein target. | Used in assays measuring polymerization dynamics and compound binding [48]. |
| Kinesin Proteins (e.g., KIF18A) | Key motor protein targets involved in cell division. | Screened in microtubule-activated ATPase assays for oncology drug discovery [48]. |
| Cardiac Myosin S1 Fragment | Key motor protein target in heart muscle. | Used in actin-activated ATPase assays for cardiomyopathy research [48]. |
| Matrigel | Basement membrane matrix. | Used for 3D culture of primary intestinal organoids [81]. |
| Saponin / Triton X-100 | Detergent-based permeabilization agents. | Critical for enabling antibody access to intracellular cytoskeletal targets in flow cytometry [82] [83]. |
| Fixable Viability Dyes (e.g, eFluor, 7-AAD) | To distinguish live from dead cells. | Gating out dead cells during flow cytometry to reduce non-specific background [83]. |
Diagrams and Workflows
Diagram 1: Cytoskeletal Drug Screening Workflow
Diagram 2: Advanced In Vitro Model Development
Diagram 3: Cytoskeleton in Substance Use Disorder
Enhancing Predictive Accuracy with Z-Stack Imaging and 3D Analysis
This technical support center provides troubleshooting and methodological guidance for researchers employing Z-stack imaging and 3D analysis in cytoskeletal drug target compound screening. The complex biology of the cytoskeleton—including tubulin, kinesins, and associated proteins—is best studied in physiologically relevant 3D models. However, these advanced models present unique imaging and analytical challenges. The following guides and protocols are designed to help you overcome these hurdles to generate high-quality, reproducible data that enhances the predictive accuracy of your preclinical research.
Frequently Asked Questions (FAQs)
Q1: Why is my 3D image data blurry, especially in deeper tissue regions?
Blurry images in thick samples are primarily caused by light scattering, where out-of-focus light from different focal planes reduces clarity and contrast [84]. This is a common challenge when imaging 3D cell cultures or microtissues that exceed the microscope's depth of focus.
- Solution: Apply image deconvolution. This computational technique uses your microscope's Point Spread Function (PSF) to mathematically reassign out-of-focus light back to its origin [85].
- Recommended Algorithm: For fluorescence microscopy, the Richardson-Lucy algorithm is often preferred as it assumes Poisson noise, common in photon-limited imaging conditions [85].
- Benefit: Deconvolution enhances image clarity, improves signal-to-noise ratio, and refines axial resolution for more accurate 3D reconstructions [85].
Q2: How can I prevent phototoxicity and photobleaching during long-term 3D live-cell imaging?
Phototoxicity and photobleaching occur because 3D imaging requires capturing multiple Z-plane images (Z-stacks), and for techniques like confocal microscopy, the entire specimen is illuminated for each plane. This cumulative light exposure can damage cells and quench fluorophores [84].
- Solution:
- Use Light Sheet Fluorescence Microscopy (LSFM): LSFM illuminates only the single plane being imaged, drastically reducing light exposure. One study noted that while only about 20 Z-layers could be imaged with confocal microscopy before reaching phototoxic limits, each layer could be illuminated about 100 times with LSFM for long-term experiments [84].
- Optimize Acquisition Settings: If LSFM is unavailable, minimize laser power and exposure time. Use the longest practical wavelength for illumination, as phototoxicity is generally lower at higher wavelengths (e.g., in multiphoton microscopy) [84].
- Employ Sensitive Detectors: Use ultra-sensitive cameras to allow for lower light doses while maintaining image quality [84].
Q3: The brightness of my Z-stacks is uneven from top to bottom. How can I correct this?
Uneven brightness, where deeper regions appear darker, is caused by light attenuation due to refraction and scattering as light travels through the sample [86].
- Solution: Use a Z-Intensity Correction function, available in software like Nikon's NIS-Elements. This feature automatically adjusts the laser power and gain settings based on the Z-position during acquisition.
- Protocol:
- Open the Z Intensity Correction control panel in your acquisition software.
- At your starting Z-position, adjust laser power and gain for optimal brightness.
- Register these settings for that Z-position.
- Move to the deepest Z-position of your sample and readjust laser power and gain to match the reference brightness.
- Register these settings. The software will create a linear function to interpolate settings between these points [86].
- Result: A 3D image with uniform brightness throughout the entire Z-stack [86].
- Protocol:
Q4: My 3D simulation of drug diffusion is not achieving realistic results. What should I check?
This often relates to the initial setup and parameters of the simulation.
- Solution:
- Review Assumptions and Parameters: Ensure your model, boundary conditions, and material properties (e.g., density, porosity of the ECM) are realistic and consistent with your biological system [87].
- Check Mesh Settings: In Finite Element Analysis, an overly coarse mesh can miss critical details. Refine your mesh size in regions of interest [87].
- Validate and Verify: Use sensitivity analysis to test how changes in input parameters affect your results. Where possible, compare simulation outputs with empirical data [87].
Troubleshooting Guides
Issue: Poor Antibody Penetration in Cleared 3D Tissues
Problem: Immunostaining of thick or cleared tissues (e.g., using CLARITY) results in a non-uniform "sandwich" staining pattern, where antibodies fail to penetrate the core of the sample [88].
Investigation & Resolution:
- Validate Antibody Compatibility: Confirm that your primary antibodies are compatible with the clearing method and hydrogel-embedding process. Some epitopes may be masked or altered.
- Optimize Staining Conditions: Systematically titrate antibody concentrations and extend incubation times. Use gentle agitation throughout the staining process to enhance diffusion [88].
- Include Rigorous Controls: Perform isotype control stains to confirm specific antibody binding and minimize background in the processed tissues [88].
Issue: Low-Throughput Data Analysis from 3D Microtissues
Problem: Manually quantifying complex phenotypes (e.g., lumen formation, cytoskeletal organization) across hundreds of 3D microtissues is time-consuming and subjective.
Investigation & Resolution:
- Implement Machine Learning (ML): Establish a pipeline to extract high-content morphological features from your 3D images.
- Develop a Classifier: Train an ML classification model using these features to automatically identify and score treatment effects.
- Example: A study on MCF-7 microtissues exposed to estrogenic chemicals extracted 140 image features to build a model that predicted chemical exposure with high accuracy (AUC-ROC > 0.95) [89].
- Incorporate Deep Learning: For specific structures like gland lumens, use deep learning-based software to fully automate the characterization of counts and volumes [89].
Experimental Protocols & Data Presentation
Detailed Protocol: 3D Confocal Imaging of a Proximal Tubule Model with Z-Intensity Correction
This protocol is adapted for imaging a 3D cytoskeletal structure embedded in a collagen matrix, relevant for drug screening [86].
1. Sample Preparation:
- Model: Human proximal tubule model constructed within a collagen gel in a microfluidic chip.
- Staining: Standard immunofluorescence staining for cytoskeletal markers (e.g., tubulin, F-actin) and relevant cellular structures.
2. Microscope Setup:
- Instrument: Confocal microscope (e.g., Nikon AX/AX R).
- Software: NIS-Elements Imaging Software.
- Objective: High-resolution water-immersion objective (e.g., 60x).
3. Z-Intensity Correction Setup:
- Access the
Z Intensity Correctionpanel from theAcquisition Controlsmenu. - Navigate to the topmost Z-plane of your structure. Adjust
Laser PowerandGainto achieve optimal, non-saturating signal. Click the[+]button to register these settings for this Z-position. - Navigate to the bottommost Z-plane of your structure. Increase
Laser PowerandGainuntil the image brightness matches the top plane. Click the[+]button to register these settings. - The software will create a linear interpolation of settings between these points.
4. Image Acquisition:
- In the
ND Acquisitionpanel, define the total Z-range and step size for the stack. - Click the
[Run Z Corr]button to begin the acquisition. The system will automatically adjust power and gain at each Z-step.
Quantitative Data from Key Studies
The following table summarizes quantitative findings from recent studies that underscore the value of 3D analysis.
Table 1: Quantitative Comparisons of 2D vs. 3D Analysis in Biological Research
| Study Focus | Key Quantitative Finding | Implication for Predictive Accuracy |
|---|---|---|
| Ki67 Heterogeneity in Breast Cancer [88] | CLARITY (3D) analysis revealed significant intra-tumoral variation in Ki67 expression that was not evident in conventional 2D FFPE sections. | 3D volumetric assessment reduces sampling bias, enabling a more accurate and unbiased analysis of tumor heterogeneity. |
| Rare Cell Detection [88] | A cell pellet model demonstrated the ability to manually detect rare cells at a ratio of 0.01% within a 3D context using CLARITY. | Enhances the ability to find rare, clinically relevant cell populations (e.g., drug-resistant cells) that are critical for therapy outcomes. |
| Estrogenic Effect Prediction [89] | A machine learning model trained on 140 image features from 3D MCF-7 microtissues predicted exposure to estradiol with an AUC-ROC of 0.9528. | High-content 3D imaging combined with ML provides a highly accurate, animal-free method for toxicological screening and drug efficacy testing. |
Research Reagent Solutions
The table below lists key materials and reagents essential for setting up 3D cultures and imaging for cytoskeletal drug screening.
Table 2: Essential Research Reagents for 3D Cytoskeletal Screening Assays
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Non-adhesive Agarose Hydrogels [89] | Provides a scaffold-free environment for the self-assembly of consistent 3D microtissues (e.g., MCF-7 spheroids). | Creating uniform 3D models for high-content screening of compounds affecting cell morphology and cytoskeletal organization [89]. |
| CLARITY Hydrogel Mixture [88] | Forms a polymer mesh that crosslinks biological molecules, enabling lipid clearing and tissue transparency while preserving structural integrity. | Processing patient-derived biopsies for 3D multiplexed immunofluorescence analysis of cytoskeletal and tumor biomarkers [88]. |
| Optical Clearing Reagents (ScaleS4) [89] | A refractive index-matched aqueous solution that renders fixed tissues transparent for deep imaging. | Clearing fixed 3D microtissues prior to high-resolution confocal imaging to reduce light scattering [89]. |
| Microfluidic MPS Chips [86] | Chips that provide a dynamic, physiologically relevant environment for cultivating and observing complex 3D tissue models (e.g., proximal tubules). | Advanced organ-on-a-chip studies where fluid flow and mechanical stresses influence cytoskeletal dynamics and drug response [86]. |
| Tubulin & Kinesin Assays [1] | Mechanistically validated biochemical assays (e.g., polymerization, ATPase) for profiling compound effects on specific cytoskeletal targets. | Primary and off-target screening of compounds for specificity against tubulin, KIF18A, and other cytoskeletal motors [1]. |
Workflow and Pathway Diagrams
3D Spheroid Imaging & Analysis Workflow
Cytoskeletal Drug Screening Signaling Pathway
Target Validation and Hit Confirmation: Integrating Multi-dimensional Assessment
Target Deconvolution Strategies for Phenotypic Screening Hits
Troubleshooting Guides and FAQs
Common Experimental Failures and Solutions
Problem: High Background Noise in Affinity Purification Mass Spectrometry
- Potential Cause: Non-specific binding of proteins to the affinity matrix or the compound's solid support.
- Solution: Incorporate more stringent wash conditions (e.g., higher salt concentrations, detergents like CHAPS). Use control beads with an inactive enantiomer or a structurally similar but inactive compound to identify and subtract non-specific binders [90].
- Prevention: Optimize the coupling chemistry to ensure the compound is efficiently immobilized and the support is properly blocked.
Problem: Loss of Compound Activity After Tagging
- Potential Cause: The addition of an affinity tag (e.g., biotin) or a photoreactive group alters the compound's structure, hindering its ability to bind the target.
- Solution: Employ a "tag-free" or "clickable" approach. Attach a small, minimally disruptive tag (like an alkyne) to the compound. After the compound has bound to its target in cells, use copper-free click chemistry to attach the bulky affinity tag (like biotin-azide) for purification [90].
- Prevention: Perform Structure-Activity Relationship (SAR) studies first to identify positions on the molecule that can be modified without affecting its biological activity.
Problem: Inability to Identify the Target in Low-Abundance Protein Scenarios
- Potential Cause: Standard proteomics methods lack the sensitivity to detect proteins that are expressed at very low levels, even if they are specifically enriched.
- Solution: Utilize quantitative mass spectrometry techniques like thermal protein profiling (TPP) or solvent-induced denaturation shift assays (e.g., SideScout). These methods detect ligand binding through changes in protein thermal stability, which can be more sensitive for low-abundance targets than direct enrichment [91].
- Prevention: Fractionate the protein sample before mass spectrometry analysis to reduce complexity and increase the depth of coverage.
Frequently Asked Questions
Q1: When should I use a phenotypic screening approach versus a target-based approach? A: Phenotypic screening is advantageous when you want to discover compounds in a physiologically relevant, complex biological system without preconceived notions of the target. This approach has been historically more efficient at generating first-in-class drugs. Target-based screening is more suitable when a specific, well-validated molecular target is already known, allowing for a more direct and optimized drug design process [90] [92].
Q2: My hit compound is not amenable to chemical modification for an affinity tag. What are my options? A: Several label-free target deconvolution strategies are available:
- Protein Stability Profiling: Techniques like thermal proteome profiling (TPP) detect shifts in a protein's melting temperature upon compound binding, enabling proteome-wide target identification without chemical modification [91].
- Computational Methods: Knowledge graphs and molecular docking can predict potential targets by integrating biological data and analyzing the compound's predicted binding affinity to thousands of proteins, as demonstrated for the p53 pathway activator UNBS5162 [93].
- Genomic Methods: CRISPR-based screens or resistance generation can help identify targets or pathways essential for the compound's activity.
Q3: How can I distinguish direct targets from indirect or downstream effectors? A: This is a central challenge. A combination of methods increases confidence:
- Direct Binding vs. Functional Effect: Techniques like affinity purification or photoaffinity labeling demonstrate direct physical interaction. In contrast, methods like RNAi or CRISPR screens identify genes important for the phenotype, which may be indirect.
- Correlation of Affinity and Potency: For a direct target, the compound's binding affinity (e.g., Kd) should correlate with its functional potency (e.g., IC50) in the phenotypic assay.
- Cellular Engagement: Use cellular assays like cellular thermal shift assays (CETSA) to confirm the compound engages with the proposed target in a live-cell context.
Q4: What are the best practices for validating a deconvoluted target? A: A multi-faceted validation strategy is crucial:
- Genetic Validation: Knockdown or knockout of the proposed target should recapitulate the phenotypic effect of the compound, and overexpression may confer resistance.
- Biochemical Validation: Show direct binding using orthogonal methods like surface plasmon resonance (SPR) or isothermal titration calorimetry (ITC).
- Pharmacological Validation: Demonstrate that known agonists/antagonists of the proposed target produce similar/opposite phenotypic effects.
- Rescue Experiments: Re-introduction of the wild-type target (but not a binding-deficient mutant) should restore sensitivity to the compound.
Detailed Experimental Methodologies
Affinity Chromatography and Photoaffinity Labeling
This is a cornerstone technique for direct target identification [90] [91].
Protocol:
- Probe Design: Immobilize the hit compound onto solid support beads (e.g., agarose, magnetic beads). A photoreactive group (e.g., diazirine) and a clickable handle (e.g., alkyne) can be incorporated for photoaffinity labeling (PAL).
- Sample Preparation: Incubate the compound-conjugated beads with a cell lysate or a complex protein mixture. For PAL, the trifunctional probe is applied to live cells or lysates first, followed by UV irradiation to cross-link the compound to its bound proteins.
- Wash and Elution: Wash the beads extensively with buffer to remove non-specifically bound proteins. Specifically bound proteins are eluted using a competitive ligand, high salt, or SDS-PAGE loading buffer.
- Protein Identification: The eluted proteins are separated by gel electrophoresis and identified by in-gel digestion and mass spectrometry (e.g., LC-MS/MS), or analyzed directly by "shotgun" proteomics.
Activity-Based Protein Profiling (ABPP)
ABPP is particularly powerful for identifying targets within specific enzyme families (e.g., proteases, kinases) [90].
Protocol:
- Probe Design: An Activity-Based Probe (ABP) contains three elements: a reactive group that covalently binds the enzyme active site, a linker region, and a reporter tag (e.g., biotin or a clickable alkyne).
- Labeling: Treat cells or cell lysates with the ABP. The probe will covalently tag active enzymes of the desired class.
- Enrichment and Detection: Lyse the cells and use the reporter tag (e.g., streptavidin beads for biotin) to enrich the labeled proteins. These are then identified by mass spectrometry.
- Competition Profiling: To identify targets of a specific inhibitor, pre-treat cells with the inhibitor followed by the ABP. Proteins whose labeling is reduced in the presence of the inhibitor are candidate targets.
Knowledge Graph and In Silico Target Prediction
This computational approach leverages existing biological data to rapidly narrow down candidate targets [93].
Protocol:
- Knowledge Graph Construction: Build or utilize a pre-existing knowledge graph that integrates data on protein-protein interactions, drug-target interactions, and pathway information (e.g., from databases like STRING, ChEMBL).
- Phenotypic Input: Start with a hit compound from a phenotypic screen (e.g., a molecule that activates a p53-luciferase reporter).
- Network Analysis: Use the knowledge graph to analyze the network of proteins associated with the observed phenotype (e.g., proteins in the p53 signaling pathway). This drastically narrows the list of candidate proteins from thousands to a manageable number (e.g., from 1088 to 35).
- Molecular Docking: Perform in silico docking of the hit compound against the shortlisted candidate proteins to predict binding affinity and pose. Top-scoring candidates are then prioritized for experimental validation.
Experimental Workflow Visualization
Affinity Chromatography Target Deconvolution
Activity-Based Protein Profiling (ABPP) Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 1: Key Reagents and Services for Target Deconvolution in Cytoskeletal Research
| Reagent/Service | Function/Description | Example Application in Cytoskeletal Research |
|---|---|---|
| Tubulin Polymerization Assays [1] | Measures the rate and extent of microtubule assembly in vitro. Used to screen for compounds that stabilize or destabilize microtubules. | Primary screen for identifying compounds that mimic taxol (stabilizers) or colchicine (destabilizers). |
| Motor Protein ATPase Assays [1] | Quantifies the ATP hydrolysis activity of motor proteins (kinesins, myosins). Inhibition indicates direct interference with motor function. | Counter-screening to assess specificity of a KIF18A inhibitor against a panel of other kinesins [1]. |
| Selective Compound Libraries [92] | A collection of highly selective tool compounds with well-defined molecular targets. Used in phenotypic screens to link a phenotype to a specific target. | Screening a library of 87 selective compounds on the NCI-60 cancer cell line panel to implicate novel targets in cancer cell growth [92]. |
| Affinity Purification Services (e.g., TargetScout [91]) | Commercial services that handle the immobilization of your compound and subsequent pull-down and mass spectrometry analysis. | Identifying the direct binding partners of a novel tubulin-binding compound without in-house proteomics expertise. |
| Photoaffinity Labeling Services (e.g., PhotoTargetScout [91]) | Specialized services that design and utilize photoreactive probes to capture transient or low-affinity protein-compound interactions. | Mapping the binding site of a compound on a kinesin motor protein or identifying weak interactors in a complex cytoskeletal network. |
| Stability Profiling Assays (e.g., SideScout [91]) | Label-free method to identify targets by detecting ligand-induced changes in protein thermal stability across the proteome. | Confirming target engagement in a complex cellular lysate for a compound targeting a cytoskeletal regulatory protein like PAK2. |
In the field of cytoskeletal drug discovery, selecting the appropriate screening strategy is paramount for success. Researchers are often faced with a choice between two fundamental approaches: biochemical assays, which focus on isolated molecular targets, and phenotypic screens, which assess compound effects in a more physiologically relevant cellular context. Biochemical methods, such as enzyme and binding assays, are target-centric and ideal for understanding direct interactions with proteins like actin or tubulin [94]. In contrast, phenotypic drug discovery evaluates compounds based on their ability to induce a desired change in a cell's state, such as altering cytoskeletal dynamics or cell morphology, without requiring prior knowledge of a specific molecular target [95] [96]. This technical support center is designed to guide researchers through the practical application, troubleshooting, and selection of these methodologies within the specific context of cytoskeletal research.
The table below summarizes the core characteristics of each screening approach to aid in initial method selection.
| Feature | Biochemical Screening | Phenotypic Screening |
|---|---|---|
| Primary Focus | Isolated molecular targets (e.g., enzymes, receptors) [94] | Cellular/system-level outcomes (e.g., morphology, survival) [95] |
| Typical Readout | Target binding affinity, enzyme inhibition kinetics [94] | Changes in gene expression, cell shape, viability, cytoskeletal organization [97] [75] |
| Throughput | Very high, easily automated for High-Throughput Screening (HTS) | Can be high, but often more complex and costly (e.g., High-Content Screening) [97] |
| Target Identification | Known a priori | Requires subsequent deconvolution [96] |
| Physiological Relevance | Lower; examines interactions outside native cellular environment | Higher; conducted in living cells or systems [95] [94] |
| Hit Rate for First-in-Class Drugs | Lower (38% of first-in-class small molecules, 1999-2008) [95] | Higher (62% of first-in-class small molecules, 1999-2008) [95] |
| Ideal for Cytoskeletal Research When... | Investigating a specific, known cytoskeletal protein (e.g., PAK2 kinase) [98] | The therapeutic goal is a complex phenotypic change (e.g., altering dendritic spine density) [26] |
Experimental Protocols for Cytoskeletal Research
Protocol for a Biochemical Binding Assay (e.g., for Actin-Binding Proteins)
Objective: To quantify the binding affinity of a small-molecule compound to a purified cytoskeletal protein, such as an actin-binding protein like cofilin or myosin.
Materials:
- Purified target protein (e.g., nonmuscle myosin II, NmII).
- Test compounds.
- Fluorescently labeled ligand or substrate.
- Assay plates (e.g., 384-well).
- Fluorescence polarization plate reader.
Methodology:
- Solution Preparation: Prepare a serial dilution of the test compound in a suitable assay buffer.
- Reaction Setup: In each well, mix a fixed, low concentration of the fluorescently labeled ligand with the purified target protein.
- Competition Incubation: Add the varying concentrations of the test compound to the wells. The compound and the fluorescent ligand will compete for binding sites on the target protein.
- Incubation: Allow the plate to incubate in the dark at a controlled temperature (e.g., room temperature for 1 hour) to reach binding equilibrium.
- Measurement: Read the plate using a fluorescence polarization reader. Polarization values are measured in millipolarization units (mP).
- Data Analysis: The degree of fluorescence polarization is inversely proportional to the amount of compound bound. A dose-response curve is generated, and the IC50 (half-maximal inhibitory concentration) value is calculated. This can be used to derive the inhibition constant (Ki), which represents the binding affinity of the test compound [94].
Protocol for a Phenotypic Screen (e.g., for Altered Cytoskeletal Morphology)
Objective: To identify compounds that induce a specific phenotypic change related to the cytoskeleton, such as the rearrangement of mitochondrial networks or changes in dendritic spine density.
Materials:
- Relevant cell line (e.g., DLBCL models like U2932 for cancer studies) [75].
- Test compound library.
- Cell culture plates (e.g., 96-well or 384-well for HTS).
- Fluorescent dyes (e.g., MitoTracker for mitochondria, phalloidin for F-actin).
- High-content imaging system or flow cytometer.
- Fixative and permeabilization reagents.
Methodology:
- Cell Seeding: Plate cells at an optimized density in assay plates and allow them to adhere overnight.
- Compound Treatment: Treat cells with the test compounds for a predetermined time.
- Staining: Fix the cells and stain with fluorescent probes specific to the cytoskeletal or organellar feature of interest. For instance, use MitoTracker Deep Red FM to visualize mitochondria and a phalloidin conjugate to stain filamentous actin (F-actin) [75].
- Image Acquisition: Use a high-content imaging system to automatically capture multiple fields per well at high magnification.
- Image & Data Analysis: Utilize image analysis software to quantify phenotypic parameters. This can include:
- Mitochondrial Morphology: Categorizing mitochondria as fragmented, mixed, or tubular [75].
- Cytoskeletal Integrity: Quantifying F-actin intensity, distribution, or formation of stress fibers.
- Cell Shape: Measuring parameters like cell area, perimeter, and form factor.
- Hit Selection: Compounds that induce a statistically significant shift in the desired phenotypic readout are identified as "hits" for further validation [97].
Troubleshooting Common Experimental Issues
FAQ 1: Our biochemical assay for a kinase involved in cytoskeletal regulation shows high background noise, leading to poor Z'-factor. What could be the cause?
- Potential Cause: Non-specific binding of the compound or fluorescent probe to assay components (e.g., plates, proteins).
- Solution: Optimize the concentration of the target protein and the detection probe. Include a DMSO control (the compound solvent) to account for solvent effects. Use a blocking agent like BSA in the assay buffer to reduce non-specific binding. Re-evaluate the purity and stability of the protein and compounds.
FAQ 2: In a phenotypic screen for actin polymerization modulators, we are seeing high well-to-well variability in our high-content images. How can we improve consistency?
- Potential Cause: Inconsistent cell seeding density, uneven staining, or plate edge effects (evaporation).
- Solution:
- Standardize Seeding: Use an automated cell counter and dispenser to ensure uniform cell density across all wells.
- Optimize Staining: Perform staining and washing steps using a multichannel pipette or an automated plate washer to ensure uniformity. Validate staining concentrations and incubation times.
- Control Environment: Use microplate lids and ensure the incubator has high humidity and precise temperature/CO2 control to minimize edge effects. Include positive and negative control compounds (e.g., Jasplakinolide and Cytochalasin D for actin) on every plate to normalize data.
FAQ 3: We have a hit from a phenotypic screen that alters mitochondrial shape, but we don't know its molecular target. How do we proceed with target deconvolution?
- Solution: This is a common challenge in phenotypic screening [96]. Several strategies can be employed:
- Affinity Purification: Immobilize the hit compound on a solid support and use it as "bait" to pull down interacting proteins from cell lysates, which can then be identified by mass spectrometry.
- Genomic Screening: Use CRISPR-Cas9 knockout libraries to identify genes whose loss makes cells resistant or hypersensitive to the compound, as demonstrated in a CDC resistance study [75].
- Transcriptomic Profiling: Compare the gene expression signature of cells treated with the hit compound to signatures of compounds with known targets using databases like the Connectivity Map [96].
Frequently Asked Strategic Questions
FAQ 4: When should I prioritize a phenotypic screen over a biochemical screen for a cytoskeletal target? Prioritize a phenotypic screen when:
- The therapeutic goal is to achieve a complex cellular outcome (e.g., change in cell motility, differentiation, or survival) that may involve multiple cytoskeletal targets or pathways [26] [96].
- The specific molecular target is unknown, but a robust and disease-relevant cellular model is available.
- You aim to discover first-in-class drugs with novel mechanisms of action, as phenotypic screens have historically been more successful in this area [95].
FAQ 5: How can we leverage computational methods to enhance these screening approaches? Computational methods are becoming increasingly integral:
- For Biochemical/Target-Based Screening: In silico target prediction and virtual screening methods like molecular docking can prioritize compounds likely to bind a specific cytoskeletal target (e.g., PAK2), saving wet-lab resources [99] [98]. Tools like MolTarPred have been shown to be effective for this purpose [99].
- For Phenotypic Screening: Machine learning frameworks, such as the DrugReflector model, use transcriptomic data to predict compounds that induce a desired phenotypic change, dramatically improving hit rates [96]. These methods can make phenotypic campaigns smaller and more focused.
Research Reagent Solutions for Cytoskeletal Screening
The table below lists key reagents and their applications in cytoskeletal drug screening experiments.
| Reagent / Material | Function in Screening | Example Application |
|---|---|---|
| MitoTracker Dyes | Fluorescent probes that label live mitochondria. | Tracking mitochondrial rearrangements and health in phenotypic screens [75]. |
| Phalloidin Conjugates | High-affinity fluorescent probes that selectively stain F-actin. | Visualizing and quantifying changes in the actin cytoskeleton via microscopy [26]. |
| CRISPR-Cas9 Libraries | Tools for genome-wide knockout screening. | Identifying genes involved in resistance or sensitivity to a compound (target deconvolution) [75]. |
| DuoHexaBody-CD37 | An engineered antibody that potently induces Complement-Dependent Cytotoxicity (CDC). | Applying selective pressure in phenotypic screens to study intracellular resistance mechanisms in cancer models [75]. |
| Mt-Keima Reporter | A pH-sensitive fluorescent protein used to measure mitophagy. | Quantifying mitochondrial turnover in live cells as a functional phenotypic readout [75]. |
| Blebbistatin (Blebb) | A selective small-molecule inhibitor of nonmuscle myosin II (NmII). | Used as a tool compound in biochemical and phenotypic assays to validate the role of actin dynamics in a cellular process [26]. |
Signaling Pathways and Experimental Workflows
Cytoskeletal Dynamics in CDC Resistance
This diagram visualizes the intracellular signaling pathway linking cytoskeletal dynamics to therapy resistance, as identified in DLBCL models [75].
Phenotypic Screening & Hit Deconvolution Workflow
This diagram outlines a generalized workflow for conducting a phenotypic screen and subsequent target identification [96] [75].
The Cellular Thermal Shift Assay (CETSA) is a pivotal label-free technique for confirming target engagement in a physiologically relevant cellular context. It is based on the biophysical principle of ligand-induced thermal stabilization, where a drug binding to its target protein, such as tubulin or other cytoskeletal components, alters the protein's thermal stability [100] [101]. This change in stability is measured as a shift in the protein's melting temperature (Tm), providing direct evidence of binding within living cells [102]. For research on cytoskeletal drug targets, this is particularly valuable. It moves beyond simple biochemical assays using purified tubulin and allows researchers to verify that a compound not only binds to its intended target in a complex cellular environment but also to study subsequent effects on protein interactions and pathway modulation [100]. This capability is crucial for understanding the mechanism of action of compounds targeting the microtubule cytoskeleton, which is a validated target for cancer therapy and other diseases [11].
CETSA Experimental Workflow
The following diagram illustrates the core workflow of a CETSA experiment, from cell preparation to data analysis.
Detailed Protocol for CETSA
- Sample Preparation: Plate cells according to the required conditions and density. Treat cells with the test compound or a vehicle control under sterile culture conditions. The incubation period should be sufficient to allow cellular uptake and target binding but ideally not so long that phenotypic effects like apoptosis significantly alter the protein landscape [45].
- Heat Application: After incubation, subject the cell samples to a series of precise temperatures in a thermal gradient. Each temperature point is maintained for a set period (e.g., 3 minutes) to induce protein denaturation [45] [102].
- Cell Lysis and Protein Extraction: Lyse the heated cells using multiple freeze-thaw cycles (e.g., rapid freezing in liquid nitrogen followed by thawing at 37°C). This process releases the cellular contents while leaving denatured and aggregated proteins insoluble [102].
- Soluble Protein Quantification: Separate the soluble protein fraction (containing non-denatured, folded proteins) from the aggregates by centrifugation. The remaining soluble target protein is then quantified using a detection method of choice [45] [102].
- Data Analysis: Plot the amount of soluble protein remaining against the temperature to generate melt curves. A rightward shift in the melting temperature (Tm) of the target protein in compound-treated samples compared to the control indicates ligand-induced thermal stabilization and confirms cellular target engagement [45] [101].
Key CETSA Formats and Data Outputs
CETSA can be implemented in several formats, each with different throughput, equipment requirements, and applications. The table below summarizes the key characteristics.
| Format | Detection Method | Throughput | Primary Application in Drug Discovery | Key Advantages |
|---|---|---|---|---|
| CETSA Classics [101] | Western Blot | Low | Target engagement for a limited number of compounds; late-stage lead optimization. | Simple, uses standard lab equipment; suitable for hypothesis-driven studies [102]. |
| CETSA HT (High-Throughput) [101] | Dual-antibody & proximity detection (e.g., chemiluminescence) | High (384/1536-well plates) | Screening of medium-sized compound libraries; SAR analysis and hit confirmation [101]. | Enables rapid screening and generation of cellular potency (EC50) data. |
| CETSA MS / TPP (Thermal Proteome Profiling) [102] [101] | Mass Spectrometry | Medium to High | Proteome-wide identification of drug targets and off-target effects; deconvolution of hits from phenotypic screens. | Unbiased analysis of thousands of proteins simultaneously; identifies direct and indirect interactions [102]. |
| 2D-TPP (Two-Dimensional TPP) [102] | Mass Spectrometry | Medium | Provides a high-resolution view of binding dynamics by analyzing both temperature and compound concentration gradients. | Allows for quantitative assessment of drug-binding affinities and mechanisms of action [102]. |
| Imaging-Based CETSA [101] | High-Content Imaging | Medium | In-situ target engagement studies in adherent cells; can study drug and target localization. | Allows for the study of multiple targets simultaneously and provides spatial information. |
Troubleshooting Common CETSA Issues
Q1: We are testing a compound in a whole-cell CETSA experiment but see no thermal shift, even though it is potent in biochemical assays. What could be wrong?
- A: The most likely culprit is poor cell membrane permeability. The compound may not efficiently cross the cell membrane to reach its intracellular target. This is a key differentiator between CETSA and biochemical assays [45].
- Troubleshooting Steps:
- Confirm Cellular Activity: Check if the compound produces the expected phenotypic or functional effect in a cell-based assay (e.g., inhibition of proliferation).
- Lysate CETSA: Repeat the CETSA experiment in cell lysates instead of intact cells. If a thermal shift is observed in the lysate but not in whole cells, it strongly suggests a permeability issue [45] [101].
- Increase Incubation Time: Extend the compound incubation time to see if a slower accumulation in cells induces a shift, though this must be balanced against potential compound stability or phenotypic effects [101].
Q2: Our DSF (a related biochemical TSA) melt curves are irregular or show high background fluorescence. How can we improve the data quality?
- A: This is a common issue often related to buffer components or the test compounds themselves [45].
- Troubleshooting Steps:
- Check Compound-Dye Interactions: Test your compounds in the absence of protein. Some compounds are intrinsically fluorescent or can quench the dye's fluorescence, interfering with the signal [45].
- Optimize Buffer Composition: Ensure your buffer is compatible with the fluorescent dye. Detergents and viscosity-increasing additives can cause high background in DSF. Consider using alternative buffers or dyes [45].
- Verify Protein Stability: Ensure the recombinant protein is stable, soluble, and not pre-aggregated at ambient temperature in the chosen buffer [45].
Q3: In our PTSA (Protein Thermal Shift Assay) or Western blot-based CETSA, the protein bands are faint or absent. What should we check?
- A: This typically points to issues with protein detection or overloaded denaturation.
- Troubleshooting Steps:
- Include a Loading Control: Use a heat-stable protein as a loading control (e.g., SOD1, APP-αCTF, β-actin, GAPDH) for normalization and to confirm that the total protein load is consistent and detectable across samples [45].
- Optimize Antibodies: Ensure the primary antibody is specific and validated for detecting the native, folded form of the target protein in the assay conditions.
- Adjust Temperature Range: The chosen temperature gradient might be too harsh, denaturing nearly all the protein. Expand the range to include lower temperatures to capture the melt curve's initial phase [45].
Q4: How do we interpret the EC50 from an ITDR-CETSA (Isothermal Dose-Response) experiment?
- A: The EC50 from ITDR-CETSA represents the concentration of compound required to stabilize 50% of the target protein at a fixed temperature. It provides a measure of cellular potency, which incorporates factors like cell permeability, efflux, and metabolism, unlike the binding affinity (Kd) measured in purified systems [102] [101]. It is common for the CETSA EC50 to be less potent than the biochemical IC50, and this data is highly relevant for medicinal chemistry optimization [101].
The Scientist's Toolkit: Key Research Reagents and Materials
The table below lists essential materials and reagents for setting up and executing CETSA experiments.
| Reagent / Material | Function / Application | Considerations for Cytoskeletal Targets |
|---|---|---|
| Polarity-Sensitive Dye (e.g., SyproOrange) | Used in DSF to bind exposed hydrophobic regions of unfolding recombinant proteins [45]. | Incompatible with detergents; check for interference from test compounds [45]. |
| Heat-Stable Loading Controls (e.g., SOD1, APP-αCTF) | Essential for normalizing protein quantification in PTSA and CETSA Western blots [45]. | More reliable than common controls like GAPDH or β-actin due to superior heat stability [45]. |
| Cell Lysis Buffer (with Protease Inhibitors) | To lyse cells after heating while preserving the soluble protein fraction. | Must be optimized to ensure complete lysis without solubilizing denatured aggregates. |
| Specific Antibodies (for WB-CETSA or CETSA HT) | To detect and quantify the target protein in the soluble fraction after heating. | Must be validated for specificity and ability to recognize the native, folded target protein. |
| Recombinant Target Protein (e.g., Tubulin) | For initial DSF or PTSA experiments to confirm direct binding in a biochemical setting [45] [1]. | Serves as a valuable stepping stone between biochemical and cellular assays [45]. |
| Permeabilization Agents | To investigate whether a lack of shift in whole-cell CETSA is due to permeability. | Use with caution as it alters native cell physiology. Data should be compared with intact cell and lysate results. |
Complementary Functional Assays for Cytoskeletal Targets
Confirming target engagement with CETSA is a critical step, but it should be integrated with functional assays to link binding to a biological outcome. For cytoskeletal targets like tubulin and kinesins, this is especially important.
- Microtubule Polymerization Assays: These are direct functional assays that measure the effect of a compound on the dynamics of tubulin polymerization into microtubules in vitro. A stabilizer (e.g., paclitaxel) will increase polymerization, while a destabilizer (e.g., vinca alkaloids) will inhibit it [1] [11].
- ATPase Activity Assays: For motor proteins like kinesins and myosins, measuring the compound's effect on their microtubule- or actin-stimulated ATPase activity is a key functional readout [1].
- Cell-Based Phenotypic Assays: These assess the downstream cellular consequences of target engagement. Examples include:
- Cell Cycle Analysis: Many microtubule-targeting agents cause mitotic arrest, which can be quantified by flow cytometry.
- Immunofluorescence Microscopy: Visualizing the microtubule network, mitotic spindle formation, or chromosome alignment can reveal profound functional impacts of compound treatment [11].
Integrating CETSA with these functional assays creates a powerful workflow: CETSA confirms the compound binds the target in cells, and the functional assays demonstrate that this binding leads to the intended mechanistic and phenotypic effect [103].
AI-Powered Bioactivity Prediction from Morphological Profiles
Frequently Asked Questions (FAQs)
Q1: What is the core principle behind using AI for bioactivity prediction from morphological profiles? A1: AI-powered bioactivity prediction uses deep learning models to analyze high-content cellular images (like Cell Painting assays) and extract complex morphological features. These features form a "fingerprint" that captures the cell's state after a chemical or genetic perturbation. The AI model learns the correlation between these morphological profiles and specific bioactivity outcomes, such as a compound's mechanism of action (MoA) or its efficacy in inhibiting cancer cell proliferation (e.g., GI50%), enabling the prediction of bioactivity for new compounds directly from their imaging data [104] [105] [106].
Q2: Why is Cell Painting a preferred assay for this application in cytoskeletal research? A2: Cell Painting is a multiplexed assay that uses up to five fluorescent dyes to stain multiple cellular compartments, including the cytoskeleton (e.g., actin filaments), nucleus, and mitochondria. It is target-agnostic, making it ideal for discovering compounds with novel mechanisms of action, which is crucial when probing cytoskeletal targets. The rich morphological data it generates can reveal subtle, cytoskeleton-driven phenotypic changes induced by compounds, such as alterations in cell shape, cytoskeletal architecture, and organelle arrangement, which might be missed by target-specific assays [104] [106].
Q3: We are encountering high variability in bioactivity predictions when testing compounds targeting tubulin. What could be the cause? A3: High variability can stem from several sources:
- Assay Conditions: Inconsistent tubulin polymerization conditions (e.g., temperature, GTP concentration) can lead to varying results [1].
- Image Analysis Workflow: Traditional feature extraction tools (e.g., CellProfiler) can be sensitive to segmentation parameters, especially with cytoskeletal structures that may appear different after tubulin perturbation. Inconsistent segmentation directly impacts feature quality [106].
- Biological Replicates: An insufficient number of biological replicates may fail to capture natural biological variation. For cytoskeletal targets, it is critical to account for cell cycle-dependent morphological changes.
Q4: How can self-supervised learning (SSL) improve the analysis of Cell Painting images in our cytoskeletal drug screens? A4: SSL models, such as DINO, are trained directly on Cell Painting images without the need for manual annotations. This provides key advantages:
- Segmentation-Free Analysis: SSL eliminates the need for error-prone cell segmentation, simplifying the workflow and reducing a major source of variability [106].
- Computational Efficiency: Feature extraction with a pre-trained SSL model is significantly faster than running a full CellProfiler pipeline [106].
- Powerful Representations: SSL features have been shown to match or exceed the performance of CellProfiler features in tasks like target identification and gene family classification, capturing biologically relevant morphological nuances critical for assessing cytoskeletal drug effects [106].
Q5: Can AI models predict a compound's Mechanism of Action (MoA) from morphological profiles? A5: Yes. By comparing the morphological profile induced by a new compound to a reference database of profiles from compounds with known MoAs, AI models can infer the likely MoA through a "guilt-by-association" principle. This is particularly powerful for identifying whether a new compound affects well-established cytoskeletal pathways or possesses a novel mechanism [104].
Q6: What are the common pitfalls in model generalization when applying a pre-trained model to a new set of compounds? A6: The main pitfalls include:
- Domain Shift: The new compounds or cell lines may induce morphological features not well-represented in the model's original training data.
- Batch Effects: Technical variations between experimental batches (e.g., in staining intensity) can degrade model performance if not properly corrected.
- Cell Line Specificity: A model trained on one cell type (e.g., U2OS) may not generalize well to another (e.g., a DLBCL model) due to inherent morphological differences [106] [75]. It is crucial to validate the model on a small, representative set from your new experimental domain before full deployment.
Troubleshooting Guides
Issue 1: Poor Performance in Predicting Cytoskeletal-Target Bioactivity
Symptoms:
- Low accuracy, precision, or recall in predicting the bioactivity of compounds known to target cytoskeletal proteins like tubulin or kinesins.
- Model fails to distinguish between active and inactive compounds in validation screens.
Diagnosis and Resolution:
| Step | Action | Rationale & Technical Details |
|---|---|---|
| 1 | Verify Assay Quality | Confirm that control compounds (e.g., known tubulin polymerizers) produce the expected strong phenotypic signal and that the Z'-factor of your HCS assay is >0.5, indicating a robust assay [1]. |
| 2 | Inspect Feature Quality | If using hand-crafted features, check for high correlation and redundancy. For deep learning features, use techniques like UMAP to visualize if profiles from active compounds cluster separately from inactives. |
| 3 | Augment Training Data | If labeled data is scarce, use self-supervised learning (SSL) to pre-train your model on all available unlabeled Cell Painting images. This allows the model to learn generalizable morphological features before fine-tuning on your specific bioactivity task [106]. |
| 4 | Employ Ensemble Models | Combine predictions from multiple models (e.g., Graph Neural Networks and Transformer-based models) to improve robustness and accuracy. Research has shown that ensemble methods can achieve high Pearson correlation coefficients (up to 83%) in predicting anticancer bioactivity [105] [107]. |
Issue 2: High Computational Cost and Slow Feature Extraction
Symptoms:
- Feature extraction from Cell Painting images takes days or weeks.
- Inability to rapidly screen large virtual compound libraries.
Diagnosis and Resolution:
| Step | Action | Rationale & Technical Details |
|---|---|---|
| 1 | Adopt a Segmentation-Free Workflow | Replace traditional software like CellProfiler with a pre-trained SSL model (e.g., DINO) for feature extraction. This bypasses the computationally intensive segmentation step [106]. |
| 2 | Implement Virtual Screening | Use the AI model to predict the morphological profiles and bioactivity of compounds in silico before synthesizing or purchasing them. This dramatically reduces wet-lab costs and time by prioritizing only the most promising candidates [104] [108]. |
| 3 | Optimize Hardware | Utilize GPUs for both model training and inference. The parallel processing power of GPUs is essential for efficient handling of large image datasets and complex deep learning models. |
Experimental Protocols & Data
Protocol 1: Generating a Morphological Profile for a Compound
This protocol details the steps to process raw Cell Painting images into a quantitative morphological profile for bioactivity prediction.
Workflow Description: The diagram below illustrates the two primary computational paths for generating morphological profiles from raw Cell Painting images: the traditional CellProfiler-based pipeline and the modern self-supervised learning (SSL) approach.
Methodology:
- Image Acquisition: Acquire high-content images from a Cell Painting assay after treating cells with the compound of interest. Include appropriate controls (e.g., DMSO vehicle and known bioactive compounds).
- Feature Extraction (Choose one path):
- Traditional Path (CellProfiler):
- Use CellProfiler with a standardized pipeline (e.g., the CellPainting pipeline from GitHub) to segment individual cells and identify organelles [106].
- Extract hundreds of hand-crafted morphological features (e.g., area, shape, texture, intensity) for every single cell.
- SSL Path (Segmentation-Free):
- Input raw image crops (ensuring they contain cells) directly into a pre-trained SSL model like DINO [106].
- The model outputs a high-dimensional feature vector (embedding) that represents the morphological content of the image crop.
- Traditional Path (CellProfiler):
- Profile Aggregation: For both paths, aggregate the single-cell or single-crop features by computing the median (or mean) across all cells/crops from the same treatment well to create a single, robust morphological profile per compound perturbation [106].
Protocol 2: Building a Bioactivity Prediction Model
This protocol outlines the steps to train a model that predicts bioactivity from morphological profiles.
Workflow Description: This diagram outlines the machine learning workflow for training and applying a bioactivity prediction model, from data preparation to model deployment for virtual screening.
Methodology:
- Data Preparation: Compile a dataset where the inputs are morphological profiles and the targets are corresponding bioactivity measurements (e.g., GI50% values from growth inhibition assays) [105]. Split the data into training, validation, and test sets.
- Feature Processing: Apply dimensionality reduction techniques (e.g., PCA, UMAP) or feature selection to reduce noise and computational load.
- Model Training: Train a machine learning model on the training set. Consider using:
- Validation: Use the validation set for hyperparameter tuning and to avoid overfitting. The test set, used only once, provides an unbiased evaluation of the model's performance.
- Deployment: Use the trained model to predict the bioactivity of new compounds from their morphological profiles, enabling virtual screening and hit prioritization [104].
The following table summarizes key performance metrics from recent studies relevant to AI-powered bioactivity and morphological profiling.
Table 1: Performance Metrics of AI Models in Drug Discovery Tasks
| Model / Platform | Task | Key Metric | Performance | Reference / Context |
|---|---|---|---|---|
| Ardigen phenAID | Hit Identification in Phenotypic Screening | Accuracy Improvement | Up to 40% more accurate hits compared to traditional methods [104] | |
| Multi-Model Ensemble (GCN, GAT, MPNN, ChemBERTa) | Anticancer Bioactivity (GI50%) Prediction | Pearson Correlation Coefficient | Up to 83% (Stacking Ensemble) [105] [107] | Breast cancer tumor cell lines [105] |
| DINO (SSL) | Drug Target Classification | Performance vs. CellProfiler | Surpassed CellProfiler in accuracy [106] | JUMP-CP Dataset [106] |
| DINO (SSL) | Computational Efficiency | Processing Time | Significant reduction vs. CellProfiler pipeline [106] | JUMP-CP Dataset [106] |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Tools for Cytoskeletal-Focused Morphological Profiling
| Item | Function in Research | Example Application in Context |
|---|---|---|
| Cell Painting Assay Kits | Provides a standardized set of fluorescent dyes to stain the nucleus, cytoplasm, cytoskeleton (actin), mitochondria, and Golgi apparatus. | Generating multiplexed morphological data for untreated and compound-treated cells [104] [106]. |
| Validated Cytoskeletal Target Compounds | Well-characterized small molecules used as positive and negative controls in screening assays. | Using tubulin polymerizers (e.g., Paclitaxel) or kinesin inhibitors (e.g., KIF18A inhibitors) to validate the assay and model's ability to detect known phenotypes [1]. |
| Specialized CRO Services | Provides expert compound screening on specific protein targets with validated biochemical and cell-based assays. | Off-target counter-screening to confirm compound specificity (e.g., testing KIF18A inhibitors against a panel of other kinesins) [1]. |
| Public Morphological Datasets | Large-scale, publicly available image sets used for training and benchmarking AI models. | Using the JUMP-Cell Painting dataset (containing ~117,000 chemical perturbations) to pre-train self-supervised learning models [104] [106]. |
In vivo target validation is a critical step in the drug discovery pipeline, providing essential proof-of-concept data before candidates advance to clinical trials. It involves modulating a therapeutic target within a living organism to confirm its role in a disease process and assess the efficacy of therapeutic interventions [110] [111]. Unlike in vitro studies, in vivo models offer the superior advantage of capturing the complex physiology of a whole organism, including multiple gene cooperation within pathways, systemic effects, and off-target interactions [111]. This process significantly de-risks later-stage clinical development by ensuring that resources are focused on targets with demonstrated therapeutic potential [110]. Within cytoskeletal drug target research, this is particularly relevant, as targets such as tubulin, kinesins, and related signaling proteins like PAK2 are implicated in diseases ranging from cancer to neurodegenerative conditions [1] [98]. This technical support center provides troubleshooting guides and detailed protocols to help researchers navigate the specific challenges of in vivo validation within this field.
Frequently Asked Questions (FAQs) and Troubleshooting
Q1: Our lead compound shows high potency in cell-based assays but fails to demonstrate efficacy in a mouse model of ALS. What could be the cause?
This is a common translational challenge. The primary issues to investigate are:
- Brain Penetrance: A compound must reach its target site in the brain to be effective. You must provide data demonstrating that your compound crosses the blood-brain barrier at the planned dose [112]. If brain penetrance is low, consider formulating the compound to improve its bioavailability or exploring alternative delivery methods.
- Disease Model Relevance: Ensure your animal model appropriately recapitulates the human disease pathology. For ALS research, the slower-progressing TDP-43 "Low Dox" mouse model, for example, may offer a more therapeutically relevant time window for intervention than the original, faster-progressing version [112]. Confirm that your model exhibits key phenotypes like cytoplasmic TDP-43 mislocalization, neurodegeneration, and motor deficits that your compound is designed to modulate.
- Target Engagement: Confirm that your compound is effectively engaging the intended target in vivo. This may require developing specific assays to measure the compound's effect on its target, such as a reduction in phosphorylated protein levels.
Q2: During a counter-screen for a novel anti-kinesin compound, we detected unexpected off-target activity. How should we proceed?
Unexpected off-target activity is a critical finding that must be thoroughly investigated to ensure compound specificity and safety.
- Comprehensive Motor Panel Screening: To assess specificity, subject your compound to a panel of related and unrelated kinesins. A validated approach, as used in industry, is to screen against a motor panel including KIF2, KIF3C, KIFC3, KIF4A, KIF10(CENPE), KIF11(Eg5), KIF20A, and KIF23 [1]. This will quantify the IC₅₀ for your primary target versus off-targets.
- Data Interpretation: If the off-target activity is against a closely related homolog (e.g., KIF18A vs. KIF18B/KIF19A), it may be acceptable depending on the therapeutic context. However, activity against distantly related kinesins with critical cellular functions is a major red flag [1]. This data should be used to inform further medicinal chemistry efforts for lead optimization and to refine the compound's structure-activity relationship (SAR).
Q3: We are using digital measures of animal behavior (e.g., home cage monitoring). How can we validate that these digital outputs are biologically meaningful?
The adoption of in vivo digital measures requires a structured validation framework to ensure reliability and relevance.
- Apply the In Vivo V3 Framework: This framework, adapted from clinical digital medicine, is the standard for building confidence in digital measures [113].
- Verification: Ensure the digital sensors (e.g., cameras, photobeams) are accurately capturing and storing raw data in your specific laboratory environment.
- Analytical Validation: Confirm that the algorithms processing the raw data (e.g., to generate "centimeters traveled per second") are precise and accurate.
- Clinical (Biological) Validation: Correlate the digital measure with established biological or functional states in the animal model. For example, a digital measure of "reduced locomotion" should correlate with a traditional manual score of motor impairment [113].
- Robust Metadata: Consistently record comprehensive metadata (animal ID, treatment, dosage, time, environmental conditions) to provide essential context for interpreting digital data and ensuring reproducibility [113].
Q4: Our in vivo study yielded high variability in the treatment response. What are the key factors to control?
High variability can obscure true treatment effects. Key factors to standardize include:
- Animal Model Parameters: Strictly control the genetic background, age, and gender of the animals. For inducible models, ensure the dosing regimen (e.g., doxycycline diet) is perfectly consistent across all animals [112] [111].
- Housing and Handling: Factors such as diet, housing conditions, microbial status, and routine handling can significantly impact animal physiology and behavior, thereby influencing study outcomes. These must be standardized as much as possible [111].
- Pharmacokinetics: Understand the absorption, distribution, metabolism, and excretion (ADME) of your compound to ensure consistent exposure across the study cohort.
Key Experimental Protocols
Protocol for In Vivo Validation of a Cytoskeletal Target in a Neurodegenerative Model
This protocol outlines the key steps for validating a therapeutic target in a mouse model of amyotrophic lateral sclerosis (ALS), a common approach applicable to other neurodegenerative diseases.
1. Objective: To evaluate the effect of modulating a candidate therapeutic target on disease phenotypes in a TDP-43 mouse model of ALS [112].
2. Materials:
- Animal Model: TDP-43 rNLS8 (or ΔNLS) mice on a doxycycline (Dox)-controlled diet ("Low Dox" model for slower progression) [112].
- Test Article: The compound (e.g., small molecule, antisense oligonucleotide) provided by the investigator. Brain penetrance data must be available [112].
- Equipment: In vivo anatomical MRI, CT imager for hindlimb muscle atrophy, electrophysiology apparatus for compound muscle action potential (CMAP), equipment for immunohistochemistry (IHC).
3. Methodology:
- Study Design:
- Grouping: Assign a maximum of 45 mice to prophylactic or interventional treatment groups and appropriate controls.
- Dosing: Administer the test article for up to 8 weeks. In an interventional design, dosing begins after disease phenotypes have started to manifest.
- Endpoint Measurements: Conduct longitudinal and terminal readouts [112].
- Clinical Measures:
- Monitor body weight twice weekly.
- Assess motor function using standardized scoring, including grip strength tests.
- Perform in vivo Anatomical MRI.
- Conduct longitudinal CT imaging to quantify hindlimb muscle atrophy.
- Measure gastrocnemius muscle electrophysiology (CMAP).
- Tissue Analysis:
- Perform IHC on brain and spinal cord tissue for key markers: human TDP-43, pathological pTDP-43 (p409/410), and GFAP (for reactive astrocytes).
- Collect frozen tissue and terminal fluids for subsequent biochemical analysis by the investigator.
- Clinical Measures:
4. Data Analysis: Compare all clinical and histological endpoints between treatment and control groups using appropriate statistical tests (e.g., t-tests, ANOVA for multiple groups) to determine if target modulation significantly alters disease progression and pathology.
Protocol for Specificity Screening of a Kinesin Inhibitor
This protocol is essential for confirming that a compound targeting a kinesin (e.g., KIF18A) does not adversely affect other essential motor proteins.
1. Objective: To evaluate the specificity of anti-kinesin drug candidates by profiling them against a panel of kinesin motors [1].
2. Materials:
- Proteins: Purified recombinant kinesin proteins, including the primary target (e.g., KIF18A) and off-target kinesins (KIF2, KIF3C, KIFC3, KIF4A, KIF10, KIF11, KIF20A, KIF23) [1].
- Assay Reagents: ATP, microtubules, buffer components for a microtubule-activated ATPase assay.
- Equipment: Plate reader for colorimetric/fluorometric detection.
3. Methodology:
- Assay Principle: Measure the compound's effect on the microtubule-stimulated ATPase activity of each kinesin. Inhibition reduces ATP hydrolysis.
- Procedure:
- Incubate each kinesin protein with a range of compound concentrations in the presence of microtubules and ATP.
- Quantify the amount of ADP produced over time using a coupled enzymatic reaction or colorimetric assay.
- Run controls (vehicle and known inhibitors) in parallel.
- Data Analysis:
- Calculate the remaining ATPase activity for each compound concentration.
- Plot dose-response curves and determine the half-maximal inhibitory concentration (IC₅₀) for each kinesin in the panel.
- A highly specific compound will show a significantly lower IC₅₀ (higher potency) for its primary target compared to all other kinesins.
Workflow and Pathway Visualization
In Vivo Target Validation Workflow
The following diagram illustrates the integrated stages of in vivo target validation, highlighting the critical role of troubleshooting and iterative learning.
In Vivo V3 Framework for Digital Measures
This diagram outlines the validation framework for ensuring the reliability of digital measures collected in vivo, such as home-cage monitoring data.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents and tools essential for conducting in vivo validation experiments, particularly for cytoskeletal targets.
Table: Essential Research Reagents for Cytoskeletal Target Validation
| Reagent/Tool | Function/Application | Example Use-Case |
|---|---|---|
| Tubulin Polymerization Assays [1] | Measures compound effect on microtubule dynamics. | In vitro profiling of compounds targeting tubulin for cancer, gout, or arthritis. |
| Kinesin ATPase Assays [1] | Quantifies inhibition of kinesin motor activity. | Specificity screening against kinesin panels (e.g., KIF18A) to identify selective inhibitors. |
| PAK2 In Silico Screening Library [98] [114] | Library of FDA-approved compounds for virtual docking. | Identifying drug repurposing candidates for PAK2 inhibition in cancer. |
| TDP-43 Mouse Model [112] | Models ALS pathology with TDP-43 mislocalization. | Evaluating therapeutic efficacy on neurodegeneration and motor deficits. |
| Conditional Gene Expression/RNAi [111] | Enables target modulation after disease establishment. | Mimicking therapeutic intervention in vivo to validate target role in disease. |
Quantitative Endpoints for ALS In Vivo Studies
Table: Key Longitudinal and Terminal Readouts for Preclinical ALS Studies [112]
| Measure Category | Specific Readout | Data Type | Significance |
|---|---|---|---|
| Clinical Phenotyping | Body Weight | Quantitative (grams) | General health indicator |
| Motor Score / Grip Strength | Quantitative (score/force) | Direct measure of motor function | |
| In Vivo Imaging | Anatomical MRI (Brain/Spinal Cord) | Volumetric & Structural | Assesses neurodegeneration |
| CT of Hindlimb Muscles | Cross-sectional area | Quantifies muscle atrophy | |
| Electrophysiology | Compound Muscle Action Potential (CMAP) | Amplitude (mV) | Measures neuromuscular integrity |
| Histopathology | IHC: TDP-43 Mislocalization | Semi-quantitative (score) | Confirms target pathology |
| IHC: pTDP-43 | Semi-quantitative (score) | Measures pathological protein form | |
| IHC: GFAP (Astrocytes) | Semi-quantitative (score) | Indicates neuroinflammation |
Kinesin Inhibitor Specificity Profile
Table: Example Specificity Data for a KIF18A Inhibitor from a Motor Panel Screen [1]
| Kinesin Target | IC₅₀ (nM) | Selectivity Fold-Change (vs. KIF18A) | Interpretation |
|---|---|---|---|
| KIF18A | 15 | 1.0 (Reference) | Primary target; highly potent. |
| KIF18B | 42 | 2.8 | Close homolog; acceptable cross-reactivity. |
| KIF19A | 110 | 7.3 | Close homolog; acceptable cross-reactivity. |
| KIF11 (Eg5) | >10,000 | >666 | Distant kinesin; excellent specificity. |
| KIF4A | >10,000 | >666 | Distant kinesin; excellent specificity. |
| KIF23 | >10,000 | >666 | Distant kinesin; excellent specificity. |
Conclusion
The field of cytoskeletal drug target screening is undergoing rapid transformation, moving beyond traditional microtubule-targeting agents to explore novel binding sites and underutilized cytoskeletal components. The integration of advanced screening platforms—including organoid models, high-content phenotypic profiling, and AI-powered image analysis—is significantly enhancing the predictive value of early-stage screening campaigns. Successful development of next-generation cytoskeletal therapeutics will depend on effectively addressing key challenges in target specificity, toxicity mitigation, and clinical translation. Future directions will likely focus on leveraging multidimensional data integration, expanding the druggable cytoskeletal genome, and developing more physiologically relevant screening systems that better predict clinical efficacy, ultimately enabling the discovery of safer, more effective cytoskeletal-targeted therapies for cancer and other human diseases.
References
- 1. Compound Screening Services [https://www.cytoskeleton.com/services/compound-screening]
- 2. Septin filament coalignment with microtubules depends on ... [https://www.nature.com/articles/s41419-019-1318-6]
- 3. Septins mediate a microtubule–actin crosstalk that enables ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9897426/]
- 4. Cellular functions of actin- and microtubule-associated septins [https://pmc.ncbi.nlm.nih.gov/articles/PMC8194058/]
- 5. Cytoskeleton [https://en.wikipedia.org/wiki/Cytoskeleton]
- 6. The Cytoskeleton – Fundamentals of Cell Biology [https://open.oregonstate.education/cellbiology/chapter/cytoskeleton/]
- 7. Microtubule Targeting Agents in Disease: Classic Drugs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8616087/]
- 8. Recent Approaches to the Identification of Novel ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2022.841777/full]
- 9. Recent Advances in Microtubule Targeting Agents for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388312/]
- 10. 19 Approved ADCs Worldwide: The Ultimate Guide (Updated ... [https://us.huatengsci.com/news/show/1719.html]
- 11. The microtubule cytoskeleton: An old validated target for novel ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9521402/]
- 12. Multiple Myeloma Drugs: Types, Classes & Treatments [https://www.myeloma.org/multiple-myeloma-drugs]
- 13. October 2025: Notable Drug Approvals [https://www.dermatologyadvisor.com/news/october-2025-notable-drug-approvals/]
- 14. Learn about Compound Screening [https://www.bosterbio.com/blog/post/learn-about-compound-screening?srsltid=AfmBOoqPXYYK9fGXJGP0D6C3gDT87J0YLO68q36FxUw0wjGVPnAiknfG]
- 15. Molecular interactions at the colchicine binding site in tubulin [https://pmc.ncbi.nlm.nih.gov/articles/PMC8901563/]
- 16. Structures of a diverse set of colchicine binding site ... [https://pubmed.ncbi.nlm.nih.gov/26462166/]
- 17. Maitansine [https://en.wikipedia.org/wiki/Maitansine]
- 18. New insights into the anticancer therapeutic potential of ... [https://www.sciencedirect.com/science/article/pii/S0753332223008296]
- 19. Insights into the distinct mechanisms of action of taxane and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5325780/]
- 20. Insights into the Distinct Mechanisms of Action of Taxane ... [https://www.sciencedirect.com/science/article/pii/S0022283617300153]
- 21. - PMC Vinca Alkaloids [https://pmc.ncbi.nlm.nih.gov/articles/PMC3883245/]
- 22. Structural insight into the stabilization of microtubules by ... [https://elifesciences.org/articles/84791]
- 23. Recent Advances in Microtubule Targeting Agents for ... [https://www.mdpi.com/1420-3049/30/16/3314]
- 24. Role of the cytoskeleton in cellular reprogramming [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1538806/full]
- 25. Interplay Between the Cytoskeleton and DNA Damage ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025774/]
- 26. Targeting the cytoskeleton as a therapeutic approach to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11034636/]
- 27. Cytoskeletal dynamics: A view from the membrane - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4427793/]
- 28. Cell Division and Cytoskeleton - Research [https://www.cancer.dk/danish-cancer-institute/research-groups/cell-division-and-cytoskeleton/]
- 29. Cytoskeleton Structure | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cell-structure/cytoskeleton.html]
- 30. High-throughput screening of FDA-approved drugs ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra01341k]
- 31. Microtubule-Targeting Agents: Advances in Tubulin ... [https://www.mdpi.com/1422-0067/26/15/7652]
- 32. Cytoskeletal targets of natural products - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7797185/]
- 33. Frontiers | The microtubule cytoskeleton: An old validated target for... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2022.969183/full]
- 34. Discovering New Drug Using High-Throughput Targets Screening [https://www.news-medical.net/whitepaper/20180815/Discovering-New-Drug-Targets-Using-High-Throughput-Screening.aspx]
- 35. AD中的Tau蛋白病变:MARK-4的治疗潜力 [https://eurekaselect.com/public/article/146523/cn]
- 36. Targeting CDKs in cancer therapy: advances in PROTACs ... [https://www.nature.com/articles/s41698-025-00931-8]
- 37. 微囊藻毒素与疾病 [http://swyxzh.ijournals.cn/swyxzh/article/html/20250205?st=article_issue]
- 38. integrity as a Cytoskeletal drug target [https://pubmed.ncbi.nlm.nih.gov/15974922/]
- 39. Tubulin Polymerization Assay - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/tubulin-polymerization-assay]
- 40. Tubulin Polymerization Assay Services [https://www.cytoskeleton.com/services/compound-screening/tubulin-polymerization-assay-services]
- 41. NanoDSF Screening for Anti-tubulin Agents Uncovers New ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406199/]
- 42. Tubulin polymerization assay using >99% pure tubulin [https://www.cytoskeleton.com/bk011p]
- 43. S-72, a Novel Orally Available Tubulin Inhibitor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10221130/]
- 44. Competitive Binding Assay - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/competitive-binding-assay]
- 45. Thermal shift assays in drug discovery [https://www.sciencedirect.com/science/article/abs/pii/S1056871925008007]
- 46. Assay setup for competitive binding measurements [https://support.nanotempertech.com/hc/en-us/articles/18014451138833-Assay-setup-for-competitive-binding-measurements]
- 47. The Art of Finding the Right Drug Target: Emerging Methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11334170/]
- 48. Compound Screening [https://www.cytoskeleton.com/custom-services/compound-screening]
- 49. Cell Painting, a high-content image-based assay for ... [https://www.nature.com/articles/nprot.2016.105]
- 50. Cell Painting, a high-content image-based assay for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5223290/]
- 51. Morphological Profiling Identifies a Common Mode of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7754162/]
- 52. Cytoskeleton-focused Screening Compound Library [https://lifechemicals.com/screening-libraries/targeted-and-focused-screening-libraries/cytoskeleton-focused-screening-compound-library]
- 53. Optimizing the Cell Painting assay for image-based profiling [https://www.nature.com/articles/s41596-023-00840-9]
- 54. Cell Painting High-Content Image Assay [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cell-structure/cell-painting-assay.html]
- 55. Ultimate IHC Troubleshooting Guide: Fix Weak Staining & ... [https://www.atlasantibodies.com/knowledge-hub/blog/the-ultimate-ihc-troubleshooting-guide-from-weak-staining-to-high-background/]
- 56. IHC Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/ihc-troubleshooting-guide.html]
- 57. Organoid FAQs - your questions answered [https://cancertools.org/resources/faqs/organoids/]
- 58. A Technical FAQ Guide to Oncology Drug Screening Using ... [https://blog.crownbio.com/oncology-drug-screening-using-innovative-organoid-technology-and-biomarker-analysis]
- 59. Advancements, Strategies, and Challenges in Organoid ... [https://www.sciencedirect.com/science/article/pii/S2095809925006083]
- 60. A Practical Guide to Developing and Troubleshooting Patient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566426/]
- 61. Organoid-Based Phenotypic Screening [https://drugscreening.bocsci.com/services/organoid-based-phenotypic-screening.html]
- 62. Organoid High-Throughput Phenotypic Screening Services [https://www.innoserlaboratories.com/oncology-cro-services/organoid-high-throughput-screening-services/]
- 63. Mass Cytometry Protocol & Troubleshooting - Creative Biolabs [https://www.creativebiolabs.net/mass-cytometry.htm]
- 64. Faq's - Cytof Mass Cytometry Boston [https://masscytometryboston.com/faqs/]
- 65. Multidimensional profiling of drug‐treated cells by Imaging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6722888/]
- 66. Review Highly multiparametric analysis by mass cytometry [https://www.sciencedirect.com/science/article/abs/pii/S0022175910001985]
- 67. Measuring expression heterogeneity of single-cell ... [https://www.nature.com/articles/s41467-021-25212-3]
- 68. Chemical biology approaches targeting the actin ... [https://www.sciencedirect.com/science/article/abs/pii/S1367593118301789]
- 69. A novel class of anticancer compounds targets the actin ... [https://pubmed.ncbi.nlm.nih.gov/23946473/]
- 70. Drug Targeting the Actin Cytoskeleton Potentiates ... [https://pubmed.ncbi.nlm.nih.gov/32269073/]
- 71. The Potential for Targeting AVIL and Other Actin-Binding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10531751/]
- 72. Actin stabilizing compounds show specific biological effects ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6611809/]
- 73. Actin stabilizing compounds show specific biological ... [https://www.nature.com/articles/s41598-019-46282-w]
- 74. Targeting the actin cytoskeleton: selective antitumor action ... [https://www.nature.com/articles/cddis2014363]
- 75. Cytoskeletal dynamics and mitochondrial rearrangements ... [https://www.nature.com/articles/s41408-025-01358-x]
- 76. Structure based drug design and machine learning ... [https://www.nature.com/articles/s41598-025-17708-5]
- 77. Discovery of novel microtubule destabilizing agents via ... [https://www.sciencedirect.com/science/article/abs/pii/S0169260725004146]
- 78. Discovery of a novel microtubule destabilizing agent ... [https://www.sciencedirect.com/science/article/abs/pii/S0006295225000668]
- 79. Accessibility of the unstructured α-tubulin C-terminal tail is ... [https://elifesciences.org/reviewed-preprints/109308]
- 80. Structural changes of tubulin by interacting with Δ9- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12312531/]
- 81. Enhancing pre-clinical research with simplified intestinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10916479/]
- 82. Flow Cytometry Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/flow-cytometry-troubleshooting-guide?srsltid=AfmBOorWMNaWJQUXzMf9G33teuAfetCssAO98OL8W3DDuSh-BElfnrvS]
- 83. Flow Cytometry Troubleshooting Guide [https://www.novusbio.com/support/support-by-application/flow-cytometry/troubleshooting?srsltid=AfmBOoqXqiK6Zvu7IanX_YcyzK_EbaV_SeIxhmQwwsKOGrIv41cTubuP]
- 84. Challenges in 3D Live Cell Imaging [https://www.mdpi.com/2304-6732/8/7/275]
- 85. Image Deconvolution 101: Guide to Crisp Microscopy [https://www.thermofisher.com/blog/life-in-the-lab/deconvolution-101/]
- 86. 3D Confocal Imaging of Thick Samples Using Z Intensity ... [https://www.microscope.healthcare.nikon.com/resources/application-notes/3d-confocal-imaging-of-thick-samples-using-z-intensity-correction]
- 87. How to Troubleshoot and Improve Your 3D Simulations [https://www.linkedin.com/advice/0/what-do-you-your-3d-simulation-software-fvkre]
- 88. Three-dimensional imaging and quantitative analysis in ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6449377/]
- 89. Machine learning-assisted high-content imaging analysis ... [https://www.nature.com/articles/s41598-024-53323-6]
- 90. Target deconvolution techniques in modern phenotypic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3594516/]
- 91. The Deconvolution Revolution: Strategies for Target ... [https://momentum.bio/content/the-deconvolution-revolution-strategies-for-target-identification/]
- 92. A data-driven journey using results from target-based drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12062751/]
- 93. A novel approach for target deconvolution from phenotype ... [https://www.nature.com/articles/s41598-025-86166-w]
- 94. What Are the Types of Biochemical Assays Used in Drug ... [https://synapse.patsnap.com/article/what-are-the-types-of-biochemical-assays-used-in-drug-discovery]
- 95. Current Screening Methodologies in Drug Discovery for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6117650/]
- 96. Improving phenotypic screening | Nature Chemical Biology [https://www.nature.com/articles/s41589-025-02093-x]
- 97. 07 2023 06 赵扬团队报道用于高通量多基因表达谱检测的表 ... [https://future.pku.edu.cn/xwyjz/xw/99e9ffb2da0d4096beddb3c1cec18252.htm]
- 98. Exploring drug repurposing for PAK2 inhibition [https://pubmed.ncbi.nlm.nih.gov/41021189/]
- 99. A precise comparison of molecular target prediction methods [https://pubs.rsc.org/en/content/articlehtml/2025/dd/d5dd00199d]
- 100. CETSA [https://www.cetsa.org/]
- 101. CETSA-Guided Medicinal Chemistry and Lead Generation [https://pmc.ncbi.nlm.nih.gov/articles/PMC6511951/]
- 102. Applications of the Cellular Thermal Shift Assay to Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12072176/]
- 103. Functional assays [https://www.pelagobio.com/drug-discovery-services/lead-generation/functional-assays/]
- 104. Phenotypic Screening AI & Morphological | Ardigen Profiling [https://ardigen.com/phenotypic-profiling-ardigen-phenaid/]
- 105. AI-Driven molecule generation and bioactivity prediction: A ... [https://www.sciencedirect.com/science/article/abs/pii/S1476927125001926]
- 106. Self-supervision advances morphological by unlocking... profiling [https://www.nature.com/articles/s41598-025-88825-4?error=cookies_not_supported&code=3a8fa1a6-41f8-4df9-8661-e27c0e569366]
- 107. AI-Driven molecule generation and bioactivity prediction [https://pubmed.ncbi.nlm.nih.gov/40550191/]
- 108. a systematic virtual screening of FDA-approved drugs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12480294/]
- 109. Recent advances in molecular representation methods and ... [https://www.nature.com/articles/s44386-025-00017-2]
- 110. In Vivo Target Validation Using Biological Molecules ... [https://pubmed.ncbi.nlm.nih.gov/26552401/]
- 111. In Vivo Target Validation [https://www.creative-biolabs.com/drug-discovery/therapeutics/in-vivo-target-validation.htm]
- 112. In Vivo Target Validation [https://www.targetals.org/in-vivo-target-validation-2025/]
- 113. Validation framework for in vivo digital measures [https://www.frontiersin.org/journals/toxicology/articles/10.3389/ftox.2024.1484895/full]
- 114. a systematic virtual screening of FDA-approved drugs ... [https://link.springer.com/article/10.1007/s12672-025-03516-w]